Translate this page into:
Fractional Erbium YAG Laser Resurfacing Versus 20% Trichloroacetic Acid Chemical Peeling in the Treatment of Acne Scars: A Comparative Study
Address for correspondence: Dr. Bhikam Chand Ghiya, Department of Skin and VD, Sardar Patel Medical College, Bikaner 334001, Rajasthan, India. E-mail: bcghiya@yahoo.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Acne scarring not only affects the aesthetic appearance of an individual but also has a detrimental effect on mental health and social life. Various treatment modalities are available for acne scars.
Aim:
In this study, fractional erbium-doped yttrium–aluminum–garnet (Er:YAG) laser resurfacing was compared with 20% trichloroacetic acid (TCA) peeling in terms of efficacy and safety.
Materials and Methods:
This prospective comparative study included 50 subjects of acne scar who were randomly divided into Groups A and B, 25 patients in each group. Group A was treated with 4 sessions of fractional Er:YAG laser and Group B with 4 session of 20% TCA application as chemical peeling, repeated every 21 days over a period of 3 months. The patients were evaluated for improvement at each visit using Goodman and Baron’s qualitative and quantitative acne scar grading.
Results:
Statistically significant improvement in Goodman and Barron’s qualitative acne scar grades was observed in both groups. At the end of therapy, that is, after 12 weeks of therapy, the mean percentage reduction in Goodman and Baron’s quantitative acne scar scores was 21.69% ± 16% in Group A and 20.97% ± 8.70% in Group B. In regards of complications, both procedures were well tolerated.
Conclusion:
We concluded that fractional Er:YAG laser resurfacing and 20% TCA peel application in the treatment of atrophic acne scar are equally efficacious. Both procedures are safe and well tolerated by the patients.
Keywords
Acne scars
erbium YAG laser
TCA peel
INTRODUCTION
Acne is a common disorder affecting pilosebaceous units, clinically characterized by the presence of comedones, inflammatory papules, pustules, nodules, and cysts.[1] Studies suggest that about 95% of patients with acne suffer from mild-to-moderate scarring, while 30% experience severe scarring. The severity of scarring reflects with grade of acne.[2] Acne scars are classified as atrophic with net loss of collagen and hypertrophic or keloid with net gain of collagen. Atrophic scars are further divided into boxcar, ice pick, and rolling.[3]
Acne scarring not only affects the aesthetic appearance of an individual but also has a detrimental effect on mental health and social life.[4] Various treatment modalities are available for acne scars. Selection of treatment option varies from individual to individual. It depends mainly on affordability, efficacy, and safety of the chosen treatment. In this study, fractional erbium-doped yttrium–aluminum–garnet (Er:YAG) laser resurfacing was compared with 20% trichloroacetic acid (TCA) peeling in terms of efficacy and safety.[5]
MATERIAL AND METHODS
This prospective comparative study included 50 subjects of acne scar who were randomly divided into Groups A and B, 25 patients in each group. Group A was treated with four sessions of fractional Er:YAG laser and Group B with four sessions of 20% TCA application as chemical peeling, repeated every 21 days over a period of 3 months.
Patients aged between 18 and 45 years with Goodman and Baron’s acne scar grades 2–4 were included in the study. Pregnant and lactating females, immunocompromised patients, patients with active acne, any active skin infections, history of oral retinoids therapy in the past 1 month, keloidal and bleeding tendencies and unrealistic expectations from the outcome of the procedure were excluded from the study.
Acne scars were assessed in terms of number, size, depth, distensibility, area, and distribution. Grading was done based on Goodman and Baron’s acne scar grades and an individualized patient had multiplicity of scar types and grades.[67]
In Group A, topical anesthetic cream was applied under occlusion for 1 h. We used Er:YAG laser system 2940 nm (Quanta Q1 plus machine, DNA Laser Technology) in the study. Acne scars were treated with three passes of fractional Er:YAG laser having fluency of 20–25 J/cm2 and pulse duration 1 ms.
In Group B, preprocedural priming was done prior to TCA application. Commercially prepared 20% TCA was applied evenly over acne scar areas. The development of frosting was observed and considered as end point of treatment. Areas showing insignificant frosting were recoated, and the areas with discomfort and erythema were noted.
To minimize pain and erythema, the skin was washed with tap water immediately after frosting. Edema, erythema, and desquamation occurred in the postpeel phase and lasted 1–3 days. Patients were instructed to avoid peak sunshine and use broad-spectrum sunscreen and mild moisturizers until the peeling process was completed.
The patients were evaluated for improvement at each visit using Goodman and Baron’s qualitative[6] and quantitative[7] acne scar grading. Photographs of both sides of the face were taken under consistent background, position, and lighting. Pre- and posttreatment photographs were compared.
Induction of collagen synthesis can start at a minimum of 3 weeks to maximum of 8 weeks. Visible improvement in appearance can be appreciated at minimum of 3 weeks.[8] Our first assessment of response in acne scars was at 3 weeks so as to evaluate even the minimum possible improvement to the treatment. All the patients were subjected to subsequent sittings at interval of 3 weeks for assessment of superadded improvement.
The improvement was graded as poor, good, and excellent depending upon the change in grade of acne scars. An improvement by two grades or more was considered as excellent, one grade as good and no improvement as poor [Table 1].
| Goodman and Baron’s qualitative acne scar grading | ||||
|---|---|---|---|---|
| Grade 1 | Macular erythematous, hypo- or hyperpigmented scars | |||
| Grade 2 | Mild atrophy that is visible at a distance of less than 50 cm and can be covered by makeup or beard hair. Examples include rolling acne scars | |||
| Grade 3 | Moderate disease that is visible at 50 cm or greater; not easily covered with makeup or the normal shadow of a shaved beard hair. Stretching the skin can flatten the scar. Examples include more significant rolling scars, shallow boxcar scars, and mild-to-moderate hypertrophic scars | |||
| Grade 4 | Severe disease as in grade 3 but scarring is not flattened by stretching the skin. Examples include severe boxcar, ice pick scars, and hypertrophic/keloid scarring | |||
| Goodman and Baron’s quantitative acne scar grading | ||||
| Grades | No. of lesions | |||
| 1–10 | 11–20 | >20 | ||
| A | Macular or mildly atrophic | 1 patient | 2 patients | 3 patients |
| B | Moderately atrophic | 2 patients | 4 patients | 6 patients |
| C | Punched-out or linear-troughed severe scars | 3 patients | 6 patients | 9 patients |
| D | Hyperplastic papular scars | 2 patients | 4 patients | 6 patients |
| E | Hyperplastic keloidal or hypertrophic scars | Area <5 cm2—6 patients | Area 5–20 cm2—12 patients | Area >20 cm2—18 patients |
The statistical tests used were chi-square test and Fisher’s exact probability test used to assess the level of significance and P value. The P value was taken significant when less than 0.05 and a confidence interval of 95% was taken. Quantitative data were expressed as mean and standard deviation and qualitative data were expressed as percentage and proportions.
RESULTS
In Group A, 20 (80%) out of 25 patients were males and 5 (20%) out of 25 patients were females. Their age ranged between 18 and 38 years with mean age of 26.6 ± 5.72 years. In Group B, 14 (56%) out of 25 patients were males and 11 (44%) out of 25 patients were females. Their age ranged between 18 and 38 years with mean age of 27.68 ± 6.50 years.
In both groups, gradual improvement in Goodman and Baron’s qualitative and quantitative acne scar grading was noted every 3rd week over a period of 12 weeks [Tables 2 and 3].
| Duration of therapy | Total number of patients | Number of patients with acne scar Grade 1 | Number of patients with acne scar Grade 2 | Number of patients with acne scar Grade 3 | Number of patients with acne scar Grade 4 | P value (difference from baseline) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | Group A | Group B | |
| Baseline | 25 | 25 | 0 | 0 | 1 | 1 | 4 | 6 | 20 | 18 | ||
| 3 weeks | 25 | 25 | 0 | 0 | 1 | 1 | 7 | 9 | 17 | 15 | 0.65 | 0.76 |
| 6 weeks | 25 | 25 | 0 | 0 | 3 | 2 | 8 | 10 | 14 | 13 | 0.21 | 0.4 |
| 9 weeks | 25 | 25 | 0 | 0 | 5 | 6 | 10 | 11 | 10 | 8 | 0.01 | 0.016 |
| 12 weeks | 25 | 25 | 0 | 0 | 10 | 6 | 10 | 13 | 5 | 6 | 0.0001 | 0.001 |
| Duration of treatment | Groups | Mean acne scar scores ± SD | P value |
|---|---|---|---|
| Baseline | Group A | 25.36 ± 6.57 | 0.82 |
| Group B | 24.92 ± 7.35 | ||
| 3 weeks | Group A | 24.88 ± 6.71 | 0.77 |
| Group B | 24.28 ± 8.16 | ||
| 6 weeks | Group A | 22.6 ± 6.33 | 0.83 |
| Group B | 23 ± 6.88 | ||
| 9 weeks | Group A | 20.4 ± 3.65 | 0.74 |
| Group B | 21.8 ± 6.95 | ||
| 12 weeks | Group A | 19.28 ± 4.77 | 0.69 |
| Group B | 19.92 ± 6.78 |
At the end of therapy, according to Goodman and Baron’s qualitative acne scar grading, in Group A, 5 out of 25 patients (20%) showed excellent response, that is, reduction in acne scars by two grades from baseline, 14 out of 25 patients (56%) showed good response, that is, reduction in acne scars by one grade from baseline and 6 out of 25 patients (24%) showed poor response, that is, no reduction in acne scar grade. Similarly, in Group B, at the end of therapy, 2 out of 25 patients (8%) showed excellent response, 13 out of 25 patients (52%) showed good response and 10 out of 25 patients (40%) showed poor response [Figure 1].
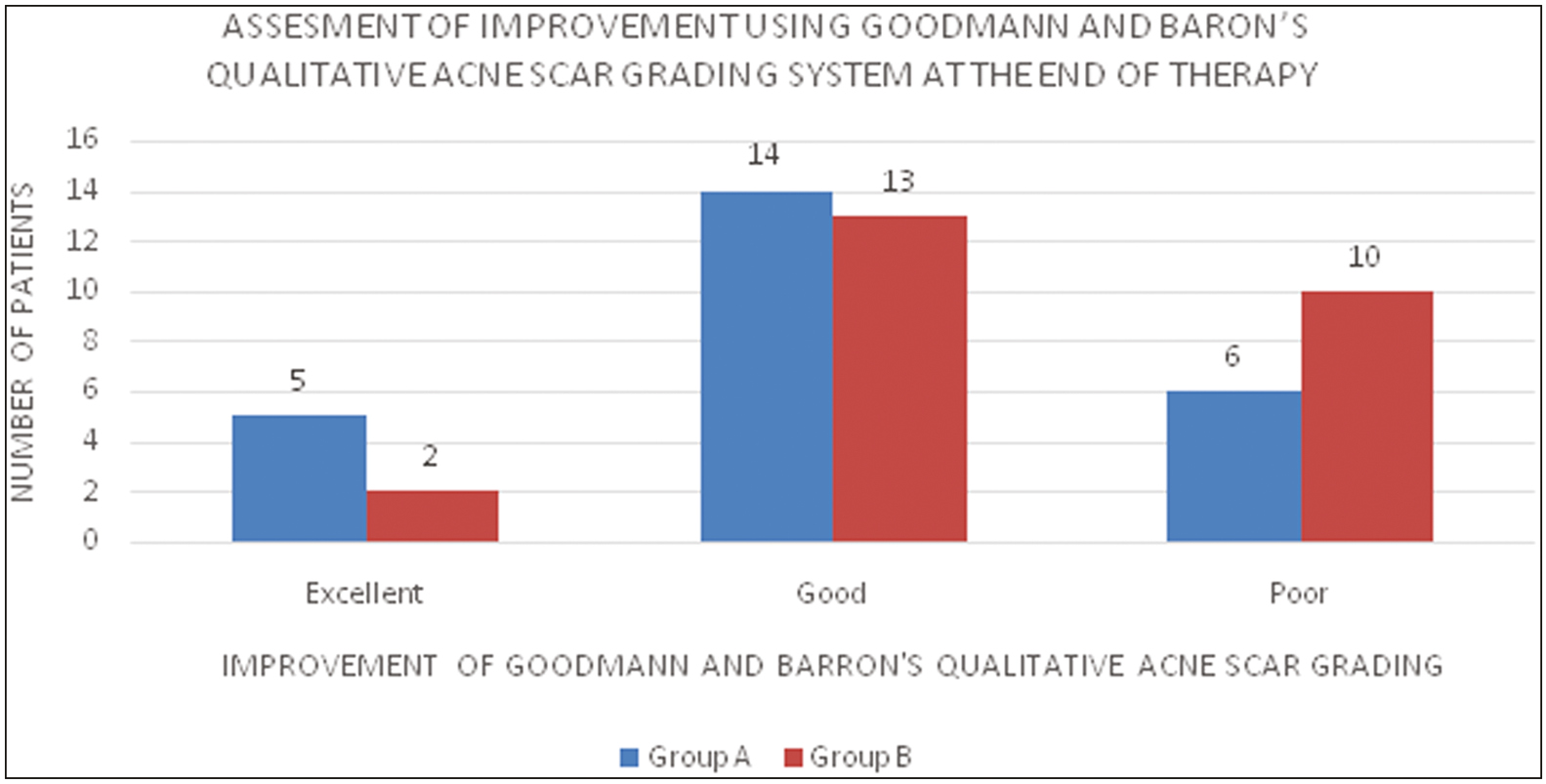
- Assessment of improvement using Goodman and Baron’s qualitative acne scar-grading system at the end of therapy
In Group A, baseline mean Goodman and Baron’s quantitative acne scar score was 25.36 ± 6.57, while in Group B, baseline mean Goodman and Baron’s quantitative acne score was 24.92 ± 7.35. At the end of therapy, that is, after 12 weeks of therapy, the mean percentage reduction in Goodman and Baron’s quantitative acne scar scores was 21.69% ± 16% in Group A and 20.97% ± 8.70% in Group B [Figure 2].
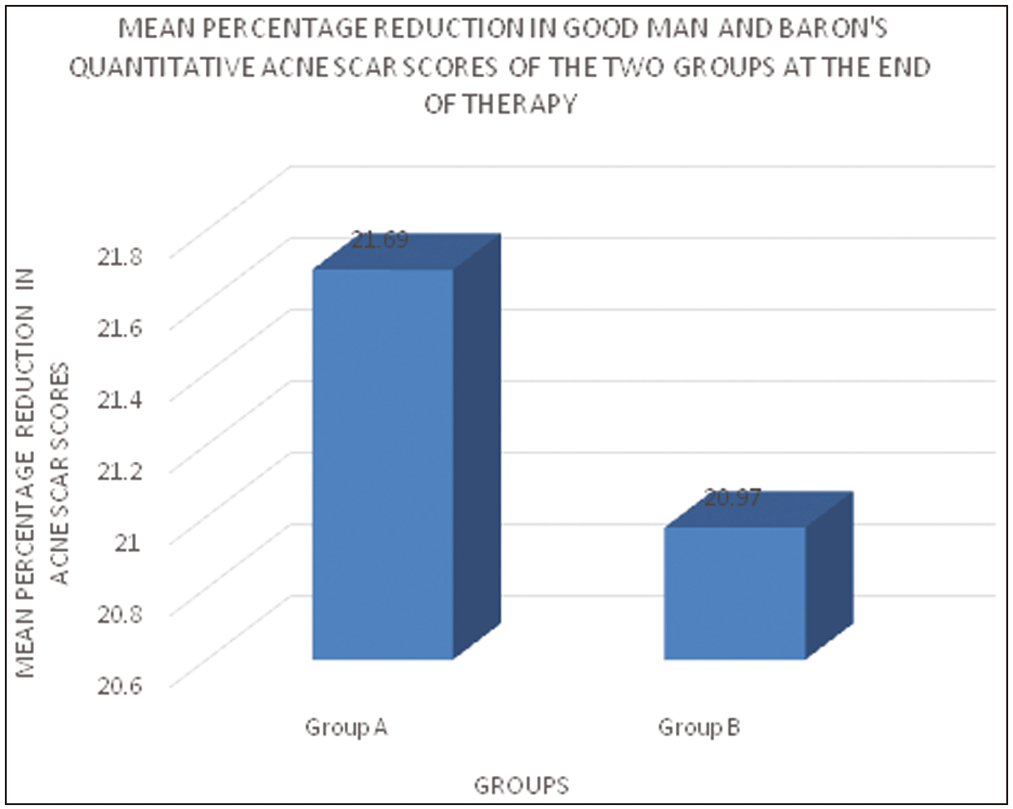
- Mean percentage reduction in Goodman and Baron’s quantitative acne scar scores of the two groups at the end of therapy
In regards of complications, both procedures were well tolerated. In Group A, 25 out of 25 patients (100%), while in Group B, 2 out of 25 patients (8%) developed erythema. In Group A, 15 out of 25 (60%) patients complained of mild burning sensation, while in Group B no one complained of burning sensation. In Group A, 3 out of 25 (12%) patients complained of itching, while in Group B, none of the patients complained of itching. In Group A, 2 out of 25 (8%) patients developed postinflammatory hyperpigmentation, while in Group B, 3 out of 25 (12%) developed postinflammatory hyperpigmentation.
DISCUSSION
In Group A, statistically significant improvement in Goodman and Barron’s qualitative acne scar grades was observed at the end of 9 weeks of therapy (P value: 0.016), which further became statistically highly significant at the end of 12 weeks (P value: 0.0001) [Figure 3]. Similarly, in Group B, statistically significant improvement in Goodman and Barron’s qualitative acne scar grades was seen at the end of 9 weeks of therapy (P value: 0.016), which further became statistically highly significant at the end of 12 weeks (P value: 0.001) [Figure 4].

- Photograph of a 23-year-old patient in Group A showing improvement after four sessions of Er:YAG laser

- Photograph of a 21-year-old patient in Group B showing improvement after four sessions of 20% TCA peel
It was observed that in Group A, significant reduction in mean Goodman and Baron’s quantitative acne scar scores was achieved earlier, that is, at 9 weeks of therapy as compared to Group B in which significant reduction in mean scores was observed after the completion of 12 weeks of therapy.
The difference in mean percentage reduction in Goodman and Baron’s quantitative acne scar scores between the two groups was statistically not significant (P value = 0.84) at the end of 12 weeks of therapy.
Nirmal et al.[9] conducted a study to assess the improvement of facial acne scars with Er:YAG 2940 nm fractional laser resurfacing and its adverse effects in 25 patients and reported at least fair improvement in 96% of cases. No serious adverse effects were noted during the study. In our study, we observed significant improvement in Goodman and Baron’s qualitative acne scar grades at the end of 12 weeks (P: 0.0001).
Shakir et al.[10] conducted a study to evaluate the safety and effectiveness of fractionated Er:YAG laser in treating 40 cases of moderate-to-severe atrophic acne scars. Fractional Er:YAG laser 2940 nm wavelength was delivered to the whole face with a single pass treatment and two passes were given to acne scar area. Ten patients (25%) reported excellent improvement, 21 patients (50%) significant improvement, 6 patients (15%) moderate improvement, and 4 patients (10%) mild improvement in the appearance of the acne scars. In our study, we used fractional Er:YAG laser in post-acne scars with maximum three passes and four sessions. Five out of 25 (20%) cases showed excellent response, 14 out of 25 (56%) cases showed good response, and 6 out of 25 (24%) cases showed poor response. The mean reduction in quantitative acne scar in Er:YAG laser was 21.69 ± 16. Thus, our study showed statistically significant improvement in acne scars after fractional Er:YAG laser (P < 0.05).
Al-Hamamy et al.[11] evaluated the effectiveness of 25% TCA combined with dermasanding. They reported a satisfactory improvement in acne scars with no significant complications except erythema and postinflammatory hyperpigmentation, which disappeared after 3 months in affected patients. In our study, we evaluated the effectiveness of 20% TCA as a chemical peel in post-acne atrophic scars. We also observed that a statistically significant improvement in Goodman and Baron’s qualitative acne scar grades at the end of the treatment (P = 0.001). The mean percentage reduction in quantitative acne scar in 20% TCA was 20.97 ± 8.70. Erythema in 8% cases and hyperpigmentation in 12% cases were observed as minor adverse effects.
Puri et al.[12] researched 25 patients who were divided into 2 groups. The first group had Jessner’s peeling with 20% TCA, while the latter had only 20% TCA. In the group treated with 20% TCA alone, mild improvement was seen in 32% of the patients, moderate improvement was observed in 40% of the patients, and marked improvement was observed in 25% of the patients. The results in both groups were similar. Thus, Puri et al.[12] demonstrated that 20% TCA peel is a superficial peel for facial skin improvement. In our study, 2 out of 25 (8%) cases showed excellent response, 13 out of 25 (52%) cases showed good response, and 10 out of 25 (40%) cases showed poor response in post-acne atrophic scars following 20% TCA chemical peel.
Although there is vast literature comparing multiple modalities in the treatment of acne scars, Er:YAG laser and TCA peeling are the two modalities which have been rarely compared yet. Till date, there is only one study available comparing the efficacy of these two modalities to the best of our knowledge. Sahel et al.[13] conducted a study to compare the clinical response to long-pulsed Er:YAG laser 2940 nm versus TCA 35% peeling in the treatment of different types of atrophic acne scars and reported that the overall improvement was equal in both groups (60%). However, the degree of improvement was better with Er:YAG laser than with TCA peeling. Thus, Sahel et al.[13] reported that both Er:YAG laser and TCA 35% were relatively safe and effective modality in the treatment of distensible ice pick, rolling, and shallow boxcar atrophic acne scars. However, one of the major limitations of this study was that they did not use a standard qualitative or quantitative acne scar-grading system for assessment of response. In contrast to Sahel et al.,[13] our study compared the efficacy of both the modalities based on the standard Goodman and Baron’s qualitative and quantitative acne scars scores, thus, making it more accountable. In our study, both groups showed significant improvement in acne scar scores.
CONCLUSION
We concluded that fractional Er:YAG laser resurfacing and 20% TCA peel application in the treatment of atrophic acne scar are equally efficacious. Both procedures are safe and well tolerated by the patients. We advocate the usage of both these modalities as first-line therapies for acne scar management. Twenty percent TCA peel can be used as a cheaper alternative of Er:YAG laser for acne scar.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Acne scarring-pathogenesis, evaluation, and treatment options. J Clin Aesthet Dermatol. 2017;10:12-23.
- [Google Scholar]
- A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19:303-8.
- [Google Scholar]
- Acne scarring: A classification system and review of treatment options. J Am Acad Dermatol. 2001;45:109-17.
- [Google Scholar]
- Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: A population based study. J Invest Dermatol. 2011;131:363-70.
- [Google Scholar]
- Advancing the care of post-acne scarring: Expert insights into new treatment options. J Drugs Dermatol. 2016;15:518-25.
- [Google Scholar]
- Postacne scarring: A qualitative global scarring grading system. Dermatol Surg. 2006;32:1458-66.
- [Google Scholar]
- Postacne scarring: A quantitative global scarring grading system. J Cosmet Dermatol. 2006;5:48-52.
- [Google Scholar]
- Laser erbium-YAG resurfacing. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2022.
- [Google Scholar]
- Efficacy and safety of erbium-doped yttrium aluminium garnet fractional resurfacing laser for treatment of facial acne scars. Indian J Dermatol Venereol Leprol. 2013;79:193-8.
- [Google Scholar]
- Treatment of acne scars using fractional erbium:YAG laser. Am J Dermatol Venereol. 2014;3:43-9.
- [Google Scholar]
- Evaluation of treatment of acne scars with 25% trichloroacetic acid chemical peel followed by manual dermasanding. J Cosmet Dermatol. 2021;20:1750-5.
- [Google Scholar]
- Efficacy of modified Jessner’s peel and 20% TCA versus 20% TCA peel alone for the treatment of acne scars. J Cutan Aesthet Surg. 2015;8:42-5.
- [Google Scholar]
- Erbium:YAG laser resurfacing versus trichloroacetic acid 35% peeling in the treatment of atrophic facial acne scars. J Pan-Arab League Dermatol. 2008;19:19.
- [Google Scholar]






