Translate this page into:
Intra-individual Right-Left Comparative Study of Combined Therapy of Intramatricial Triamcinolone and Platelet-Rich Plasma vs. Intramatricial Triamcinolone Only in Lichen Planus-Associated Nail Dystrophy
Address for correspondence: Dr. Fozia Rehman, Department of Dermatology, Venereology, and Leprosy, Government Medical College Srinagar, Karan Nagar, Jammu and Kashmir 190010, India. E-mail: drfoziarehman16@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
While intramatricial triamcinolone is the most commonly used treatment option for onychodystrophy due to lichen planus, the role of platelet-rich plasma (PRP) in the treatment of onychodystrophy is not established. So we combined the two treatment modalities to assess the synergistic action on nail dystrophy.
Aims and Objectives:
The aim of this article is to compare the effect of combination of intramatricial triamcinolone and PRP vs. intramatricial triamcinolone alone in the treatment of onychodystrophy.
Materials and Methods:
This study was done in 26 and 25 pairs of symmetrical dystrophic nails in hands and feet, respectively. The patients received intramatricial injection of triamcinolone and PRP on one side of finger and toe nails and triamcinolone on the contralateral side.
Results:
Statistically significant improvements in grades of dystrophy according to the Nail Dystrophy Grading System (NDGS) in the finger and toe nails treated with combined therapy were obtained (P < 0.001 and = 0.002, respectively). According to the physician global assessment, response to combination therapy was statistically significant between the two comparison groups of finger and toe nails (P = 0.001 and = 0.004, respectively). Similarly, according to the patient satisfaction score, statistically significant difference was found between the comparison groups of combination therapy and single therapy (P < 0.001).
Conclusion:
Addition of PRP significantly improved the nail quality. Intramatricial PRP is a safe and effective therapeutic modality in refractory nail dystrophies.
Keywords
Intramatricial injection
onychodystrophy
platelet-rich plasma
triamcinolone
INTRODUCTION
Onychodystrophy can be seen in various dermatological disorders like psoriasis, lichen planus, alopecia areata, connective tissue diseases, onychomycosis, and various ectodermal syndromes and can be idiopathic in nature.[12] Lichen planus is one of chronic inflammatory dermatological disorders in which nail and mucosal involvement can sometimes be seen without cutaneous lesions. The severity of onychodystrophy varies from disease to disease, within patients of same disorder, and also between nails of hands and feet and also from one nail to other depending on the proportion of germinative nail matrix involvement. Different types of nail findings seen in lichen planus include nail plate thinning, longitudinal ridging and striations, fissuring, distal splitting, subungal hyperkeratosis, onycholysis, trachonychia, and pterygium unguis with or without nail discoloration. Finger nails are more commonly affected than toe nails.[345]
Onychodystrophy, though painless but being visible disorder, has got a significant negative impact on self-esteem of a person irrespective of their gender and forces the patient to consult a dermatologist for treatment. However, at the same time, it is difficult to dealt with due to complex and unique anatomy of nail unit. Proximal nail fold which is formed by double layer of skin and nail plate protects the nail matrix and nail bed, respectively, but at the same time prevents the effective topical drug delivery.[6] Systemic drug administration for long duration with associated risks and adverse effects also does not form rationale for treatment of onychodystrophies in case of single or few nail involvements. Various methods have been used to enhance drug delivery within nail unit but intralesional therapy, a form of “targeted therapy,” is most commonly used by practitioners which help in administration of a drug at a site where it is most required.[7] The germinative portion of nail, i.e. the nail matrix and the little extent of nail bed, needs to be targeted in various inflammatory nail dystrophies. Most common drugs administered intramatricially for various nail dystrophies include steroids, methotrexate, and cyclosporin; however, intramatricial triamcinolone is most commonly used in the concentration of 2.5–10 mg/mL at intervals of 4–6 weeks.[8910] There are reports of use of platelet-rich plasma (PRF) for refractory nail dystrophies with good results.[11] So we conducted this study to see whether or not combined therapy of intramatricial PRP and triamcinolone is more effective than intramatricial triamcinolone therapy alone in treating refractory nail dystrophy.
MATERIALS AND METHODS
This study was conducted after approved by the Institutional Ethical Committee and included 14 cases of onychodystrophy attending the Outpatient Department of Dermatology of Government Medical College Srinagar, Kashmir over a period of 10 months. All cases of onychodystrophy were subjected to detailed clinical history and cutaneous and mucosal examination. Informed consent was taken from all cases. The necessary laboratory investigations advised before proceeding with the interventional therapy included complete blood count including manual platelet count (CBC +MPC), fasting blood sugar levels, triple serology-HIV, HBSAG and ANTI HCV, KOH smear of nail scrapings. Inclusion criteria for the case to be included were: a person of age more than 14 years with dystrophy of symmetrical nails of either hand or feet or both and who has not taken any systemic or intralesional therapy in the past 6 months. Exclusion criteria were: age less than 14 years, nail scrapings positive for fungal elements on KOH smear, MPC less than 1.5 lakh, hypersensitivity to lignocaine, history of any oral or intralesional therapy in the past, diabetes mellitus, pregnancy, and those with unrealistic high expectations.
All the nails were photographed before starting therapy, at each session, and 4 weeks after the last session of intramatricial therapy.
Although Naildex is a valid and reliable measure of onychodystrophy severity in our study, the severity of nail dystrophy was quantitated with a self-designed objective Nail Dystrophy Grading System (NDGS), which is simple and feasible.[12] For this, the surface of the nail was divided into four quadrants (1, 2, 3, and 4) and each quadrant was graded as per the status of the respective nail quadrant from grades 1 to 5 as G1, G2, G3, and G4 [Table 1]. Thus, the total grade (NDGS-T: G1 + G2+ G3 + G4) varies from 4 (which denotes normal/almost normal appearing nail) to 20 (which denotes anonychia). Similarly, average grade (NDGS-T/4) varies from 1 to 5 [Figure 1].
| Nail Dystrophy Grading System | |
|---|---|
| Grade | Description |
| 1 | Normal appearing nail/almost normal nail/nail with insignificant pits, longitudinal or transverse striations or discoloration |
| 2 | Nail plate present with significant longitudinal or transverse striations/splits or discoloration |
| 3 | Nail plate present but totally dystrophic nail plate with discoloration |
| 4 | Small or thin nail speck present with significant scarring in respective quadrant |
| 5 | Anonychia/total scarring of nail quadrant |
![Self-designed objective NDGS, average grade of nail= [G1+ G2 +G3+G4]/4](/content/173/2021/14/3/img/JCAS-14-311-g001.png)
- Self-designed objective NDGS, average grade of nail= [G1+ G2 +G3+G4]/4
Patients received intramatricial injection of triamcinolone (5 mg/mL) and PRP (T + P) on one side of finger and toe nails and triamcinolone (T) on the contralateral side. Each side was given consistent treatment for the reason of feasibility and to avoid confusion. Right-sided nails received single modality of treatment and left side was given both intramatricial injection of triamcinolone and PRP.
Method of PRP preparation
After apheresis, PRP was prepared by a double-spin centrifugation technique using an automated centrifuge machine (REMI PRP centrifuge) and then transferred to 32G syringes for intramatricial administration.[1314]
Method of intramatricial injection
For anesthesia before injecting PRP or triamcinolone, topical lidocaine anesthetic cream under occlusion or digital nerve anesthesia and cooling with ice cubes was done for patients who could tolerate pain while giving injection. The 32G insulin syringe was used to administer injections. After cleaning the local area of injection, needle is entered at point of injection which is 2 mm below and 2 mm lateral to the junction of proximal and lateral nail folds. After insertion, needle is kept almost parallel to the skin surface and advanced till resistance is lost and advanced up to mid of proximal nail fold, and injection of 0.1–0.2 mL content is administered to raise the semilunar blanch. Needle is withdrawn and sustained pressure is given to ensure adequate hemostasis, thus preventing subungal hematoma.[6]
Number of intramatricial sessions
Since finger nails show faster growth when compared with toe nails, five monthly sessions of triamcinolone were given for both sides of finger nails at 0 visit, 4 weeks (wk), 8 wk, 12 wk, 16 wk and six monthly sessions were done for toe nails at 0 visit, 4 wk, 8 wk, 12 wk, 16 wk, and 20 wk. Intralesional PRP in nails of only one side of hand and/or feet was given after an interval of 2 weeks of every monthly triamcinolone injection. Accordingly, intramatricial PRP was given on one side of hand at 2 wk, 6 wk, 10 wk, 14 wk, and 18 wk and in toe nails at 2 wk, 6 wk, 10 wk, 14 wk, 18 wk, and 22 wk. The rationale behind the increased number of sessions for toe nails is the difference in rate of growth of nail plates between hand and feet.[15]
At each follow-up session, all nail units were subjected to clinical examination, photography, and dermoscopy for improvement and side effects. Final follow-up assessment was done for finger and toe nails at 1 month after the previous steroid session, i.e. at 20 and 24 wks, respectively, and was graded using the same NDGS as used before starting intralesional therapy.
At final follow-up session, physician’s perception of improvement was graded by Physician’s Global Assessment (PGA) scores (based on clinical assessment as well as on evaluation of photographic records). This was graded as good response (>50% improvement), moderate response (25–50% improvement) and poor response (<25% improvement). The satisfaction of response in both sides was also subjectively graded using Patient’s Satisfaction Score on a four-point scale from 1 to 4 as follows: 1—least satisfied, 2—slightly satisfied, 3—satisfied, and 4—very satisfied.
Statistical analysis
The data were analyzed using computer software Microsoft Excel and SPSS version 21.0 for Windows. Data are reported as mean ± standard deviation and proportions as deemed appropriate for quantitative and qualitative variables, respectively. The statistical difference in mean value between the two groups was tested using the Mann–Whitney Test. A P-value of <0.05 was considered as statistically significance. All P-values reported were two-tailed.
RESULTS
Our study included 14 patients (4 males and 10 females) and age of the patients varied from 14 to 55 years with mean age of 27.5 ± 11.59 years. The maximum number of patients (10) belonged to second and third decades. Duration of onychodystrophy varied from 4 to 18 months with a mean duration of 6.5 months. Upon cutaneous and mucosal examination, cutaneous lesions of lichen planus were seen in four patients, mucosal lesions in three patients, and both in two patients. However, there were five patients in whom no cutaneous or mucosal lesions were found but typical nail changes were present and clinically diagnosed as nail lichen planus. The number of nails affected per patient varied from single pair to all nails of both hands and feet; however, we included and analyzed only symmetrical 26 pairs of finger nails and 25 pairs of toe nails in our study.
In finger nails, according to our self-designed NDGS, mean initial average grade was 2.73 ± 0.92 in the combined therapy group (FN-T + P) and 2.72 ± 0.92 in the single therapy group (FN-T). In toe nails, the mean initial average grade was 3.75 ± 1.07 in the combined therapy group (TN-T + P) and 3.59 ± 1.08 in the single therapy group (TN-T). The statistical difference between the two groups was insignificant (P = 0.897 and P = 0.314, respectively), indicating the same grade of dystrophy between both the finger nail and toe nail treatment groups. Similarly, at the final follow-up visit, using the same self-designed NDGS, in finger nails, the mean final average grade was 1.54 ± 1.01 in the combined therapy group (FN-T + P) and 2.27 ± 1.03 in the single therapy group (FN-T). While in toe nail, the mean final average grade was 2.61 ± 1.77 in the combined therapy group (TN-T + P) and 3.03 ± 1.48 in the single therapy group (TN-T). The statistical difference between the two groups was significant (P < 0.001 and P = 0.002, respectively), indicating significant add-on effect of PRP in response to treatment [Figures 2A–C and 3A–C].

- A. Picture showing bilateral nail dystrophy before treatment. B. Clearly evident improvement of proximal nail plate of left side treated with combined therapy when compared with right side treated with single therapy at 12 wk. C: Significant improvement of left nail at final follow-up when compared with right side

- A. Picture showing both toe nails dystrophic before study. B. Appreciable improvement of left nail treated with combined therapy. C. Almost normal nail on combined treatment side at final follow-up visit
Out of the 25 pairs of toe nails included in our study, 8 pairs of toes had anonychia and each nail had an NDGS of 5 and no appreciable improvement or regrowth of nail plate was seen at the end of study after giving single or combination therapy.
According to the physician global assessment, in finger nails, good response was seen in 13 (50%) nails, moderate response in nine (34.6%) nails, and poor response in four (15%) nails in the combined therapy group (FN-T + P), whereas in the single therapy group (FN-T), good response was seen in three (11.5%) nails, moderate response in 10 (38.4%) nails, and poor response in 13 (50%) nails. The difference between these two finger nail treatment groups is statistically significant (P = 0.001) [Figure 4]. Similarly, in toe nails, out of the 25 nails on each side, good response was seen in 12 (48%) nails, moderate response in four (16%) nails, and poor response in nine (36%) nails in the combined therapy group (TN-T + P), whereas in the single therapy group (TN-T), good response was seen in three (12%) nails, moderate response in six (24%) nails, and poor response in 16 (64%) nails. The difference between the two treatment groups of toe nails being statistically significant (P = 0.004) [Figure 4].
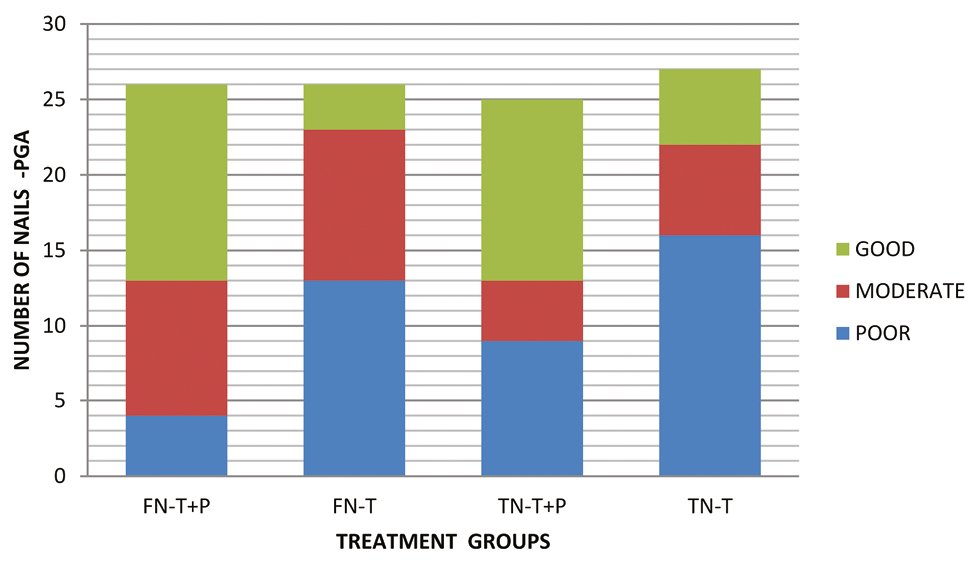
- Chart depicting number of nails according to the physician global assessment
According to the patient satisfaction score, in the combined therapy group irrespective of hand or feet, more numbers of patients, nine (64%), were very satisfied, three (21.4%) were satisfied, and two (14.3%) were slightly satisfied. There was no patient from the combination group who was least satisfied. However, in the single therapy group, only one (7%) patient was very satisfied followed by two (14.2%) patients who were satisfied, four (28.5%) patients slightly satisfied, and more number of patients, seven (50%), were least satisfied. The difference between the two treatment groups is statistically significant (P < 0.001) [Figure 5].
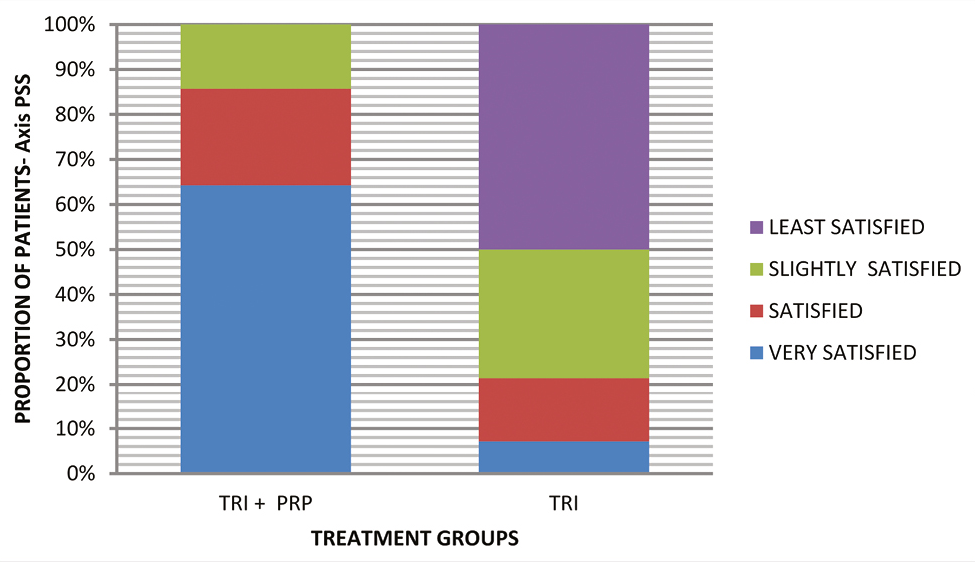
- Chart depicting number of patients according to the patient satisfaction score
DISCUSSION
It is always a challenge to treat a patient with nail dystrophy. The most common therapy is the injection of triamcinolone acetonide into the nail matrix.[16] Although it seems to be an effective one, various side effects such as injection site atrophy, disappearance of the phalanx under injection, or tendon rupture were also described.[1718]
In our study, according to the self-designed NDGS, there was statistically significant difference in the mean initial and final average grades of the fingers as well as toe nails among the patients receiving intramatricial PRP along with triamcinolone when compared with triamcinolone alone (P < 0.001 and =0.002, respectively).
Moreover, we noted better results in finger nails among the patients receiving PRP along with triamcinolone and 50% of them show “good response” when compared with 11.5% of the patients who received only intramatricial steroid, and the physician global assessment between the groups was statistically significant (P = 0.001). Similar results were seen in the patients receiving combined therapy in toe nails where 48% of them show good response when compared with 12% in the single therapy group, indicating that clinical improvement was better on the PRP-treated site.
Also according to the patient satisfaction score, among the patients receiving combined therapy, i.e. PRP along with triamcinolone irrespective of finger or toe involvement, 64% were “very satisfied” and no patient (0%) was “least satisfied” when compared with the single therapy group in which 7% and 50% of the patients were seen in the “very satisfied” and “least satisfied” groups indicating that patients receiving intramatricial PRP also were more satisfied with the outcome of combination therapy.
The PRP contains various bioactive molecules such as mitogenic and chemotactic growth factors released from the alpha (α) granules of activated platelets: platelet-derived growth factors (PDGFs), transforming growth factor-β1 (TGF-β1), TGF-β2, vascular endothelial growth factor (VEGF), basic fibroblast growth factor (bFGF), and epithelial growth factor (EGF).[1920] These constituents have a role in tissue repair and other cellular events through the upregulation of genes responsible for cellular proliferation and differentiation, angiogenesis, tissue regeneration, and extracellular matrix synthesis.[21222324252627] In particular, among growth factors, PDGF and TGF-β play critical roles in the regeneration. TGF-β is a potential cytokine involved in the control of cell growth, stimulation of matrix production, and suppression of the immune system[28]
The statistically significant response of inflammatory nail disorder to the combination therapy of triamcinolone and PRP in our study can also be attributed to the anti-inflammatory action of PRP. The anti-inflammatory action of PRP is mediated by two main inflammatory mediators: hepatocyte growth factor (HGF) and tumor necrosis factor alpha (TNF-α) which not only disrupt the NF-kB transducing pathway, which is a critical regulator of the inflammatory cascade, but also reduce the chemotaxis of monocytic cells by inhibiting chemokine transactivation and CXCR-4 receptor expression.[29]
α-granules of platelets release a significant amount of Regulated on Activation Normal T Expressed and Secreted (RANTES) that inhibits cytokine release of basophils and results in resolution of inflammation, which in turn decrease the number of inflammatory cells.[30]
Also in our study, no improvement in eight pairs of anonychia toe nails can be hypothetically attributed to the unresponsiveness of completely and/or permanently damaged nail matrix due to the inflammatory process of growth promoting factors of PRP.
In the literature, we found only two cases of nail dystrophy reported by Kaur and Jakhar[11] in which nails showed marked improvement to intramatricial PRP. However, we could not find any study evaluating the result of combination of steroid and PRP in nail dystrophy. The role of PRP has been already used and studied in the field of dermatology. Its role in acne scars, skin rejuvenation, ulcer healing, and different kinds of alopecia has been attributed to growth factors released from platelets upon activation.[31323334]
Due to this anti-inflammatory response, PRP is being used as cost-effective and high result-yielding modality of treatment in other fields, e.g. Orthopedics, Dentistry, Surgery, etc. In Orthopedics, it has shown promising result in tendinopathies and osteoarthritis.[3536373839] Also the statistically significant decrease in the lymphocyte concentration has been shown after injecting PRP treatment in the periodontal pocket in patients of chronic periodontitis.[40] Steroids in combination with PRP have also been promoted as good therapeutic modality in tendon and extremity joint degenerative and inflammatory diseases.[41]
In our study, side effects to intramatricial injection were almost similar between the combination therapy group and single treatment group and included pain during procedure and subungal hematoma but in two patients subungal hematoma resolved faster in PRP-treated nails.
CONCLUSION
In our study, the combination therapy of intramatricial PRP and steroids did alter the final outcome significantly when compared with steroids alone. However, at the end of the study, we did not observe any improvement or nail growth in eight toes and anonychia of more than 1-year duration was present. So more large-scale studies are needed to evaluate the beneficial effect of PRP and its role as early intervention in this appendageal disorder which has significant aesthetic appeal.
Limitations
Our study included less sample size.
Blinding could not be done in patients.
Histopathological documentation and onychoscopic/dermoscopic evaluation were not done.
Further follow-up to denote relapse was not done.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
REFERENCES
- Onychodystrophy and its management. Ger Med Sci. 2003;1:Doc02. Published 1 Jul 2003
- [Google Scholar]
- Update on lichen planus and its clinical variants. Int J Womens Dermatol. 2015;1:140-9.
- [Google Scholar]
- A compendium of intralesional therapies in nail disorders. Indian Dermatol Online J. 2018;9:373-82.
- [Google Scholar]
- Insights into drug delivery across the nail plate barrier. J Drug Target. 2014;22:769-89.
- [Google Scholar]
- Intramatricial injections for nail psoriasis: An open-label comparative study of triamcinolone, methotrexate and cyclosporine. Indian J Dermatol Venereol Leprol. 2018;84:419-23.
- [Google Scholar]
- Intralesional injection for inflammatory nail diseases. Dermatol Surg. 2016;42:257-60.
- [Google Scholar]
- Efficacy of triamcinolone acetonide in various acquired nail dystrophies. J Dermatol. 2005;32:963-8.
- [Google Scholar]
- Intramatricial platelet-rich plasma therapy: A novel treatment modality in refractory nail disorders. Dermatol Therapy. 2019;32:e12831.
- [Google Scholar]
- Naildex: Pilot evaluation of an onychodystrophy severity instrument. Mycoses. 2008;51:14-20.
- [Google Scholar]
- A comparative study of combined dermaroller and platelet-rich plasma versus dermaroller alone in acne scars and assessment of quality of life before and after treatment. Indian J Dermatol. 2018;63:403-8.
- [Google Scholar]
- Enhanced effect of platelet-rich plasma containing a new carrier on hair growth. Dermatol Surg. 2011;37:1721-9.
- [Google Scholar]
- Growth rate of human fingernails and toenails in healthy American young adults. J Eur Acad Dermatol Venereol. 2010;24:420-3.
- [Google Scholar]
- Role of nail bed methotrexate injections in isolated nail psoriasis: Conventional drug via an unconventional route. Clin Exp Dermatol. 2017;42:420-3.
- [Google Scholar]
- Nail psoriasis successfully treated with intralesional methotrexate: Case report. Dermatology. 2011;222:5-7.
- [Google Scholar]
- Psoriasis of the nail: Anatomy, pathology, clinical presentation, and a review of the literature on therapy. J Am Acad Dermatol. 2007;57:1-27.
- [Google Scholar]
- Platelet genomics and proteomics in human health and disease. J Clin Invest. 2005;115:3370-7.
- [Google Scholar]
- Histologic evidence of new collagen formulation using platelet rich plasma in skin rejuvenation: A prospective controlled clinical study. Ann Dermatol. 2016;28:718-24.
- [Google Scholar]
- Effect of platelet rich plasma on ultraviolet b-induced skin wrinkles in nude mice. J Plast Reconstr Aesthet Surg. 2011;64:e31-9.
- [Google Scholar]
- The healing effects of autologous platelet gel on acute human skin wounds. Arch Fac Plast Surg. 2007;9:174-83.
- [Google Scholar]
- Platelet-rich plasma: Evidence for the treatment of patellar and Achilles tendinopathy—A systematic review. Musculoskelet Surg. 2015;99:1-9.
- [Google Scholar]
- A systematic review and meta-analysis of the application of platelet rich plasma in sports medicine. Electron Phys. 2016;8:2325-32.
- [Google Scholar]
- Systematic review of the use of platelet-rich plasma in aesthetic dermatology. J Cosmet Dermatol. 2015;14:315-23.
- [Google Scholar]
- Additive effect of autologous platelet concentrates in treatment of intrabony defects: A systematic review and metaanalysis. J Investig Clin Dent. 2016;7:13-26.
- [Google Scholar]
- Platelet-rich plasma: Quantitative assessment of growth factor levels and comparative analysis of activated and inactivated groups. Arch Plast Surg. 2013;40:530-5.
- [Google Scholar]
- Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: Mechanisms of NF-κB inhibition via HGF. J Cell Physiol. 2010;225:757-66.
- [Google Scholar]
- Platelet-rich plasma: Growth factors and pro- and anti-inflammatory properties. J Periodontol. 2007;78:661-9.
- [Google Scholar]
- Platelet-rich plasma and its utility in the treatment of acne scars: A systematic review. J Am Acad Dermatol. 2019;80:1730-45.
- [Google Scholar]
- A systematic review of the safety and effectiveness of platelet-rich plasma (PRP) for skin aging. Arch Dermatol Res. 2020;312:301-15.
- [Google Scholar]
- Effectiveness of platelet-rich plasma for androgenetic alopecia: A review of the literature. Skin Appendage Disord. 2018;4:1-11.
- [Google Scholar]
- Platelet-rich plasma in androgenic alopecia: Myth or an effective tool. J Cutan Aesthet Surg. 2014;7:107-10.
- [Google Scholar]
- HGF mediates the anti-inflammatory effects of PRP on injured tendons. PLoS One. 2013;8:e67303.
- [Google Scholar]
- Platelet-rich plasma as a treatment for patellar tendinopathy: A double-blind, randomized controlled trial. Am J Sports Med. 2014;42:610-8.
- [Google Scholar]
- Platelet-rich plasma: Current concepts and application in sports medicine. J Am Acad Orthop Surg. 2009;17:602-8.
- [Google Scholar]
- Efficiency of platelet-rich plasma therapy in knee osteoarthritis does not depend on level of cartilage damage. J Orthop Surg Res. 2019;14:153.
- [Google Scholar]
- Platelet-rich plasma combined with decalcified freeze-dried bone allograft for the treatment of noncontained human intrabony periodontal defects: A randomized controlled split-mouth study. Int J Periodont Restorative Dent. 2014;34:705-11.
- [Google Scholar]
- The anti-inflammatory effect of the platelet-rich plasma in the periodontal pocket. Eur J Dent. 2018;12:528-31.
- [Google Scholar]
- Anaesthetics, steroids and platelet-rich plasma (PRP) in ultrasound-guided musculoskeletal procedures. Br J Radiol. 2016;89:20150355.
- [Google Scholar]






