Translate this page into:
Lasers for Lentigines, from Q-Switched to Erbium-Doped Yttrium Aluminium Garnet Micropeel, is There a Need to Reinvent the Wheel?
Address for correspondence: Dr. Kabir Sardana, Sector 28, House No. 466, Noida - 201 303, Uttar Pradesh, India. E-mail: kabir.sardana@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
The use of lasers in pigmentary disorders is largely based on the principles of selective photothermolysis (SPT)[1] that dictates that the pulse duration of the laser should be less than the size of the target cell. This is the basis of the use of Q-switched (QS) lasers for pigmented lesions. The use of the 532 nm wavelength for lentigines is ideal, as the lesion is found superficially wherein shorter-wavelength devices can be used successfully, despite their limited penetration depth of about 250 μm.[2] While this principle is good enough in Type I-III skin, in pigmented Skin Type IV-VI, laser interventions should factor in the consideration of postinflammatory hyperpigmentation (PIH). For this, an attempt has been made using the millisecond lasers that though are less selective also cause less PIH.[2] The logic is that long-pulsed lasers have a longer millisecond pulse width that results in more absorption by target melanin and less absorption by competing chromophores, such as oxyhemoglobin and surrounding pigmented skin, unlike the QS lasers. In addition, these lasers target melanin by photothermolysis only.[2] In contrast, QS lasers emit high-energy, nanosecond radiation, causing both photothermal and photomechanical effects. This paradoxically stimulates the surrounding melanin and oxyhemoglobin, thus leading to PIH.[2]
The need for using ablative tools for removing lentigines is an old concept and was abandoned as it was not based on the principles of SPT but on nonselective damage, as the target chromophore is water, abundant in the epidermis.[3] Moreover, as the thermal damage is more than the QS lasers, there are more chances of PIH.[2] The use of erbium-doped yttrium aluminium garnet (Er:YAG) in the so-called “micropeel mode” as a modality is based on the almost perfect and predictable depth dose dynamic of the Er:YAG laser.[2]
It is now well-understood that there are various Er:YAG treatment regimes, depending on the laser pulse width and the laser pulse energy, or more correctly, laser fluence (i.e., the laser energy per surface area in J/cm2).[345] The ablation threshold fluence is approximately 0.7 J/cm2 and can vary in real patient situations from 0.4 J/cm2 to 1.5 J/cm2 [Figure 1]. Professor Roland Kaufmann discovered that for each J/cm² an ablation of about 5 μm is achieved.[6] But this is only true above the ablation threshold of 1.5 J/cm² and was first studied with the prototype Er:YAG laser of Ascepelion, a laser that we have used extensively. To achieve an accurate depth, as a thumb rule, for every 1 J/cm2 after the ablation threshold, approximately 3-5 μm of tissue is ablated.[3] This can be used to set the fluence to effect accurate ablation. A second concept is that the more the energy that is transformed into heat, the less efficient the ablative effect and the greater the skin collagen coagulation. The Er:YAG single laser pulse durations may vary from 100 μsec to 1500 μsec.[345] The higher the pulse duration, the more the coagulation [Figure 2]. Thus, by adjusting laser pulse durations, the Er:YAG laser can be used to perform “Er:YAG” type, as well as erbium-doped yttrium scandium gallium garnet (Er:YSGG) and carbon dioxide (CO2) type laser treatments.
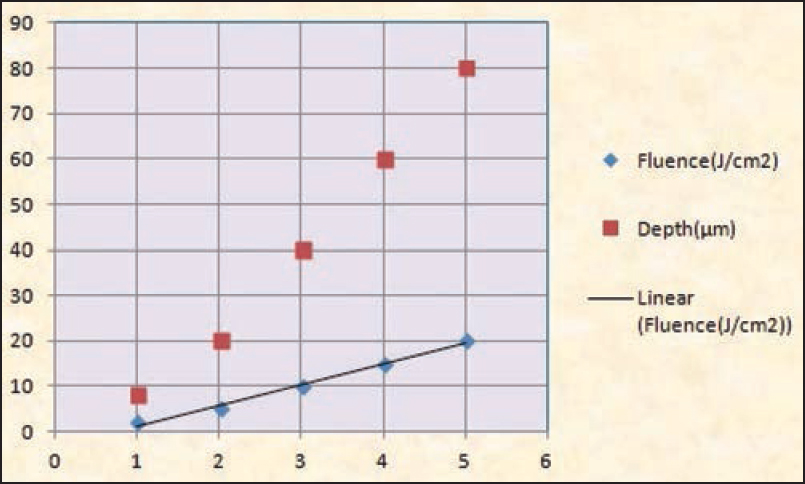
- A depiction of the predictable depth and dose equation of Er:YAG after the ablation threshold of about 0.4-1.5. X-axis fluence in J/cm2, Y-axis depth in μm
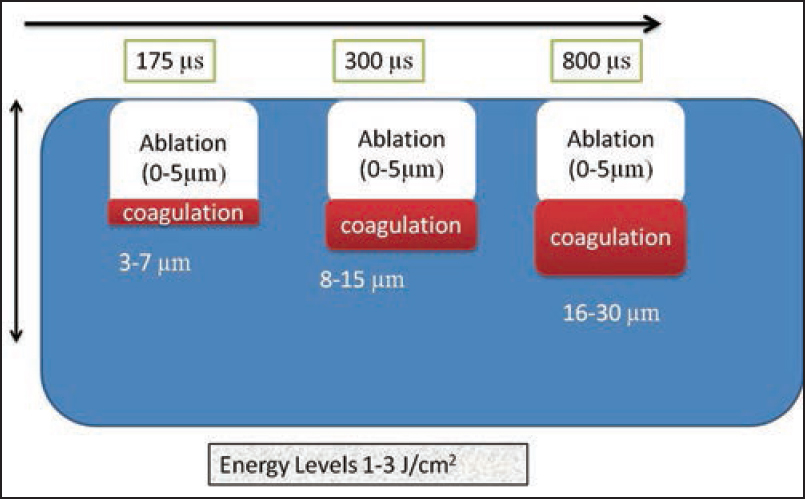
- A depiction of the effect of pulse duration on the ablation and thermal effect of Er:YAG laser in the so-called “Er:YAG peel setting.” Note that for the same fluence, an increase in the pulse duration leads to more thermal effect
In lentigines, what is needed is a “micropeel,” where the aim is minimum ablation. For this, the pulse duration and fluence has to be appropriately balanced. Many practitioners might assume that in order to work more safely, laser energy should be decreased. Paradoxically, this is not always the case. If the energy settings of the laser are reduced, more thermal effects in the tissue may be created. Additionally, the smaller the spot size, the less is the fluence that is required. Thus, the three parameters of importance are the fluence, pulse duration, and the spot size.
In a study, in this issue, the settings used were of 0.7 J/cm2, spot size 12 mm, 15 Hz. First, 0.7 J/cm2 is less than the ablation threshold of the skin. The large spot size would actually require a higher energy that is contrary to the lower fluence used. For pulse widths of or below approximately 100 μsec, the thermal effect again becomes limited to the Er:YAG laser absorption depth of 5 μ. This is the ideal pulse duration for a “micropeel,” but the authors have not mentioned the pulse duration. Notably, a high pulse duration will lead to unnecessary coagulation [Figure 2], not needed to treat lentigines. The advantage of the Er:YAG is that, for high repetition rates thermal necrosis does not exceed 50 μ, corresponding clinically to capillary bleeding after exposure of the dermis.[6] Thus, as there is less tissue necrosis, it is better than using the CO2 laser for such indications, a fact that we have seen in our practice. But the in vitro assessment of ablation depth requires advanced laser triangulation methods that allows a fast and accurate determination of ablated volumes and depths.[456] This as well, depends on the patient's skin type, treatment location, skin hydration level, and pulse duration. Thus, it is obvious that using the Er:YAG in the so-called “peel” mode is an art in itself and should not be universally used for all indications, specially pigmented lesions, where QS lasers have been found to be useful.
Importantly, even after using this mode, the results are not superior to conventional QS neodymium-doped yttrium aluminium garnet (Nd:YAG). In fact, two split-face studies have elegantly shown that the QS Nd:YAG was better than the Erbium peel and the combined approach caused more PIH.[7] Additionally, another study confirmed that the QS laser was superior to the fractional CO2 laser.[8] This just goes to prove that lasers that do not follow the principle of SPT[12] in reference to pigmented lesions rarely succeed in clinical practice.[2]
While there is no end to the types of combination modes, they should be based on a valid scientific logic. With epidermal pigmented lesions, the principles of SPT[1] fit in with the use of QS lasers and there is no reason to use ablative tools, as in pigmented skin, they can lead to PIH. Combination techniques can be used when one modality is not useful. In acne scars, ice-pick scars do not always respond to fractional lasers, hence, a punch excision followed by fractional treatment is a great idea. In case of a tattoo, specially professional types, a combination approach may be useful.[9] But for lentigines, there is little need for aggressive therapy, even if a good variable pulse Er:YAG laser is available. Moreover, where is the logic of using a pigment-specific laser, followed by the ablation of the epidermis with an Er:YAG laser? Here, the Er:YAG is merely serving as a tool to eliminate the pigment destroyed by the QS laser! Thus, it is better to “look through a window that others have opened than to create a new one where none is required.” It is our measured view, based on the existing literature that though the Er:YAG laser is a safe and well-researched tool,[345] its use in lentigines[67] is a case of “reinventing the wheel” and is probably not required in the treatment of lentigines.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220:524-7.
- [Google Scholar]
- Pigmented lesions and tattoos. In: Sardana K, Garg VK, eds. Lasers in Dermatological Practice (1st ed). New Delhi: Jaypee Brothers; 2014. p. :101-60.
- [Google Scholar]
- Carbon dioxide laser surgery. In: Goldman MP, Fitzpatrick RE, eds. Cutaneous Laser Surgery (2nd ed). USA: Elseiver; 1999. p. :302.
- [Google Scholar]
- Deep coagulation of dermal collagen with repetitive Er:YAG laser irradiation. Lasers Surg Med. 2000;26:215-22.
- [Google Scholar]
- A method for rapid measurement of laser ablation rate of hard dental tissue. Opt Laser Technol. 2009;41:397-402.
- [Google Scholar]
- Pulsed Erbium:YAG laser ablation in cutaneous surgery. Lasers Surg Med. 1996;19:324-30.
- [Google Scholar]
- A split-face, evaluator-blind randomized study on the early effects of Q-switched Nd:YAG laser plus Er:YAG micropeel (combined therapy) versus Q-switched Nd:YAG alone in light solar lentigines in Asians. Lasers Med Sci. 2014;29:1153-8.
- [Google Scholar]
- Laser treatment of solar lentigines on dorsum of hands: QS Ruby laser versus ablative CO2 fractional laser — A randomized controlled trial. Eur J Dermatol. 2011;25:122-6.
- [Google Scholar]
- A rapid tattoo removal technique using a combination of pulsed Er:YAG and Q-Switched Nd:YAG in a split lesion protocol. J Cosmet Laser Ther. 2015;17:177-83.
- [Google Scholar]





