Translate this page into:
Leiomyoma mimicking hypertrophic scar/keloid over the surgical incision site
*Corresponding author: Surajit Gorai, Department of Dermatology, Apollo Multispeciality Hospital, Kolkata, West Bengal, India. drsurajit@drgorai.com
-
Received: ,
Accepted: ,
How cite this article: Gorai S, Das K. Leiomyoma mimicking hypertrophic scar/keloid over the surgical incision site. J Cutan Aesthet Surg. doi: 10.25259/JCAS_65_2024
Abstract
Following surgery, hypertrophic scars/keloid is a frequent consequence, especially in people with a hereditary propensity for scar development. Although the precise cause of hypertrophic scar development is unknown, it is believed to be caused by an excess of collagen being produced at the site of damage. There are several ways to treat hypertrophic scars, including cryotherapy, laser therapy, intralesional steroids (ILS), and surgical excision. Recurrence rates are significant, and treatment results might be uncertain. In this case report, we describe a 43-year-old male patient who had spinal decompression and fixation surgery and thereafter acquired a hypertrophic scar/keloid-like lesion that was resistant to ILS. Following a biopsy, it was discovered that the tumor was a leiomyoma, which is quite rare in this situation.
Keywords
Leiomyoma
Hypertrophic scar
Keloid
Surgical incision
INTRODUCTION
Hypertrophic scar or keloid can happen over surgical or non-surgical trauma sites in predisposed individuals. Intralesional steroids (ILSs) are a standard therapy for that condition. We present a case of a patient with a hypertrophic scar over the back that developed after spine surgery, which, upon receiving ILS, progressed to form a keloid.
CASE REPORT
The patient, a 43-year-old male, presented with a firm, elongated, and mildly erythematous plaque at the site of a previous spinal decompression and fixation surgery 2 years back. The patient did not have any family history or similar lesions elsewhere in the body. The lesion had grown progressively over the past year and was causing itching, mild pain, and discomfort. The patient had previously undergone treatment with three sessions of ILSs in 1 month interval, but the lesion did not respond to this therapy. Thinking it as hypertrophic scar one more session of ILS given after 2 months when patient came to me. Despite treatment, the lesion continued to enlarge and developed into a keloidal lesions within 2 months [Figure 1]. Hence, it was decided to do a biopsy to confirm the diagnosis.
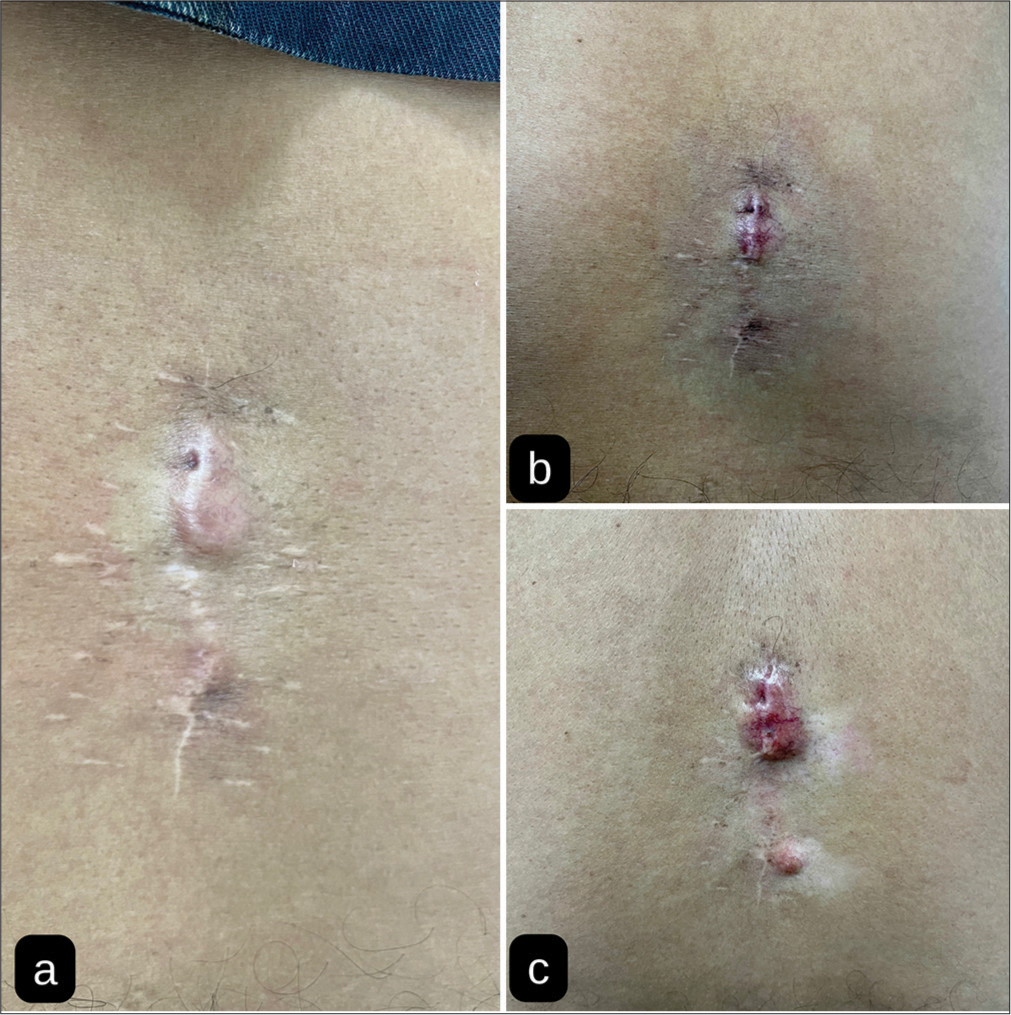
- (a) Lower back showing a midline linear keloid like mass, (b) lesion after first intralesional steroid (ILS) injection, and (c) lesion after second ILS injection.
An histopathology examination showed bundles of spindle-shaped cells with elongated, cigar-shaped nuclei, arranged in a whorled pattern. These cells had a smooth appearance and a moderate amount of eosinophilic cytoplasm. The finding was consistent with a leiomyoma. For confirmation, immunohistochemistry was done with desmin, smooth muscle actin (SMA), and Kiel-67 (Ki-67 Stain) and it was confirmatory [Figure 2]. Leiomyomas are benign tumors that arise from smooth muscle cells and are usually found in the uterus or gastrointestinal tract. Leiomyomas are rare in the skin and subcutaneous tissue, particularly following trauma or surgery.
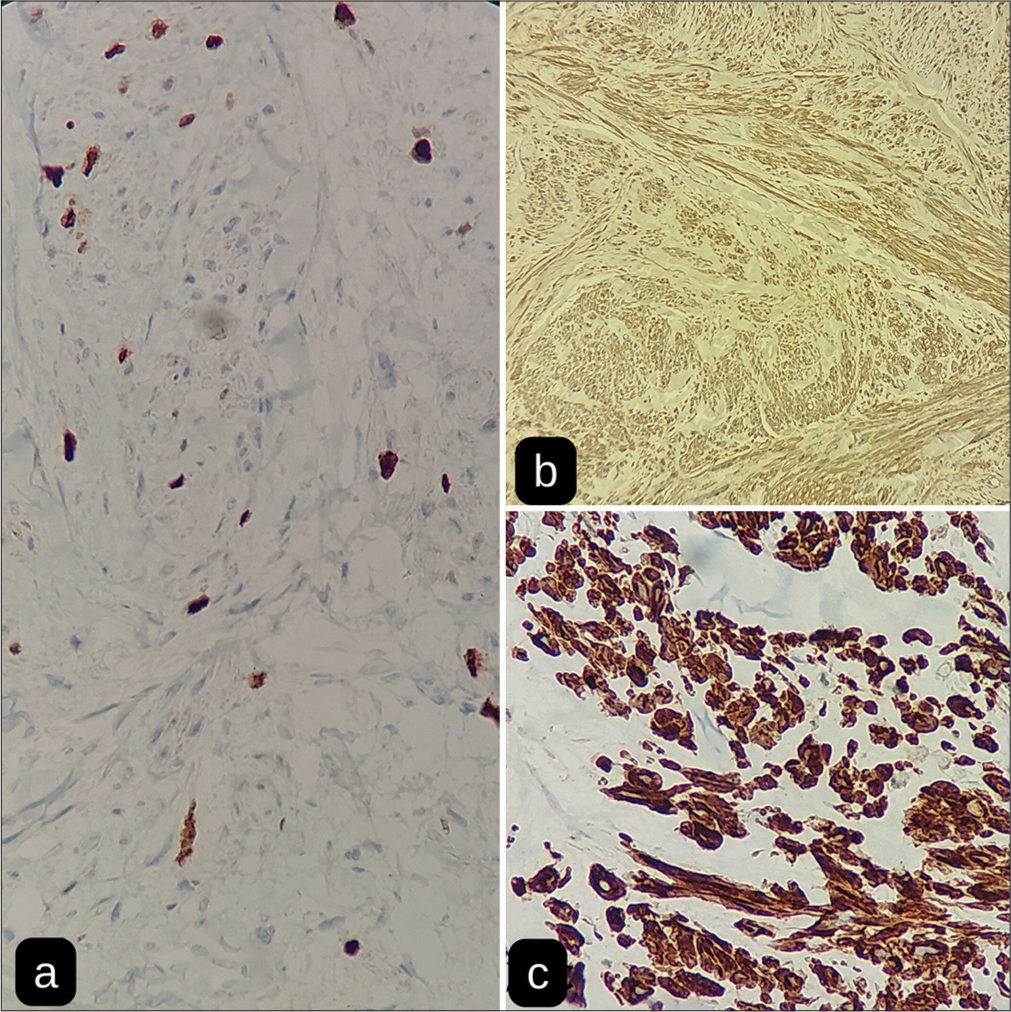
- (a) Kiel-67 (Ki-67 Stain) stain, (b) Smooth muscle actin (SMA) stain, and (c) Desmin stain.
Treatment
After the diagnosis of leiomyoma was confirmed, the patient underwent surgical excision of the lesion. The procedure was performed under local anesthesia, and the lesion was completely excised. The wound was closed with sutures.
Outcome
The patient experienced an uneventful post-operative recovery, with no complications or recurrence of the lesion. The histopathological analysis of the excised lesion confirmed the diagnosis of leiomyoma, and the patient was advised to follow-up with regular check-ups to monitor for any signs of recurrence.
DISCUSSION
Hypertrophic scars/keloid is a frequent post-operative consequence, and treatment results might vary. A biopsy may be required to rule out other underlying reasons when standard treatments, such as ILS, are ineffective in treating hypertrophic scars.1 Leiomyoma is a benign tumor that develops from smooth muscle cells. These tumors may develop in the skin, uterus, and other organs. Leiomyomas are normally slow-growing and asymptomatic, although depending on the organ or tissue they impact, their size and location may result in symptoms. Leiomyomas in the uterus, sometimes referred to as uterine fibroids, are the most prevalent benign tumors in women of reproductive age. They may result in various symptoms such as infertility, painful pelvis, and excessive menstrual flow. Leiomyomas in the skin appear as firm, well-defined nodules that are often asymptomatic. Leiomyoma is diagnosed based on clinical symptoms and imaging tests such as magnetic resonance imaging or ultrasound. Histopathological analysis and biopsy are gold standard investigations. Depending on the location, size, and severity of the tumor, there are many treatment options for leiomyomas. A surgical excision of the tumor or hormonal treatments may be advised in certain situations, while observation and monitoring may be suitable in others. Although leiomyomas are normally benign, there have been a few recorded occurrences of leiomyosarcoma, a malignant version of the condition. Within 15 years, up to 50% of cases may recur even after complete excision. In situations where surgical intervention is not feasible or is declined by the patient, alternatives such as nifedipine or nitroglycerin may be considered. Therefore, an accurate diagnosis and appropriate treatment rely heavily on detailed histological evaluation.2-4
CONCLUSION
Hypertrophic scars/keloid are consequences of surgery, trauma, infection, or sometimes spontaneous development in predisposed individuals. Histopathological examinations may be required to rule out other differential diagnosis when traditional therapy fails to improve hypertrophic scars. This instance emphasizes the need for awareness of leiomyomas, which are few and far between tumors that may develop in the skin and subcutaneous tissue after trauma or surgery. Additional study is required to better understand the pathophysiology of leiomyomas and to provide more potent therapy choices.
Authors’ contributions
Dr. Surajit Gorai: Conceptualization, clinical investigation, writing - Original draft. Dr. Kinnor Das: Literature review, writing - review & editing. Both authors reviewed and approved the final manuscript.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Keloids and hypertrophic scars: Review and treatment strategies. Semin Cutan Med Surg. 1999;18:159-71.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous leiomyomas In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: http://www.ncbi.nlm.nih.gov/books/NBK482166 [Last accessed on 2023 May 07]
- [Google Scholar]
- Cutaneous leiomyoma: Novel histologic findings for classification and diagnosis. Acta Med Iran. 2013;51:19-24.
- [Google Scholar]
- Review of leiomyoma variants. Am J Roentgenol. 2015;205:912-21.
- [CrossRef] [PubMed] [Google Scholar]







