Translate this page into:
Intralesional drug delivery with a bent needle
*Corresponding author: Sharad D. Mutalik, Department of Dermatotherapy and Cosmetology, Maharashtra Medical Foundation’s Joshi Hospital, Shivajinagar, Opposite Kamala Nehru Park, Pune, Maharashtra, India. planetskinpune@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mutalik SD, Rasal YD. Intralesional drug delivery with a bent needle. J Cutan Aesthet Surg. 2024;17:348-50. doi: 10.4103/JCAS. JCAS_38_23
Abstract
Intralesional injections to wide, thick lesions and lesions on curved surfaces are challenging with the syringe and needle unit being held parallel to the skin surface. Bending the needle eases negotiation by lifting the syringe away from the skin surface with the needle entering parallel to the lesion ensuring uniform and optimal drug delivery.
Keywords
Hypodermic needle
Intralesional injection
Drug delivery
INTRODUCTION
Intralesional injection delivers a high concentration of medicine into the site of pathology to maximize efficacy while minimizing systemic adverse effects of the drug. The most common medication used for intralesional injection is a corticosteroid (e.g. triamcinolone acetonide) or other drugs such as 5-fluorouracil, bleomycin, methotrexate, etc. Superficial administration can lead to local pain, inflammatory reaction, and rarely infection, while a subcutaneous injection may cause deep tissue injury, hypopigmentation, hyperpigmentation or atrophy. The authors propose a simple modification to the injection technique in order to facilitate uniform intralesional drug delivery at the desired level of affected tissue.
LEARNING POINTS
Intralesional injections to wide thick lesions and lesions on curved surfaces pose a challenge for optimal drug delivery.
Easy negotiation is achieved by bending the needle.
This ensures the needle enters the lesion parallel to the skin surface while the syringe is lifted away providing easy maneuverability.
Bending the needle delivers the drug uniformly at the desired level.
Optimal drug delivery through intralesional injection requires piercing the lesion at an appropriate depth. Injection with a straight hypodermic needle and syringe held parallel to the skin surface poses a challenge, particularly in cases of wide, thick lesions, or locations on curved surfaces. If the syringe is held at an angle of 30°–45° to the skin surface, the drug is neither delivered uniformly nor at the desired depth.
The authors have developed a modified injection technique by using a bent hypodermic needle in order to make the needle entry smoother and movement easier facilitating optimal drug delivery.
This innovation certainly helps in thick skin lesions such as chronic lichenified eczema, prurigo nodularis, recalcitrant plaques of psoriasis, and keloids over difficult-to-treat sites like curved surfaces of the body.
24 or 25 gauge × 1–1.5 inches straight steel needle is bent just above the hub at the required angle. Bending the needle is easily achieved by gentle manipulation with artery forceps with force just enough to angulate the needle without breakage or functional loss.1-3 The needle is bent for approximately 30°–40°. Inserting this needle parallel to the lesions deflects the syringe body equally, lifting it away from the body surface. As a general principle and practice, the needle is bent with the beveled side up (similar to filler delivery) for easy insertion, avoidance of injury, and controlled drug release into the tissue in a horizontal fashion.
With this modification, the syringe is no longer parallel to the lesion but is lifted away from the surface allowing easier negotiation with lesser effort giving ergonomic ease to the injector [Figures 1-3]. As the hypodermic needle remains parallel to the skin surface, the drug is delivered uniformly at the same anatomical plane/depth, which helps in achieving a uniform reduction in the thickness of the lesion.
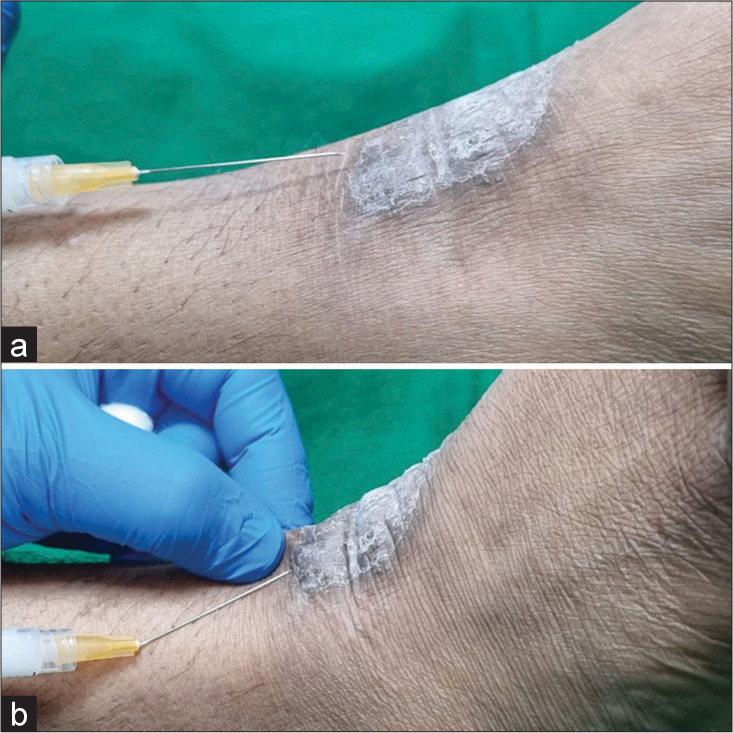
- (a) Difficult navigation for intralesional injection for a chronic lichenified lesion over a curved ankle surface with a straight needle. (b) Ergonomic ease for intralesional drug delivery with a bent needle for the same lesion.

- Presternal keloid injected with a bent needle (note the parallel orientation of the needle with the skin surface and lifted up a syringe).

- Hypertrophic scar on cheek injected with a bent needle.
CONCLUSION
Intralesional injection is a common and effective dermatologic procedure for the treatment of various skin conditions. If the needle is bent at the hub, it helps easy and smooth entry without causing any hindrance to the syringe barrel especially when negotiating at curved surfaces. This simple modification in injection technique makes the procedure easy without causing any resistance and perfect delivery of the medication.
Authors’ contributions
Both the authors’ equally contributed to the research study. Sharad D. Mutalik: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Yashashree Dhaval Rasal: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal.
The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Assessment of conduction anesthesia effectiveness using the angulated needle approach for the inferior alveolar nerve block. J Craniomaxillofac Surg. 2020;48:607-15.
- [CrossRef] [PubMed] [Google Scholar]
- Uses of hypodermic needle in dermatology. Indian J Dermatol Venereol Leprol. 2013;79:721-4.
- [CrossRef] [PubMed] [Google Scholar]
- The biomechanics and optimization of the needle-syringe system for injecting triamcinolone acetonide into keloids. J Med Eng. 2016;2016:5162394.
- [CrossRef] [PubMed] [Google Scholar]






