Translate this page into:
Idiopathic Guttate Hypomelanosis Treated with 308-nm Excimer Light and Topical Bimatoprost
Address for correspondence: Dr. Firas Constantin Kreeshan, Everything Skin Clinic, Suite B, Haw Bank House, Cheadle SK8 1AL, UK. E-mail: fkreeshan@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Idiopathic guttate hypomelanosis (IGH) is an acquired pigmentary disorder that is characterized by the presence of multiple hypopigmented macules on the shins and forearms. Albeit asymptomatic, it can cause considerable cosmetic anxiety. The pathogenesis is not fully understood and to date, there have been no successful treatments. We report a case of a 48-year-old female who presented with an 8-year history of multiple hypopigmented macules on both legs, typical of IGH. She previously failed to respond to topical pimecrolimus. She received targeted phototherapy with an excimer lamp (308 nm, 250–480 mJ), and a small patch was treated once daily with topical bimatoprost, in addition to the excimer lamp. After five sessions, better improvement was noted on the combination treatment patch; she received combination treatments for further six sessions. Good repigmentation has been achieved on the smaller macules. The larger depigmented macules continue to improve with further treatments. A combination of excimer light with topical bimatoprost appears to be a promising potential treatment option for IGH, a condition where management options are otherwise limited.
Keywords
Bimatoprost
excimer light
idiopathic guttate hypomelanosis
INTRODUCTION
IGH is a benign acquired pigmentary disorder that is characterized by the presence of multiple oval hypopigmented macules on the arms and shins. The exact pathogenesis is unclear; however, chronic sun exposure has been implicated.[1] Although asymptomatic, it can cause considerable cosmetic anxiety, especially in patients with darker skin. There are no universally effective treatments.
CASE REPORT
A 48-year-old female presented with an 8-year history of multiple depigmented macules on her legs, and this was diagnosed as IGH. She had Fitzpatrick skin phototype 4 and a positive family history of IGH. Previous treatment with topical pimecrolimus was ineffective. She received targeted phototherapy with an excimer lamp (308 nm, 250–480 mJ) and in addition, a small patch was treated with once-daily topical bimatoprost (Lumigan 0.1 mg/mL). After five sessions, better improvement was noted on the combination treatment patch; she received combination treatments for further six sessions. Good repigmentation was achieved on small macules, and larger macules continued to improve [Figures 1 and 2].
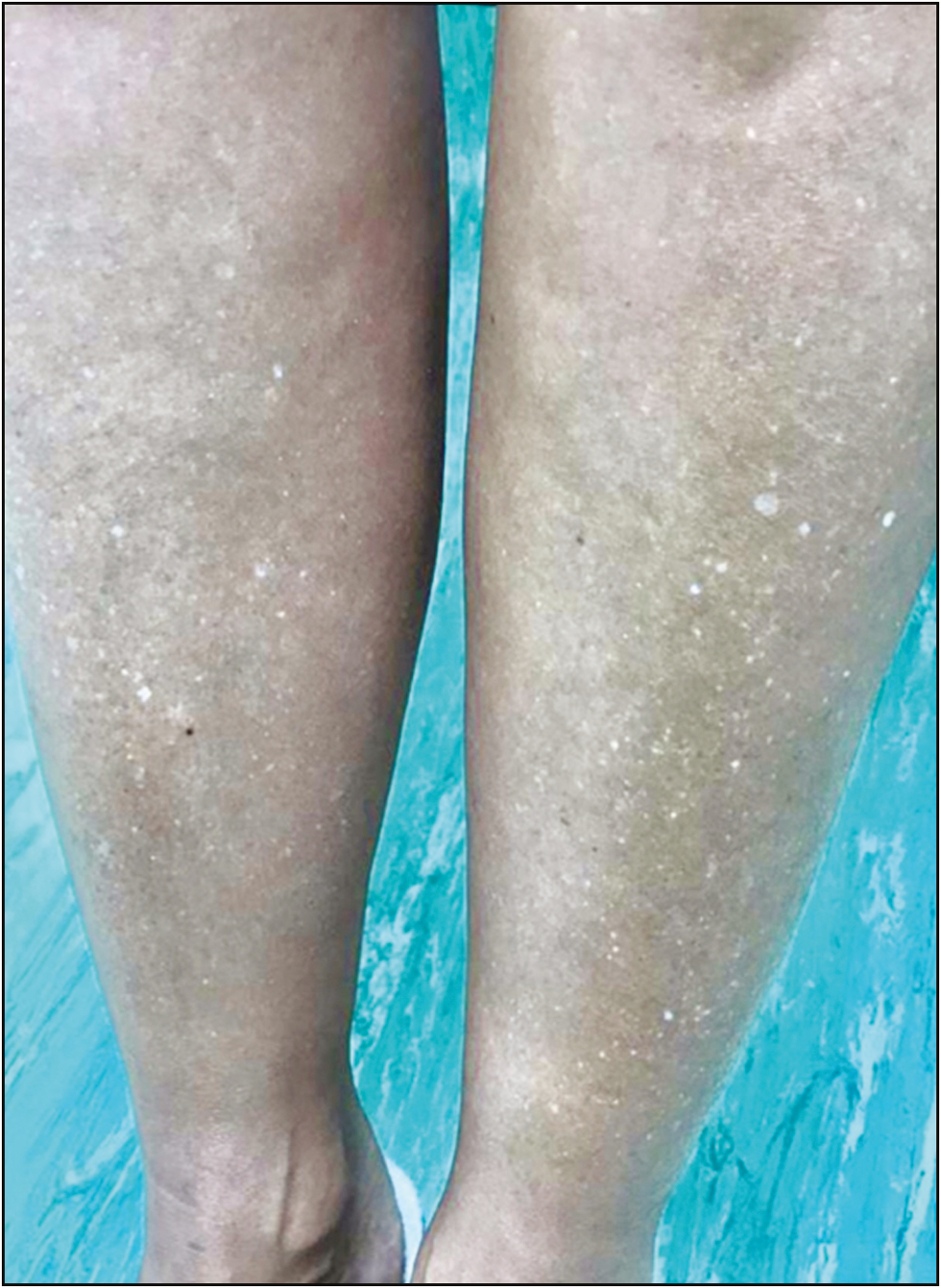
- Before treatment

- After treatment
DISCUSSION
IGH is usually diagnosed based on history and clinical picture, and it should be differentiated from other hypo/ depigmentary disorders such as vitiligo, pityriasis versicolor, progressive macular hypomelanosis, lichen sclerosis et atrophicus, guttate morphea, and postinflammatory hypopigmentation. Histologically, IGH typically shows hyperkeratosis with an atrophic epidermis, and flattened rete ridges. There is decreased melanin content and a reduced number of melanocytes.[2] Electron microscopy studies by Kakepis et al.[3] demonstrated normal density and structure of melanocytes but an abnormal and reduced uptake of melanocytes by the keratinocytes, suggesting a possible dysfunction disorder of the keratinocytes.
As no standard treatment is available for IGH, different medical and surgical modalities such as topical retinoids, topical calcineurin inhibitors, phenol peels, cryotherapy, superficial dermabrasion, skin grafting, and ablative and nonablative lasers have been trialed with variable success rates.
Excimer laser or light has been used for the treatment of vitiligo for many years. It stimulates repigmentation through its immunosuppression and immunomodulation effect. It is hypothesized that it stimulates melanocytes to produce melanin through keratinocyte release of enolin-1.[4] In a pilot study of six patients, Gordon et al. showed that the excimer laser was an effective treatment option for IGH. At the end of their 12-week study, significant repigmentation was achieved in most of the treated lesions.[5]
Bimatoprost is a prostamide F2a analogue used in the treatment of glaucoma. Increased eyelid pigmentation and hypertrichosis are its notable side effects. Bimatoprost is being increasingly used in a number of dermatological conditions such as vitiligo and alopecia areata. A histopathological study by Kapur et al. showed that bimatoprost-induced hyperpigmentation is caused by increased melanogenesis.[6]
We presented a case of IGH successfully treated with a combination of excimer light and topical bimatoprost. We conclude that this combination approach is a promising potential treatment option for IGH, a condition where management options are otherwise limited.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form/ forms, the patient(s) has/ have given his/ her/ their consent for his/ her/ their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Clinical features of idiopathic guttate hypomelanosis in 646 subjects and association with other aspects of photoaging. Int J Dermatol. 2011;50:798-805.
- [Google Scholar]
- Comprehensive understanding of idiopathic guttate hypomelanosis: Clinical and histopathological correlation. Int J Dermatol. 2010;49:162-6.
- [Google Scholar]
- Idiopathic guttate hypomelanosis: An electron microscopy study. J Eur Acad Dermatol Venereol. 2015;29:1435-8.
- [Google Scholar]
- Melanocyte destruction and repopulation in vitiligo. Pigment Cell Res. 1994;7:193-203.
- [Google Scholar]
- Excimer light treatment for idiopathic guttate hypomelanosis: A pilot study. Dermatol Surg. 2017;43:553-7.
- [Google Scholar]
- Bimatoprost -unduced periocular skin hyperpigmentation: Histopathological study. Arch Opthalmol. 2005;123:1541-6.
- [Google Scholar]






