Translate this page into:
Giant trichilemmal cyst of scrotum
*Corresponding author: Anirudha D. Gulanikar, Department of Dermatology, MGM Medical College and Hospital, N-6 Cidco, Aurangabad, Maharashtra, India. agulanikar@hotmail.com
-
Accepted: ,
How to cite this article: Gulanikar AD, Kulkarni OS, Kulkarni J, Reddy N. Giant trichilemmal cyst of scrotum. J Cutan Aesthet Surg. 2024;17:249-51. doi: 10.4103/JCAS.JCAS_43_21
Abstract
A 45-year-old man with an asymptomatic lesion on the scrotum since 25 years presented to the skin out patient department (OPD). There were multiple skin-colored to hyperpigmented nodules with areas of calcification on the scrotum. The mass measured 20 cm × 10 cm × 8 cm as a whole. Steatocystoma was clinically diagnosed and excision of the lesion was performed by a plastic surgeon. The mass was removed en masse and the removed specimen was measured to be 20 cm × 10 cm × 5 cm. On histopathological examination, the cysts showed epithelium resembling that of outer hair root sheath. Contents of the cysts were homogenous unlamellated keratin with focal calcification.
Keywords
Adnexal tumor
Giant trichilemmal cyst
Pilar cyst
Steatocystoma multiplex
Trichilemmal cyst
CASE REPORT
A 45-year-old man came to skin out patient department (OPD) complaining of progressive increase in scrotum size since the past 25 years. The mass was asymptomatic except for occasional exudation of whitish chalky material from the surface of the mass. It was not associated with pain or tenderness.
On examination, there were multiple skin colored to hyperpigmented nodules with areas of calcification, the smallest nodule measuring 2 cm × 2 cm × 1 cm and the largest measuring 5 cm × 4 cm × 2 cm present on the scrotum. The whole mass was measured to be 20 cm × 10 cm × 8 cm en masse [Figure 1].

- Preoperative clinical picture of scrotal cysts as seen from the front.
Differential diagnosis of idiopathic scrotal calcinosis, steatocystoma multiplex, and pilar cyst were placed. High-frequency ultrasound of mass revealed irregular thick-walled hyperechoic calcific areas with poor acoustic penetration. Underlying tissue was normal in architecture and vascularity as found on the Doppler scan.
The patient was investigated and excision of the mass was planned in coordination with the plastic surgery department. The following three surgical approaches were considered: (1) excision en masse without grafting, (2) excision en masse with skin grafting, and (3) excision in two or three stages. Considering that the skin of the scrotum is loose, there was no need for a graft; thus, excision en masse without grafting was planned.
The mass was completely removed after dissection from normal tissue. The resultant specimen was measured to be 20 cm × 10 cm × 5 cm.
Histopathology showed cysts lined by epithelium that resemble the outer root sheath at the level of the isthmus as it keratinized without the formation of the granular layer. Cyst contained homogenous unlamellated keratin with foci of calcification [Figure 2].
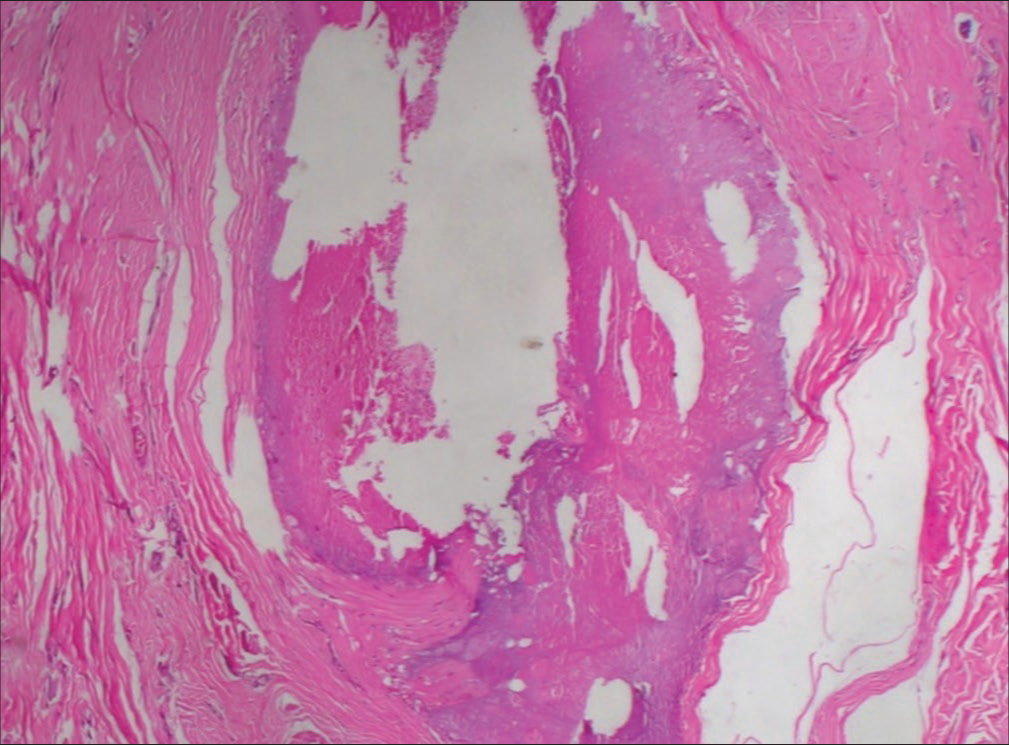
- Histopathological picture showing cross-section of a cystic cavity lined by keratinized epithelium without granular layer.
Thus, the final diagnosis of the trichilemmal cyst was made.
DISCUSSION
Trichilemmal cyst is a benign adnexal tumor usually occurring on hair-bearing such as scalp, neck, trunk, and groins.1 These arise from outer root sheath or trichilemma.
The lesion presents as a solitary, skin-colored papule or nodule, with a smooth, sometimes telangiectatic surface.2
These occur sporadically or are inherited in an autosomal dominant fashion. Those with a family history show multiple cysts and early onset.3 Although our patient had multiple lesions, he had no family history.
Trichilemmal cysts can gradually increase in size and number, which is said to be the result of the budding of daughter cysts from the parent lesion.4
As these are derived from outer root sheath, they are common areas with a high concentration of hair such as the scalp (90%). Multiple lesions (70%) are more common than solitary lesions (30%).1 These are benign, usually asymptomatic, and progress very very slow.3 In our patient, these were asymptomatic, multiple, and showed very slow progression over the course of 25 years.
Long-standing cysts can become infected and tender, so a course of a systemic antibiotic is appropriate before definitive management by surgical excision.5
The usually slowly progressive cysts have a variant that progresses rapidly called proliferating trichilemmal cysts. These are managed by surgical excision.6
The histological hallmark of trichilemmal cyst is the presence of trichilemmal keratinization, that is, an abrupt transition from a nucleated epithelial cell to an anucleate keratinized cells without the formation of a granular layer.7
The commonly accepted treatment for trichilemmal cysts is local excision with or without skin grafting.8
CONClUSION
Long standing tumors in scrotum may become extensive is size. Careful examination and relevant investigation should be performed to rule out malignant changes before surgical excision. In our case although huge mass there it was without damaging underlying structures and histopathologically evaluated to rule out secondary malignant changes.
Authors’ Contributions
All the authors contributed to the research study. Anirudha D. Gulanikar: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Omkar S. Kulkarni: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Jiten Kulkarni: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Nikhil Reddy: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
References
- Giant trichilemmal cyst at the neck region. J Craniofac Surg. 2009;20:961-2.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous Adnexal Tumors (1st ed). Philadelphia, PA: Wolters Kluwer; 2015. p. :313-6.
- [Google Scholar]
- Hereditary trichilemmal cysts: A proposal for the assessment of diagnostic clinical criteria. Clin Genet. 2013;84:65-9.
- [CrossRef] [PubMed] [Google Scholar]
- The natural history of trichilemmal cysts. Br J Dermatol. 1976;94:379-90.
- [CrossRef] [PubMed] [Google Scholar]
- An inflamed trichilemmal (pilar) cyst: Not so simple? N Am J Med Sci. 2011;3:431-4.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferating trichilemmal tumor: Case report. An Bras Dermatol. 2011;86:S190-2.
- [CrossRef] [PubMed] [Google Scholar]
- "Sebaceous cysts" are trichilemmal cysts. Arch Dermatol. 1969;99:544-55.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferating pilar tumors: A clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol. 2004;122:566-74.
- [CrossRef] [PubMed] [Google Scholar]






