Translate this page into:
Intralesional Vitamin D3 Versus Bleomycin for Difficult-to-Heal Palmoplantar Warts: A Comparative Study
Address for correspondence: Dr. Jantikolalu Parameswarappa Prathibha, Department of Dermatology, St John’s Medical College Hospital, Bangalore 560034, India. E-mail: prathibha.jp@stjohns.in
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Difficult-to-heal or recalcitrant palmoplantar warts are notoriously resistant to treatment, making treatment difficult and challenging. To improve the outcome and overcome the difficulties, various treatment options have been tried, but none is gold standard. Many comparative studies have been undertaken to assess the efficacy of various drugs; however, none of them are standardized, and no single treatment is effective. Various comparative efficacy studies have been conducted but, to the best of our knowledge, no study has been conducted comparing intralesional (IL) injection (inj) vitamin D3 (Vit D3) with the chemotherapy drug IL inj Bleomycin for difficult-to-heal palmoplantar warts. We conducted a trial to evaluate the efficacy of IL inj Vit D3 versus IL inj Bleomycin in the treatment of difficult-to-heal palmoplantar warts. The purpose of this study was to compare the efficacy of IL inj vitamin D3 versus IL inj Bleomycin as biological response modifier therapy in difficult-to-heal palmoplantar warts.
Materials and Methods:
A cohort of 48 patients with difficult-to-heal warts were consecutively assigned to one of two groups: Group 1 IL inj Vit D3 (0.2–0.5 mL inj vitamin D3 600,000 IU solution 15 mg/mL) or Group 2 IL inj Bleomycin (0.2–0.4 mL of 1 U/mL solution) for a maximum of four treatments spaced 2 weeks apart, with a maximum of five warts treated at each visit for both groups. Warts were measured at baseline and at each subsequent visit. Wart’s resolution was measured as 1–25%, 2–50%, 3–75%, and 4–100% reduction. Patients were followed-up for 3 months after treatment.
Results:
All the 48 patients completed the study, with 26 receiving IL inj Vit D3 with complete resolution in 88.5%, partial resolution in 11.5%, and side effects in 6.2%. In 22 patients receiving IL inj Bleomycin, 95.5% had complete resolution, 4.5% had partial resolution, and 8.2% had side effects. Maximum resolution was observed in the third session. We found no recurrence after 3 months.
Conclusion:
IL inj Vit D3 and IL inj Bleomycin are both safe and effective in treating difficult-to-heal palmoplantar warts with better outcomes and patient satisfaction. IL Bleomycin was significantly more effective than IL Vit D3, although the difference was not statistically significant.
Keywords
Bleomycin
difficult-to-heal wart
intralesional
palmoplantar wart
recalcitrant wart
INTRODUCTION
Treating warts that are difficult-to-heal is tedious and challenging for a dermatologist because they are resistant to conventional treatments. Although a spontaneous resolution of warts is observed in 65–78% of cases,[1] one-third of cases do not resolve and instead become highly resistant or recalcitrant, particularly on the palms, soles, and periungual regions.[2] Recalcitrant or difficult-to-heal warts could indicate a localized or systemic Human Papilloma Virus (HPV) related cell-mediated immune (CMI) deficiency. Various explanations have been proposed, including lack of memory-T cells to target HPV infection, failure to effectively induce lymphocyte clonal expansion, T-lymphocytes’ reluctance to go to infection sites, and a poor effector response mechanism. As a result, warts are frequent in patients who have had organ transplants, Hodgkin’s disease, acquired immunodeficiency syndrome, or those taking immunosuppressive drugs.[1] There are numerous treatment options for warts, but there are no set guidelines for the treatment of difficult-to-heal warts. Intralesional (IL) immunotherapy or biological response modifier has gained popularity not only for its effectiveness in clearing warts locally, but also provides advantage of clearance of wart at distant sites by stimulating cell-mediated immunity.[3]
To the best of our knowledge, no study has been undertaken comparing IL injection (inj) vitamin D3 (Vit D3) with the chemotherapeutic agent IL inj Bleomycin for difficult-to-heal palmoplantar warts. In this study, we evaluated the safety and efficacy of IL inj Vit D3 to IL Bleomycin in the treatment of difficult-to-heal palmoplantar warts.
The goal of this study was to assess the efficacy of IL inj Vit D3 versus IL inj Bleomycin in difficult-to-heal palmoplantar warts.
MATERIALS AND METHODS
The trial was conducted in Out Patient Department of Department of Dermatology, Venereology and Leprology of a tertiary care teaching hospital. The study was approved by the Institutional Ethical Committee (IEC Ref. No. 169/2018). Warts that are difficult-to-heal are those that have not resolved despite several therapeutic options. Difficult-to-heal warts are those that did not reduce or reduce by <50% of mean percentage in size, after at least three consecutive selected treatment options. Following a thorough clinical history and examination, patients with difficult-to-heal palmoplantar warts were diagnosed and men and women above 18 years of age were enrolled into the study after obtaining a proper written informed consent. Pregnant females, lactating mothers, children, and those >60 years, immunocompromised individuals, ulcerated and inflamed warts, and patients with peripheral vascular disease were excluded. Sixty-eight patients who met the above inclusion criteria were enrolled. A total of 20 of them either lost to follow-up or discontinued the intervention either because of pain or reasons not mentioned. The CONSORT flow diagram of patient is shown in Figure 1. Baseline evaluation was made at first visit, and demographic data were recorded. For each patient, location, number, size of difficult-to-heal warts were recorded.
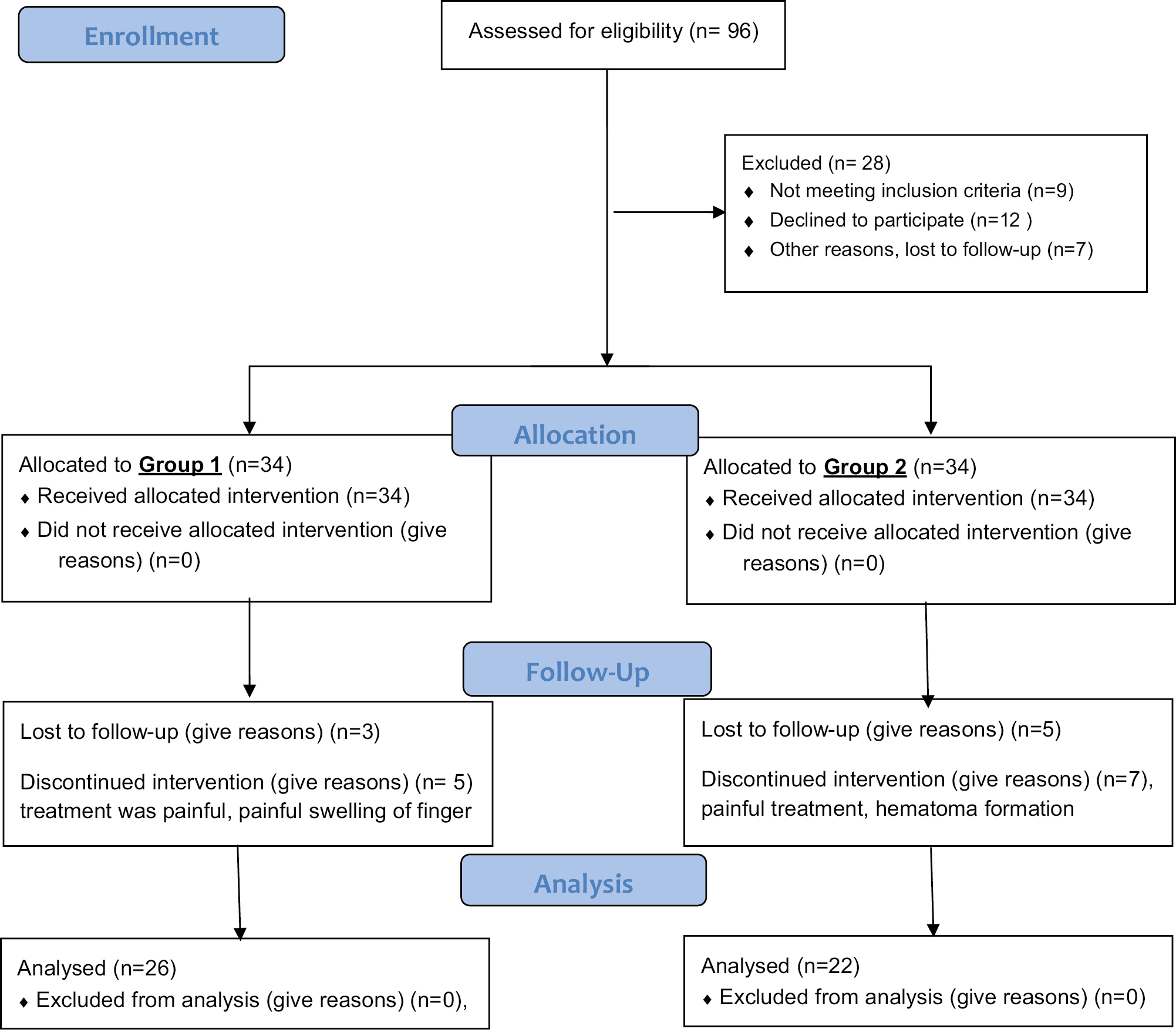
- CONSORT statement
Patients were consecutively assigned to either group 1 IL Vit D3 (0.2–0.5 mL) or group 2 IL inj Bleomycin (1 U/mL).
Group 1: Inj Vit D3 (vitamin D3 injection Arachitol-6L® is available in ampoules containing 600,000 IU of aqueous preparation of cholecalciferol in the dose of 15 mg/mL) after scraping the wart surface and after injecting 2% lidocaine (20 mg/mL), Inj Vit D3 (0.2–0.5 mL) small warts received 0.1–0.2 mL of solution, while larger warts received 0.3–0.5 mL injected into the base of the wart until it blanched, with the largest wart receiving the highest dose. At each session, the total volume injected was limited to 7.5 mg of Inj Vit D3. Group 2: IL Inj Bleomycin vial of 15 U was diluted with 5 mL of distilled water to prepare stock solution (each mL containing 3 U). This could be stored for 60 days at 2–8°C. At the time of treatment session, two parts of lidocaine 2% and one part of the Bleomycin stock solution were taken in a 1 mL syringe, thus using a final solution of 1 U/mL of Bleomycin. After scraping the wart, and after injecting 2% lidocaine (20 mg/mL) freshly prepared IL inj Bleomycin 0.2–0.4 of 1 U/mL solution was injected to the base of the wart, until it blanched. In a single treatment session, the total volume injected was limited to 2 mL. Up to five difficult-to-heal warts were treated during each session, for a maximum of four treatments sessions spaced two weeks apart, for both groups. Patients were followed-up to 3 months after compete resolution. Clinical response, decrease in size, number of lesions, and adverse reactions were recorded at each visit. The enrolled patients were advised not to use any other wart treatment during the study period. Signs and symptoms of hypervitaminosis D, if any, were noted. At each visit, the total number of warts and each/individual difficult-to-heal wart treated and improved, were assessed. The subjective evaluation of the treatment’s effectiveness of each wart was graded based on the reduction of the size of the lesions as follows: 0 – no reduction, 1 – 25%, 2 – 50%, 3 – 75%, and 4 –100% reduction, treatment was considered a failure if the size of the warts did not decrease or reduced by at least by 50% after three consecutive treatments with either Inj Vit D3 or Inj Bleomycin. Serial photographs were taken at each visit to support the recorded data.
Descriptive statistics was reported as mean and standard deviation, median with 25th and 75th percentiles, number, and percentages. The respective median percentages of reduction in lesion were compared between vitamin D3 and Bleomycin groups using Mann–Whitney U test. Wilcoxon signed rank test was used to compare the change in reduction from baseline to each visit. The percentage of reduction categories were compared between the two study groups, using χ2 test. P value < 0.05 was considered statistically significant. Analyses were carried out using SPSS version 25.0.
RESULTS
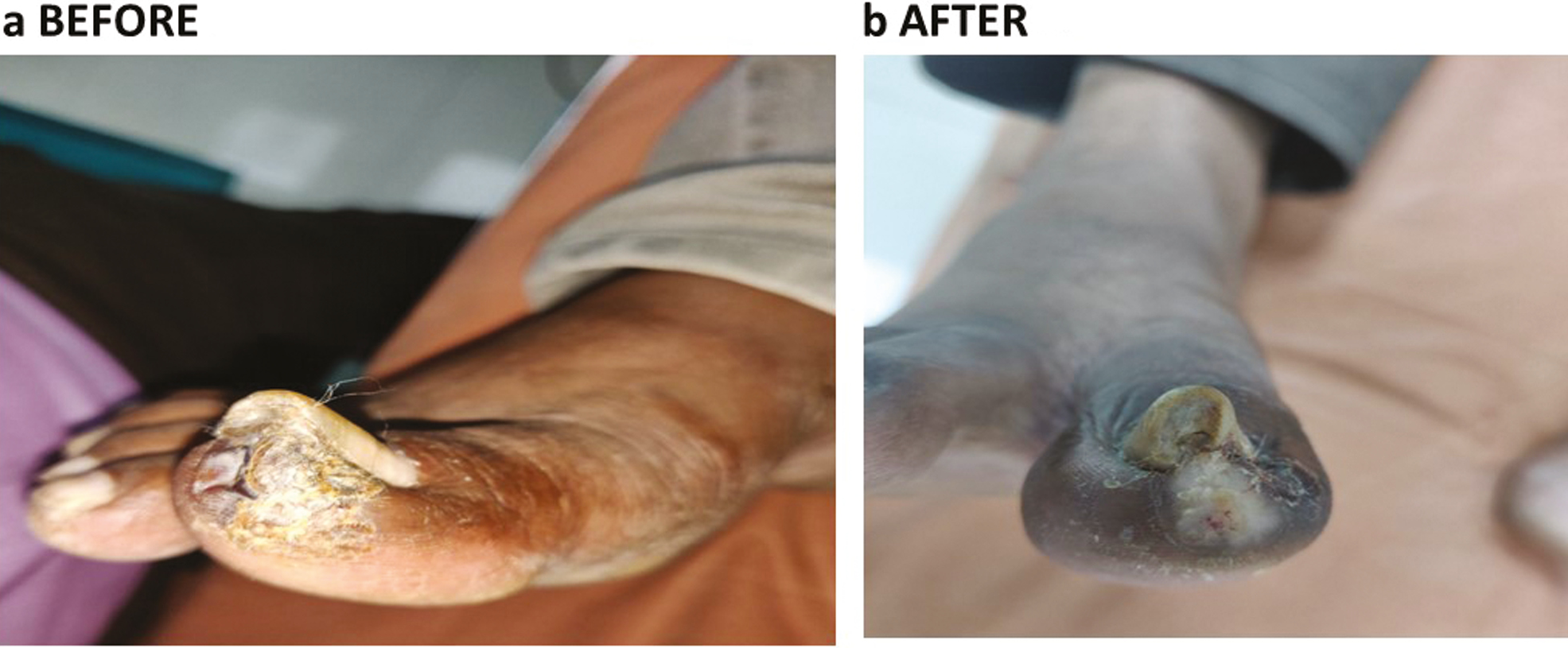
In the current research, there were no statistically significant differences between the two study groups with respect to gender, age, history of lesions, duration, and number of lesions [Table 1]. In the IL inj Vit D3 group, 26 patients completed the course of the treatment. Age of the patients ranged from 18 to 40 years, mean age being 26.2 years. Eighteen (69.2%) of them were males and 8 (30.8%) were females. Duration of difficult-to-heal warts ranged from 2 to 24 months, with an average of 6.6 months. The number of warts varied from 1 to 10, with an average of 2.96. Fifteen (57.7%) of them had warts on palms, 10 (38.5%) on soles, and 1 (3.8%) on both palms and soles. Two (7.7%) had received purified protein derivative (PPD) earlier, 12 (46.2%) cryotherapy, 11 (42.3%) electro surgery, and 1 (3.8%) had undergone auto-inoculation before enrollment. Twenty three (88.5%) patients showed complete resolution [Figures 2a, b, 3a, b]; whereas 3 (11.5%) showed partial solution. Adverse effects such as pain and swelling at the injection site was noticed in two patients (7.7%) which was managed by nonsteroidal anti-inflammatory drugs. None of the patients developed allergic reactions, systemic adverse reaction or signs, and symptoms of hypervitaminosis D. None of them had recurrence during 3 months follow up.
| IL Vit D | IL Bleomycin | P value | |
|---|---|---|---|
| No. of patients | 26 | 22 | |
| Age (years) | 18–40 | 20–43 | 0.146 |
| Mean age (years) | 26.2 | 28.9 | |
| Gender | |||
| Male | 18 (69.2%) | 16 (72.7%) | 0.791 |
| Female | 8 (30.8%) | 6 (27.3%) | |
| Site of lesions | |||
| Palm | 15 (57.7%) | 13 (59.1%) | |
| Palmoplantar | 1 (3.8%) | 1 (4.5%) | |
| Plantar | 10 (38.5%) | 8 (36.4%) | |
| Duration (months) | 2-24 | 2-120 | 0.042 |
| 6.68 months | 17.1 months | ||
| No. of lesions | 2.5–10 | 2–11 | 0.279 |
| 2.96 (±2.66) | 3.67 (±2.79) | ||
| Previous treatment | |||
| PPD | 2 (7.7%) | 9 (40.9%) | |
| Cryo | 12 (46.2%) | 9 (40.9%) | |
| EC | 11 (42.3%) | 3 (13.6%) | |
| Autoinoculation | 1 (3.8%) | 1 (4.5%) | |
| Complete resolution | 23 (88.5%) | 21 (95.5%) | 0.6 |
| Partial resolution | 3 (11.5%) | 1 (4.5%) | |
| Adverse effects | |||
| Pain | 100% | Pain 100% | |
| Swelling 7.7% | Swelling hematoma 8.2% | ||
| Distant resolution | No | No | |
| Recurrence | No | No | |

- (a, b) Plantar wart before IL Vit D3 treatment. Complete resolution after three sessions of IL Vit D3

- (a, b) Palmar wart before IL Vit D3 treatment. Complete resolution after four sessions of IL Vit D3
In the IL Bleomycin group, 22 patients completed the study. Age of patients ranged from 20 to 43 years, with a mean age of 28.9 years. Sixteen (72.7%) of them were male and 6 (27.3%) were female. The duration of warts ranged from 2 to 120 months, with an average of 17.1 months. The number of the warts varied from 1 to 11, with an average of 3.67. Thirteen (59.1%) had warts on palms, 8 (36.4%) on soles and 1 (4.5%) on both palms and soles. Nine (40.9%) had received PPD, 9 (40.9%) cryotherapy, 3 (13.6%) electro surgery and 1 (4.5%) had auto-inoculation before enrollment. Twenty one (95.5%) patients showed complete resolution [Figures 4a, b, 5a, b]; whereas 1 (4.5%) patient showed partial resolution. Pain was seen in all; only 2 (8.2%) patients had complications such as eschar, painful swelling erythema, and hematoma [Table 1]. None of them developed Raynaud’s phenomena, allergic reactions or systemic adverse reactions. None of them had recurrence during 3 months follow-up.
- (a, b) Plantar wart before IL Bleomycin, same wart after 4 months of IL Bleomycin
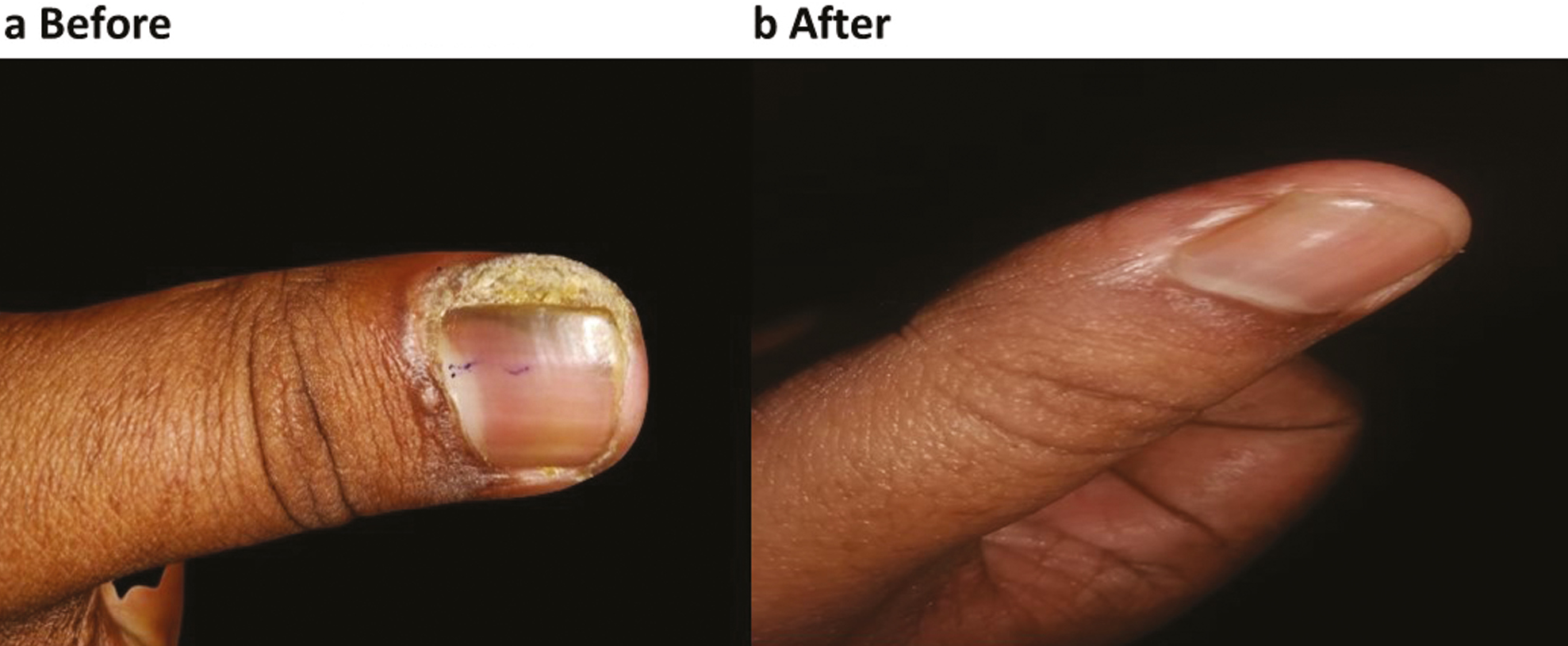
- (a, b) Periungual wart before and after 4 months of IL Bleomycin
DISCUSSION
Currently, there is no universally accepted definition for difficult-to-heal or recalcitrant warts. One of them defines them as warts that do not reduce or reduce <50% of mean percentage in size, after at least three consecutive treatment sessions.[3] Recalcitrant warts have historically been difficult to cure because they frequently recur and relapse. Destructive, immunological, and cytotoxic medicines are all used to treat recalcitrant warts.[4] Difficult-to-heal warts are refractory to treatment with high recurrence rates. Various explanations have been proposed, including a lack of memory-T cells to target HPV infection. This could result from a failure of lymphocyte clonal expansion to adequate stimulation, inability of T lymphocytes to traffic to infection sites, and a poor effector response mechanism.[3] Contumacious nature of warts may be due to localized or systemic HPV-related CMI deficiency. Low interleukin-17 and zinc deficiency and low serum retinol binding protein have a role in the pathogenesis of recalcitrant warts, through the imbalance of immune system and deficiency of immune cells.[56] More research is needed to back up this argument. Aktas et al. used intralesional Vit D3 injection for the first time to treat palmoplantar warts and reported favorable outcomes.[7] IL Vit D3 has been used successfully in other studies for recalcitrant warts, with the efficacy of 90%.[891011] The exact mechanism of Vit D3 activity against warts is not completely understood. Vit D3 regulates/modulates innate immunity by enhanced production of Defensin B2 and Cathelicidin antimicrobial peptide by macrophages, monocytes, and keratinocytes, thereby increasing their antimicrobial properties. It increases their chemotactic, autophagic, and phagocytic ability. Vit D through vitamin D receptor (VDR) promotes antigen presenting cells (dendritic cells) to increase the levels of anti-inflammatory cytokine IL-10 and also induces differentiation of T-reg cells to induce apoptosis. Vit D3 has the ability to regulate proliferation and differentiation of epidermal cells and modulation of cytokine production.[12] As a response, viral infected keratinocytes are eliminated. Bleomycin is a mixture of glycopeptide anti-neoplastic antibiotics isolated from the bacterium Streptomyces verticillus. Bleomycin has an antitumor, antibacterial, and antiviral activity. Bleomycin is an anti-neoplastic drug that inhibits DNA metabolism and is used in various skin conditions such as hemangiomas, vascular malformations, leishmania cutis, and several cutaneous malignancies.[13] Numerous reports have published the use of IL Bleomycin in the treatment of recalcitrant warts, with success rates ranging from 14% to 99%.[1415] IL injection of Bleomycin interferes with DNA synthesis, thereby causing acute necrosis of the wart tissue.[16]
In our study, a systematic transition to intralesional injections was able to elicit an immune response in patients who had failed to respond to other therapies including cryo, electrocautery, PPD, etc. Table 2 compares the outcome of our study to those of previous studies in the treatment of difficult-to-heal palmoplantar warts with IL Vit D3. It was interesting to notice more resilient and difficult-to-heal warts on the hands 28 (59.6%) than on the soles 18 (36.7%) or on both palmoplantar 2 (4%) regions, indicating constant trauma and friction during daily routine work, which could lead to auto-inoculation and pseudo-Koebner response, making them resistant to treatment. Complete clearance of difficult-to-heal palmoplantar warts was comparable to Priya et al., findings.[10] The average number of sessions necessary to eliminate warts was three sessions, which was also noted in other research.[810] Most of the adverse effects had pain (100%), while swelling was observed in two (7.7%) of the patients, which was higher than Raghukumar et al.’s 3.3% but lower than Priya et al.’s 25.4%. Over the three-month follow-up period, none of them experienced recurrence.
| Studies | Raghukumar et al.[6] | Fathy et al.[7] | Priya et al.[8] | Raveendra et al.[9] | Our study |
|---|---|---|---|---|---|
| Mean duration of wart | 14.12 months | 21.14 months | 1.47 ± 1.19 yrs | 7.3 months | 6.68 months |
| Dose of Vit D3 | 0.2–0.5 mL of vitamin D3 (600,000 IU; 15 mg/mL) | 0.6 mL 60,000 IU | 0.2–0.5 mL of vitamin D3 (15 mg/mL) | 0.1 mL | 0.2–0.5 mL Vit D3 600,000 IU, 7.5 mg/mL |
| Number of warts injected | 5 | Largest wart | 4 | 10 | 5 |
| Number of treatment sessions | 4 | 3 | 4 | 4 | 4 |
| Interval between the sessions | 3 | 3 | 2 | 2 | 2 |
| Average number of sessions for complete resolution | 3.66 | 3.05 | NM | 3 | |
| Complete resolution | 90% | 70% | 88.90% Periungual 92.9% Palmar 90% Plantar 86.6% |
94% | 88.50% |
| Partial resolution | 6.66% | 30% | 11.10% | 6% | 11.50% |
| Adverse effects | 3.33% Pain 100%, Edema 3.33%, Erythema 5% |
Pain | 3.2% Pain 100%, Local swelling 25.4% |
Minimal to moderate pain | Pain 100% Discoloration swelling 7.7% |
| Distant wart resolution | Yes | Yes | NM | Yes | No |
| Recurrence | 3.33% | 5% | 3.20% | 8% | None |
There are very few studies on the treatment of difficult-to-heal palmoplantar warts with Bleomycin.[151617181920]Table 3 compares the outcome of our study to those of others in the treatment of difficult-to-heal palmoplantar warts with IL Bleomycin. Complete clearance was reported in 95.5% of patients, which was similar to Shumer et al.’s finding of 94% after only two sessions of treatment, others reported 73–92%, which could be due to a lower number of sessions or a longer time between sessions. Average number of sessions for complete clearance was noticed in two sessions[1517,19] Adverse effects such as eschar formation and discoloration at the site of injection were seen in almost all our patients (100%). Swelling at the injection site lasting more than a week was seen in 8.2%, compared to 86% in the study by Aziz et al.[20] No systemic toxicity or Raynaud’s phenomenon was observed during study and follow-up period.[16] Recurrence was not seen in our study but recurrence was high in Aziz et al. which may be because of a smaller number of sessions. It was observed that warts which were larger in size and of longer duration were slower to resolve, and hence needed more sessions. This was also observed in the study by Singh et al. and Aziz et al.[1920] Partial response was noticed in all warts treated with both modalities of treatment. Distant warts in both groups had no response. After 3 months, no recurrence was observed. Both treatment modalities had almost comparable responses. Overall, 8.1% partial response of which 4.5% (n = 1) in the Bleomycin group and 11.5% (n = 3) in the IL Vit D3 group. IL inj Bleomycin was slightly better than IL inj Vit D3 in treating difficult-to-heal or recalcitrant palmoplantar warts; however, the difference was not statistically significant (P = 0.684).
| Bleomycin | Shumer et al.[12] | Agius et al.[18] | Mann et al.[14] | Aziz et al.[19] | Our study |
|---|---|---|---|---|---|
| Mean duration of warts | 6 months | 24 months | 24 months | 24 months | 17.1 months |
| Dose of Bleomycin | 1 mg/mL | 1 mg/mL | 1 mg/mL | 1 mg/mL | 1 mg/mL |
| Number of warts injected | Multiple | 20 | Multiple | Multiple | 5 |
| Number of treatment sessions | 2 | 5 | 1–12 | 3 | 4 |
| Interval between the sessions | 2 | 5 | 4 | 4 | 2 |
| Average number of sessions for CR | Only 2 sessions done | 3 | 4 | 2 | 3 |
| Complete resolution (CR) | 94% periungual and 60% plantar | 89.90% | 92% | 73% maximum of which were around the nail | 95.50% |
| Partial resolution | NM | 12.30% | 3% | 24% | 4.50% |
| Adverse effects | Pain, erythema and swelling | Pain, hematoma | Pain, Raynaud’s phenomena | Pain 86%, swelling, erythema | Pain 100% painful swelling, hematoma 8.2% |
| Distant Wart resolution | NM | NM | Yes | NM | No |
| Recurrence | None | 4.40% | 11% | 23% | None |
NM = not mentioned
The smaller sample size, short follow-up time, and lack of placebo as controls are the limitations of the study. For the treatment of difficult-to-heal palmoplantar warts, a standardized protocol would be required. A standardized protocol would be required for the treatment of difficult-to-heal palmoplantar warts.
CONCLUSION
Both IL Vit D3 and the chemotherapeutic medication IL Bleomycin were found to be safe and effective in the treatment of difficult-to-heal palmoplantar warts, with fewer post-procedure complications and a higher cure rate. IL Bleomycin produced marginally better outcome results than IL Vit D3; however, IL Vit D3 could be a beneficial alternative in resource-limited settings. To standardize intralesional therapy protocols for the treatment of difficult-to-heal palmoplantar warts, additional placebo-controlled randomized trials would be required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Immunomodulators in warts: unexplored or ineffective. Indian J Dermatol. 2015;60:118-29.
- [Google Scholar]
- Intralesional immunotherapy with purified protein derivative PPD for cryotherapy-resistant warts. Int J Dermatol. 2020;59:726-9.
- [Google Scholar]
- A comprehensive review of treatment options for recalcitrant nongenital cutaneous warts. J Dermatolog Treat. 2020;11:1-18.
- [Google Scholar]
- Evaluation of serum interleukin 17 and zinc levels in recalcitrant viral wart. J Cosmet Dermatol. 2020;19:954-9.
- [Google Scholar]
- Serum retinol-binding protein: a novel biomarker for recalcitrant cutaneous warts. Int J Dermatol. 2019;58:1435-8.
- [Google Scholar]
- Intralesional vitamin D injection may be an effective treatment option for warts. J Cutan Med Surg. 2016;20:118-22.
- [Google Scholar]
- Intralesional vitamin D3 injection in the treatment of recalcitrant warts: a novel proposition. J Cutan Med Surg. 2017;21:320-4.
- [Google Scholar]
- Intralesional vitamin D3 versus Candida antigen immunotherapy in the treatment of multiple recalcitrant plantar warts: a comparative case–control study. Dermatol Ther. 2019;32:e12997.
- [Google Scholar]
- Intralesional vitamin D3 in recalcitrant palmoplantar and periungual warts: a prospective, observational study. Acta Dermatovenerol Croatica. 2019;27:215-24.
- [Google Scholar]
- Comparison of purified protein derivative and vitamin D in the treatment of recalcitrant warts. Clin Dermatol Rev. 2021;5:54-8.
- [Google Scholar]
- Bleomycin in dermatology: a review of intralesional applications. Dermatol Surg. 2008;34:1299-313.
- [Google Scholar]
- The treatment of resistant warts with intralesional bleomycin: a controlled clinical trial. Br J Dermatol. 1984;111:197-207.
- [Google Scholar]
- A new method of intralesional bleomycin therapy in the treatment of recalcitrant warts. Br J Dermatol. 1996;135:969-71.
- [Google Scholar]
- Reduced dose of bleomycin in the treatment of recalcitrant warts. J Am Acad Dermatol. 1986;15:1002-6.
- [Google Scholar]
- Dermojet delivery of bleomycin for the treatment of recalcitrant plantar warts. J Dermatol Treat. 2006;17:112-6.
- [Google Scholar]
- Efficacy of intralesional bleomycin in the treatment of resistant warts. J Skin Stem Cell. 2014;1:e18875.
- [Google Scholar]
- A study on safety and efficacy of intralesionalvitamin D3 in cutaneous warts. Int J Res Dermatol. 2020;6:648-51.
- [Google Scholar]






