Translate this page into:
Keystone Flap for Postburn Finger Flexion Contracture Release
Address for correspondence: Dr. Ravi Kumar Chittoria, Department of Plastic Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry 605006, India. E-mail: drchittoria@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Flexion contracture of finger is a major cause of disability in postburn patients. Various methods have been described to cover the resultant defect after surgical release of finger flexion contracture. Local flaps are used when there is sufficient tissue available on lateral sides of the finger to recruit into the defect. Keystone flap can be designed on volar aspect of finger to cover the post contracture release defect. Use of local flap reduces need of skin graft and donor site morbidity. Here we discuss a case of postburn finger flexion contracture release using type-3 keystone flap. Postoperative results are satisfactory. Various pros and cons of the technique are discussed. Keystone flap is a new addition to the armamentarium of plastic surgeons for release of postburn flexion contracture of fingers.
Keywords
Finger flexion contracture
keystone flap
postburn contracture
1. Keystone flap is a new option for release of postburn flexion contracture of finger.
2. It reduces skin graft requirement, thus donor site morbidity is low.
3. Its utility is limited to mild contractures only.

INTRODUCTION
Postburn contracture is a major problem in developing countries.[1] Contractures are common sequela of hand burns because it is difficult for the patient to be compliant of physiotherapy and splinting regime. Flexion contracture of fingers is a cause of deformity in postburn patients.[2] Surgical release is the standard treatment for postburn flexion contractures of finger.[3] There are various methods described for coverage of resultant defect after finger contracture release.[12345] In case the defect is smaller it can be covered with local flaps, borrowing tissue from the adjacent (lateral) areas of finger. Most common flap described is the z-plasty transposition flap. Keystone design flap can be planned for these defects in such a way that it recruits tissue from lateral sides of finger to the defect in central part. We have used type-3 keystone design flap for coverage of defect after release of finger flexion contracture, with good post operative results.
CASE HISTORY
A 17-year-old, right-hand dominant, school-going girl, came to the plastic surgery department of our hospital with postburn flexion contracture of index, middle, and ring fingers at proximal interphalangeal (PIP) joint level. She had a history of accidental flame burn to the right hand 1 year back which healed with secondary intention without splinting. Now patient was admitted for surgical correction of deformity [Figure 1]. While planning the surgery, the expected defect was calculated by comparison from normal hand and it was found that there is tissue deficiency in index and middle fingers and the defect will require tissue from distant site for coverage. However, for ring finger contracture was found to be less severe and there was available tissue on lateral sides of finger to cover the defect. Table 1 presents the calculated defect size for each finger. Staged reconstruction was planned to correct the deformity. In the first stage, index and middle finger contracture was released and the resultant defect was covered with full thickness skin graft from groin area. Then after 1 week the ring finger contracture was released and a type-3 keystone design flap was planned to cover the defect [Figure 2]. The flap markings were planned preoperatively on normal finger beforehand [Figure 3].
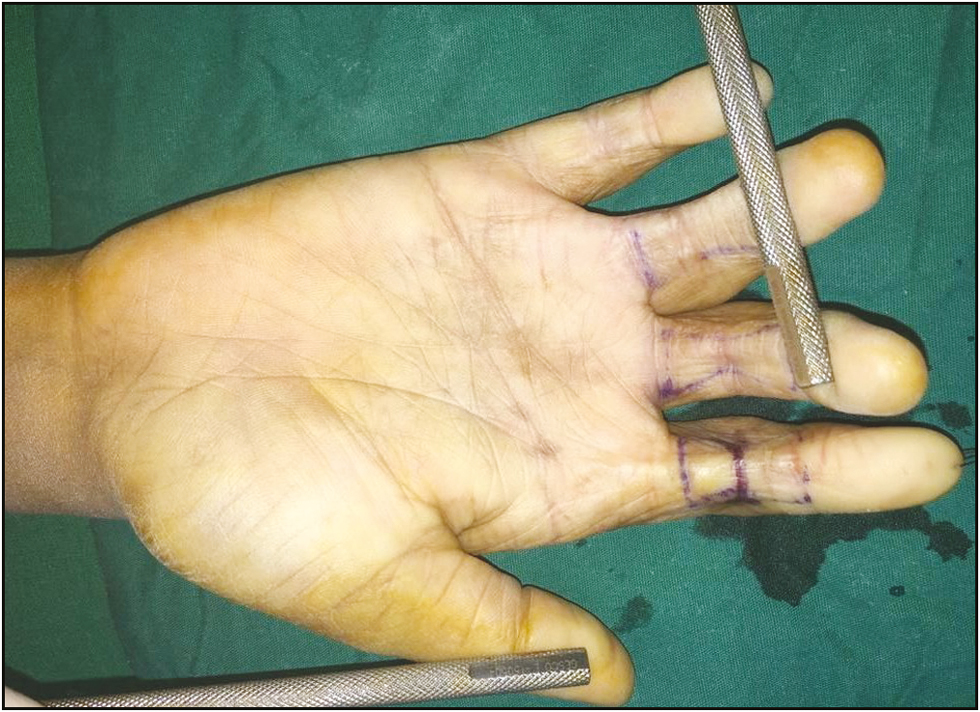
- Preoperative image of the postburn flexion contracture of right index, middle, and ring fingers
| True defect (area of the same zone of finger in normal hand) | Apparent defect (area of the scar tissue) | Expected defect size (difference between true and apparent defect) | |
|---|---|---|---|
| Index finger | 8 cm2 | 2.5 cm2 | 5.5 cm2 |
| Middle finger | 6.7 cm2 | 2.2 cm2 | 4.5 cm2 |
| Ring finger | 5.6 cm2 | 3.6 cm2 | 2 cm2 |

- Defect of width 1.5 cm after contracture release and internal splinting with Kirschner wire. Type-3 keystone flap is planned of width 0.7 cm on each side

- Preoperative planning on normal finger (opposite hand) for contracture release using type-3 keystone flap
Transverse release incision was given at the summit of the contracture. All the scar tissue was released until the finger became straight. The resultant defect was 1.5 cm wide extending up to midaxial line on both sides. For designing type-3 keystone flap the defect was imagined in two halves divided by a transverse line in the center. A curve parallel to the side of the ellipse was drawn proximal and distal to the defect taking width of the flaps same as that of the half defect (0.7 cm). Then tangents were drawn from both ends of the defect and perpendicular lines were made up to the point of intersection with the curve.[1] After marking the flap, skin and subcutaneous tissue were cut leaving the fascia over the pulley intact. Flaps were mobilized to cover the defect and two stay sutures were put. V-Y advancement was gained from both ends of the flaps. Both ends were closed in Y fashion. Two triangles of excessive tissue at the volar margin of the defect were cut and discarded from the flaps. Then the flap inset was given using HEMMing technique (horizontal everting mattress method of suturing).[1] There was a secondary defect at the proximal end of the finger, which was covered with a small full thickness skin graft from the groin area [Figure 4]. Full thickness skin graft of size 1.2 cm × 0.5 cm was required. Bolster dressing was given over the graft and light moist dressing was put on the flaps. External hand splint was applied keeping the PIP joint and metacarpophalangeal (MCP) joint straight. Hand elevation provided with the sling.
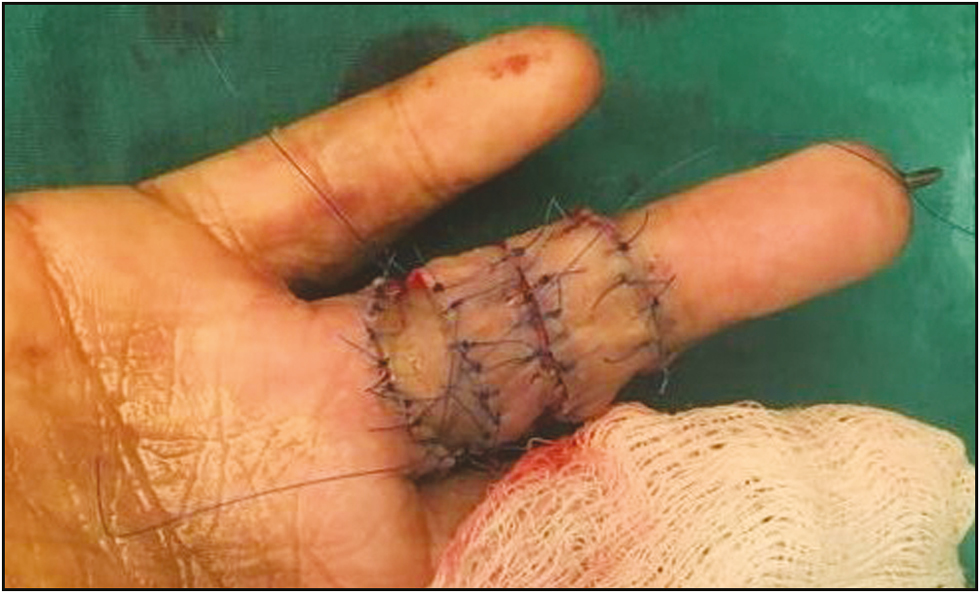
- Immediate postoperative image. Note that secondary defect after flap mobilization is covered with full thickness skin graft
Proximal flap had venous congestion during the first week, which got corrected by the second week. Graft was taken well. Sutures and K-wire were removed after 2 weeks. Hand therapy was started after K-wire removal. Pressure garments and silicone sheet were applied to facilitate better scar maturation. Figure 5 shows a postoperative picture after 4 weeks of surgery.

- Postoperative image after 4 weeks of surgery
DISCUSSION
The Keystone Design Perforator Island Flap (KDPIF) is a curvilinear shaped trapezoidal design flap. It is named after its similarity with the keystone used to support the arch in roman constructions. Behan[6] has described and classified this flap and also popularized its application in various locations of the body. There are four types of keystone flaps described:[6]
Type 1: Standard flap design, without cutting the deep fascia (suitable for defects up to 2 cm wide).
-
Type 2A: Standard flap design with deep fascia cut along the flap margins
a. Type 2A: Flap inset closes the defect primarily.
b. Type 2B: secondary defect created which is covered using split thickness skin graft.
Type 3: Double keystone flaps, designed on either side of the defect
Type 4: Rotational keystone flap.
Keystone flap is essentially two V-Y flaps end to side.[6] For designing a keystone flap, the excision should be parallel to the vessels or the line of perforators in that region.[7] Blood vessels of finger form a ladder pattern. Digital vessels run in longitudinal fashion along the length of the finger and give multiple transverse branches which are interconnected. Based on this there are two designs of keystone flaps possible in the finger [Figure 6]. Vascular supply of keystone flap in the finger comes through the subcutaneous tissue in the base of the flap similar to the volar V-Y advancement flap [Figure 7].
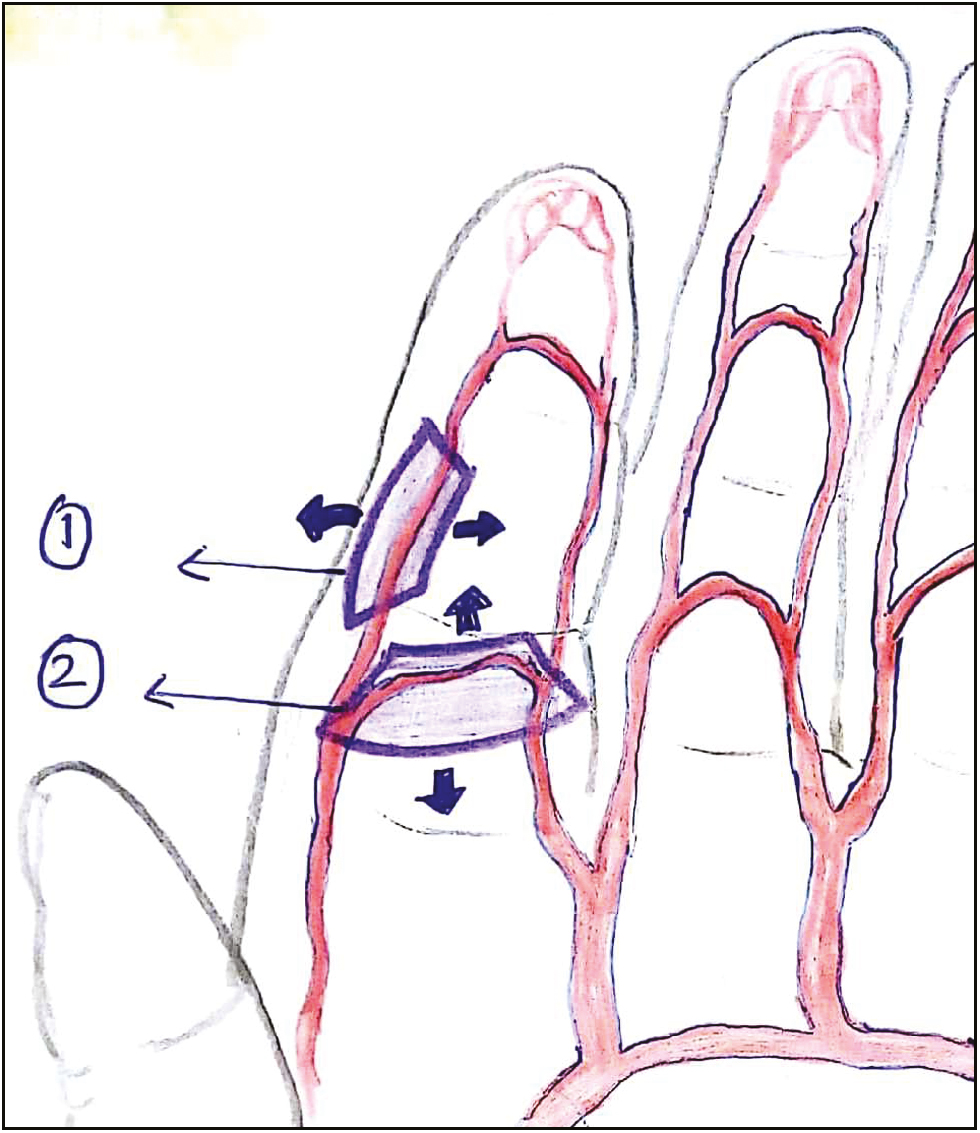
- Arterial pattern and possible designs of keystone flap in a finger. A keystone flap should be designed parallel to the vessels or the line of perforators in that region
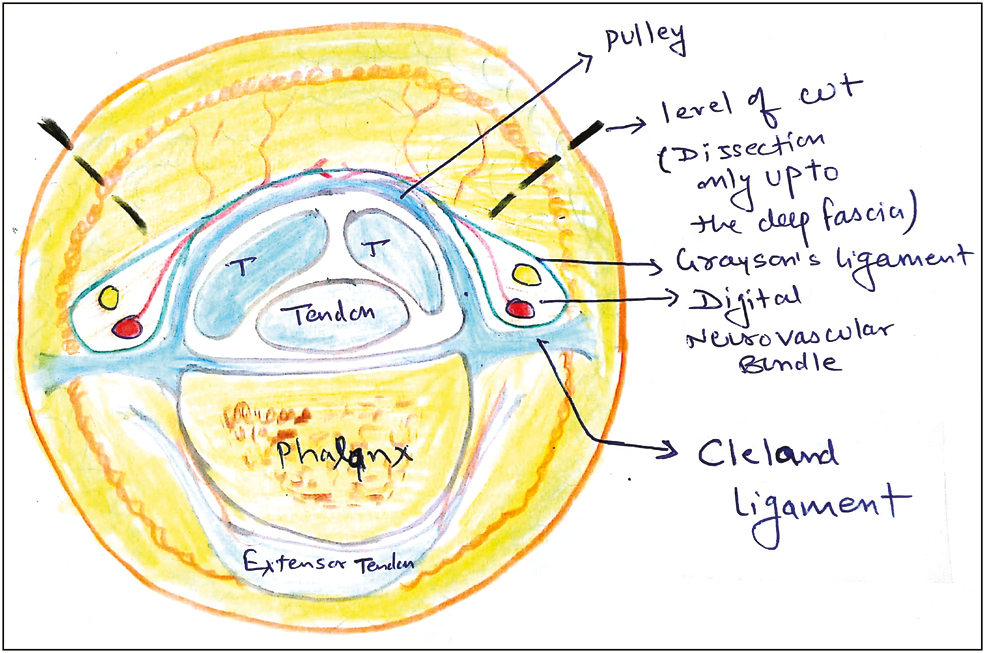
- Cross-section of finger at the level of shaft of proximal phalanx; the figure is showing depth of incision for raising keystone flap
There are various modifications of the keystone design flap described and it has been used in all regions of body from head to toe.[6789101112131415] We used type-3 keystone flap for reconstruction of defect after release of postburn flexion contracture of the fingers. It is the local tissue rearrangement which recruits tissue from lateral side of the finger similar to a z-plasty [Figure 8].
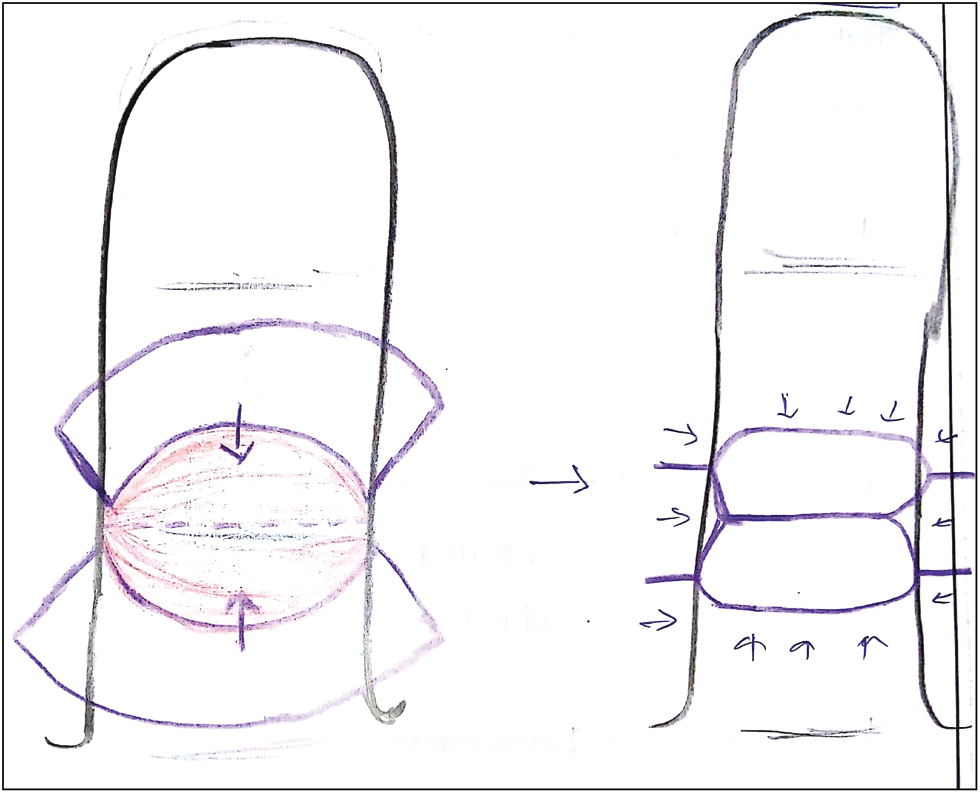
- Keystone flap is similar to two lateral V-Y flaps joined together. It recruits tissue from lateral sides and fills the defect in center
Advantage of doing a flap for finger flexion contracture release is that it utilizes the local tissue and thus it reduces requirement of the skin graft. Donor site morbidity is reduced. Also there is less scar contraction with flap compared to graft and thus chances of recurrence are less with flap. Compared to z-plasty the flap tip necrosis is expected to be less with the keystone flap because entire flap is attached to the base.
Limitation of using keystone flap for finger flexion contracture release is limited advancement. Designing a keystone flap requires availability of the tissue proximal and distal to the contracture site. Also, there should be skin laxity on lateral sides of the finger to provide V-Y advancement to flap from the sides. Thus, utility of this method of reconstruction is limited to mild contractures only. In our case, we were able to close 1.5 cm wide defect with this flap and 0.5 cm wide graft. Thus effective flap mobilization was 1 cm only.
Pin cushioning type edema and venous congestion are described as expected complications of keystone flaps.[6789] Proximal flap showed venous congestion in immediate postoperative period in our case. Keystone flap produces more scarring compared to skin graft or z-plasty. In case of finger reconstruction scar hypersensitivity may be a long-term complication of this procedure. Our patient is under follow up for long-term outcomes of the procedure. This is a single case report about use of type-3 keystone flap for finger contracture release. This case report shows that use of keystone flap is suitable for this indication. A large case series is required to study its anatomical and clinical effects.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Management of postburn contractures of the upper extremity. J Burn Care Res. 2007;28:212-9.
- [Google Scholar]
- Postburn flexion contractures of fingers: Anatomy and treatment with trapeze-flap plasty. In: Plastic and Reconstructive Surgery of Burns. Cham, Switzerland: Springer; 2018. p. :269-85.
- [Google Scholar]
- Bilateral side finger transposition flaps in the treatment of chronic postburn flexion contractures of the fingers. Ann Plast Surg. 2002;49:344-9.
- [Google Scholar]
- A systematic review on burn scar contracture treatment: Searching for evidence. J Burn Care Res. 2015;36:e153-61.
- [Google Scholar]
- The keystone design perforator island flap in reconstructive surgery. ANZ J Surg. 2003;73:112-20.
- [Google Scholar]
- Evolving concepts of keystone perforator island flaps (KPIF): Principles of perforator anatomy, design modifications, and extended clinical applications. Plast Reconstr Surg. 2016;137:1909-20.
- [Google Scholar]
- The keystone design perforator island flap. Part I: Anatomic study. J Plast Reconstr Aesthet Surg. 2007;60:883-7.
- [Google Scholar]
- The keystone design perforator island flap. Part II: Clinical applications. J Plast Reconstr Aesthet Surg. 2007;60:888-91.
- [Google Scholar]
- Extended experience and modifications in the design and concepts of the keystone design island flap. J Plast Reconstr Aesthet Surg. 2010;63:1359-63.
- [Google Scholar]
- The keystone island flap: Use in large defects of the trunk and extremities in soft-tissue reconstruction. Plast Reconstr Surg. 2011;127:1212-21.
- [Google Scholar]
- Keystone design perforator island flap for closure of myelomeningocele. Childs Nerv Syst. 2011;27:1459-63.
- [Google Scholar]
- Keystone island flap: An alternative reconstructive option to free flaps in irradiated tissue. ANZ J Surg. 2006;76:407-13.
- [Google Scholar]
- The cervico-submental keystone island flap for locoregional head and neck reconstruction. J Plast Reconstr Aesthet Surg. 2013;66:23-8.
- [Google Scholar]
- Keystone island flap reconstruction of parotid defects. Plast Reconstr Surg. 2012;130:36e-41e.
- [Google Scholar]





