Translate this page into:
Full Thickness Macular Hole in Aesthetician Occurring Due to Accidental Self-exposure to Cosmetic Laser Machine Trying to Take Special Precautions Against COVID-19
Address for correspondence: Dr. Alay S. Banker, Banker’s Retina Clinic and Laser Centre, 5 Subhash Society, Ahmedabad 380009, Gujarat, India. E-mail: alay.banker@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
A 25-year-old aesthetician was operating Q-switch pulse (SPECTRA) cosmetic laser machine of 1,064 nm wavelength, for the purpose of skin bleaching. The probe suddenly slipped over the plastic sheet that had been placed to avoid COVID-19 exposure after which she complained of sudden loss of vision. She was diagnosed as having vitreous hemorrhage in her right eye and was treated conservatively for one month. She then complained of central scotoma and was diagnosed to have developed a full-thickness macular hole, for which she was advised vitrectomy surgery. The purpose of this case report is to emphasize the importance of taking precautions during the COVID-19 era and while doing that making sure how to handle the machines so as not to inflict any accidental injury to the operating physician. Macular Holes following skin bleaching with Nd:YAG laser occurring in operating aesthetician is rare as compared to that occurring in the patients.
Keywords
COVID-19
macular hole
Q-switch pulse cosmetic laser
skin bleaching
INTRODUCTION
The trend of using lasers for the purpose of beautification is seeing an immense rise in the recent years. Use of lasers over the face also proposes a threat to the nearby structures and organs on the face, especially if not used with proper precaution. The laser used commonly for facial procedure is the Q-switch Nd:YAG laser. Previous cases of accidental Nd: YAG laser injuries include several common features such as retinal and vitreous hemorrhage, occurring mainly in the patient’s eyes and not to the operating aesthetician. It is particularly harmful as it is designed to emit short pulses of high energy in durations of few to tens of nanoseconds and can deliver an invisible dose of energy very rapidly to the retina.[12] Use of high fluence and long wavelength lasers increases the risk of ocular injury due to deeper penetration of the organ by radiation. We report a rare case of full thickness macular hole occurring due to accidental self-exposure to cosmetic laser machine in the operating aesthetician while trying to take special precautions against COVID-19.
CASE REPORT
A 25-year-old aesthetician developed sudden blurring of vision and floaters in her right eye after an accidental laser injury. She was operating a SPECTRA (Q - switch) Nd:Yag cosmetic laser machine of 1,064-nm wavelength, having fluence:1.2J/cm2, spot size:8 for bleaching of skin. She was not wearing any protection for the eyes, but considering the current COVID scenario, she had kept a particular “plastic sheet” on the skin of the patient for the sake of aseptic precautions and also had worn a face shield. During adjusting the laser, the probe slipped over the plastic sheet and she heard a “pop” sound, felt a flash in her right eye followed by floaters and severe dimness of vision. She was diagnosed elsewhere as having vitreous hemorrhage and was treated conservatively with oral steroids. Three weeks later, she presented to us with complains of central scotoma in her right eye. Her best corrected visual acuity in right was counting fingers at 3 meters and left eye was 20/20. On examination her anterior segment was within normal limits in both eyes. Posterior Segment examination revealed full thickness macular hole (FTMH) and resolving vitreous hemorrhage in right eye [Figure 1]. Left eye fundus showed few retinal pigment epithelial changes in macula. Imaging including spectral domain optical coherence tomography (SD-OCT) identified an 800 mm FTMH with IS-OS junction disruption with cystic spaces at the edges of the hole in right eye [Figure 2]. The patient was advised vitrectomy surgery for the repair of her macular hole in her right eye.
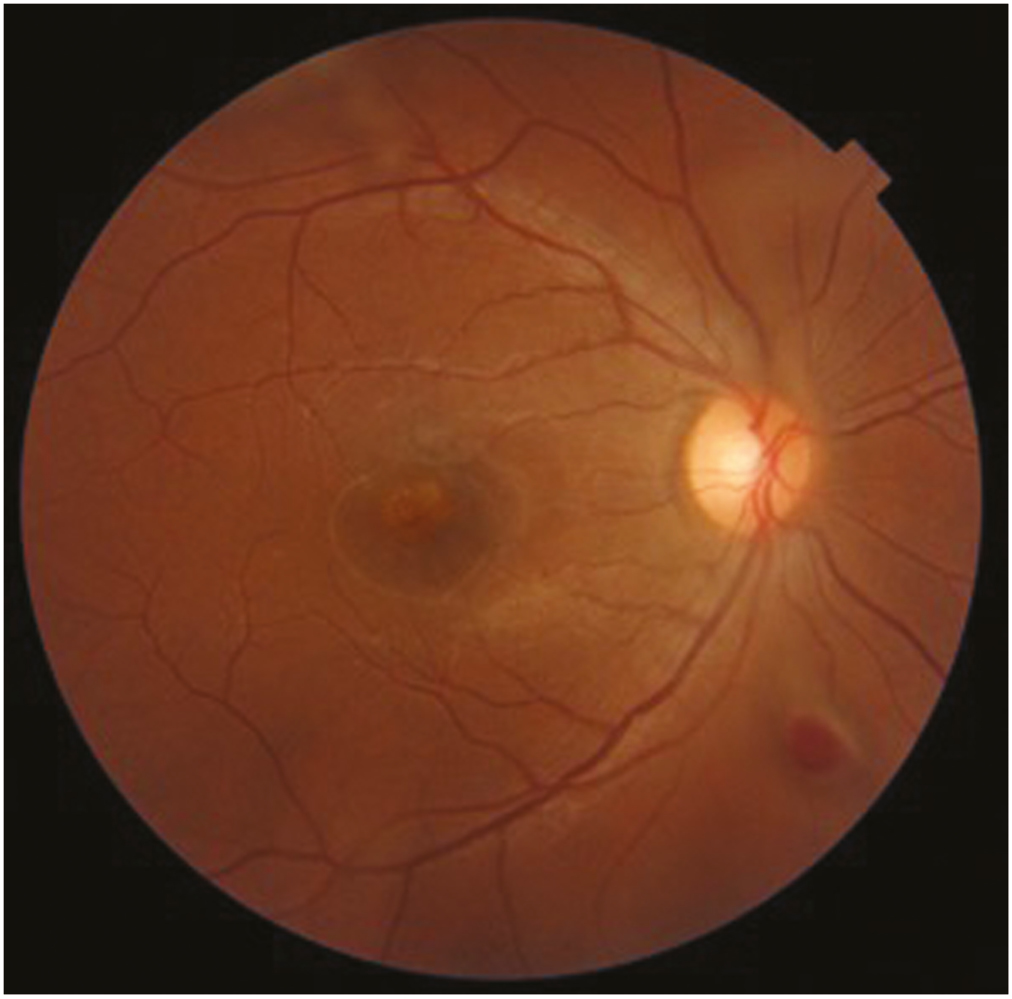
- Fundus photo of the right eye reveals full thickness macular hole and resolving vitreous hemorrhage
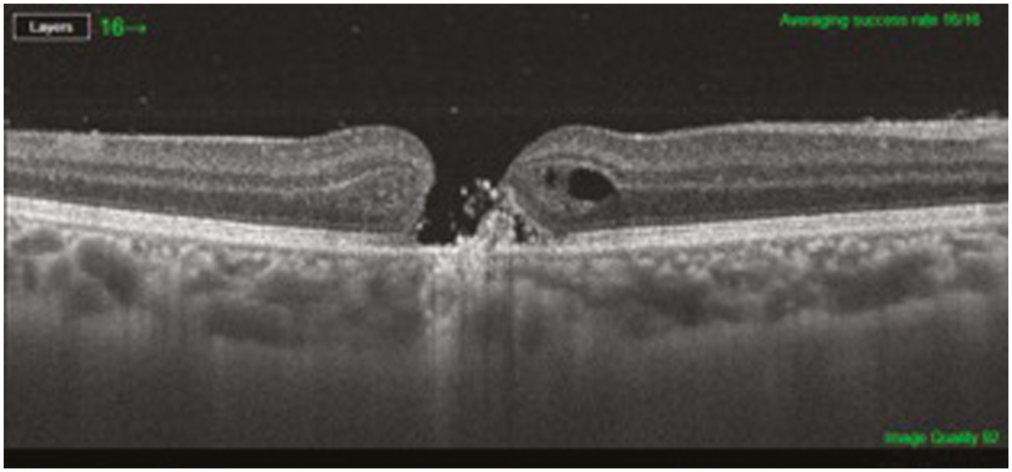
- Spectral domain optical coherence tomography (SD-OCT) shows a full thickness macular hole with IS-OS junction disruption and hyperreflective mass in base with cystic spaces at the edges of the hole in right eye
DISCUSSION
Lasers are effective modalities for facial cosmetic treatments, but can cause injury to the eye when used periorbitally or on the eyelids.[12] Several safety measures can prevent laser ocular injury. First, the treating physician must be properly trained to operate the laser, and should have basic knowledge in laser physics and safety. Second, lesions around the eye or on the eyelids should not be treated without metal ocular shields or wavelength-specific glasses, including eye protection for operating personnel. Care must be taken to ensure eye protection is not removed or moved, especially during long procedures. Third, frequent and sufficient cooling of the treated areas must be ensured to prevent thermal injury and overheating of the metal corneal shields. Despite these precautions, laser ocular injury might still occur, though rarely.[1-8] However, in most cases the injuries occur to the patients and not to the operating aesthetician. Our case is unique in the sense that the injury occurred to the operating aesthetician herself and that too due to inadvertent slipping of the probe over the plastic sheet while trying to take special precautions in the setting of COVID-19 pandemic. It is ofcourse to be noted that she was not wearing any protective eye glasses inside the face shield for COVID-19 protection. Lasers in the visible to near-infrared spectrum (400 nm–1400 nm) are hazardous to the retina and as most lasers used in dermatology fall within this spectrum, caution should be undertaken when operating cosmetic lasers. This highlights the critical need for aestheticians to use eye protection for themselves and also provide proper eye protection to patients by using wavelength-specific goggles or spectacles during the entire procedure.
One of the mechanisms by which lasers work, for skin bleaching treatment is that of selective photothermolysis. Selective photothermolysis allows clinicians and trained aestheticians to treat pigmented and vascular lesions, perform facial resurfacing, and remove hair in select areas. Clinically, the 1064 nm Nd:YAG laser, which is implicated in the majority of laser-induced ocular injuries, is capable of causing retinal hemorrhage, vitreous hemorrhage, scarring, preretinal membrane formation, and retinopathy when the radiation is absorbed by the melanin-rich retinal pigment epithelium. Initially, the Nd:YAG energy is absorbed by melanin located in the retinal pigment epithelium (RPE) and creates tissue ionization, plasma formation, and an acoustic shock wave that spread centrifugally leading to mechanical disruption of the surrounding retina, RPE, and choroid.[12,4] Over time, the initial injury causes a release of inflammatory mediators from the directly damaged cells that lead to collateral damage to neighboring cells. Late complications include chorioretinal scarring and neovascularization, macular cyst, macular pucker, and FTMH.[1-8] Some FTMHs may close spontaneously, but most cases require surgical repair.[3-12]
In laser-induced cases, the posterior hyaloid is still partially attached with a localized detachment over the FTMH, but tractional forces may develop due to disruption of retinal tissue and retinal fibroglial formation.[9] Spontaneous closure of laser-induced holes may relate to small initial hole size and the presence of hemorrhage that may act as tissue glue.[9] In this case, the FTMH formation may have been due to a combination of mechanical and thermal damage. Had the injury occurred in a controlled manner with this Q-switched Nd:YAG laser, the damage mechanism would have certainly been optical break down within the retinal tissue. However, the OCT image suggests a thermal component to the injury. The loss of tissue seen at the center of the macula suggests optical breakdown, while the white, hyperreflective mass at the base of the hole and the patient’s history suggest thermal damage. In our case, the treating aesthetician developed a full thickness macular hole following inadvertent exposure to the pulse of the laser. The COVID pandemic has necessitated medical fraternity to come out with unique solutions to safeguard themselves while treating patients. However, one should also keep in mind the possibilities of accidents occurring due to that like what happened in our case to the operating aesthetician.
Financial support and sponsorship
No financial associations or grants to declare .
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Ocular injury in cosmetic laser treatments of the face. J Clin Aesthet Dermatol. 2018;11:15-8.
- [Google Scholar]
- Laser-induced macular holes demonstrate impaired choroidal perfusion. Retina. 2004;24:92-7.
- [Google Scholar]
- Accidental nd:YAG laser-induced macular hole in a pediatric patient. Ophthalmic Surg Lasers Imaging Retina. 2013;44 Online:e7-10.
- [Google Scholar]
- A case of accidental ocular injury from cosmetic laser burn. Retin Cases Brief Rep. 2016;10:115-20.
- [Google Scholar]
- A case of accidental macular injury by nd: YAG laser and subsequent 6 year follow-up. Korean J Ophthalmol. 2009;23:207-9.
- [Google Scholar]
- Vitrectomy and autologous thrombocyte adhesion of an accidental macular hole caused by nd:YAG laser. Br J Ophthalmol. 1997;81:803-4.
- [Google Scholar]
- Vitrectomy with indocyanine green-guided inner limiting membrane peeling for a Q-switched nd:YAG laser-induced macular hole. Retina. 2003;23:714-6.
- [Google Scholar]
- Vitrectomy and microperimetry of an accidental macular hole caused by nd:Yag laser. Case Rep Ophthalmol. 2010;1:80-4.
- [Google Scholar]
- Vitrectomy for macular hole following nd:YAG laser injury. Taiwan J Ophthalmol. 2016;6:195-8.
- [Google Scholar]






