Translate this page into:
Light-emitting Diode Light Therapy for Facial Seborrhoeic Dermatitis: A Case Report
Address for correspondence: Dr. Sanjeewani Fonseka, Department of Pharmacology, Faculty of Medicine, University of Peradeniya, Sri Lanka. E-mail: Sanjeewani.fonseka@yahoo.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Seborrhoeic dermatitis (SD) is a chronic, relapsing, papulosquamous inflammatory itchy dermatoses. It manifests as erythematous papules, macules, or ill-defined flat plaques with varying levels of scaling and pruritus. The exact pathogenesis of this condition is not known but Malassezia yeasts, hormones (androgens), amount of sebum produced, and deranged immune response are known to play important roles in its development. There is a wide range of therapeutic options to treat SD but some patients do not respond to any of the treatments. Here, we report three patients with treatment-resistant facial SD, successfully treated with light-emitting diode light therapy (LED-LT).
Keywords
Light-emitting diode light therapy
seborrhoeic dermatitis
treatment-resistant
LED-LT is a promising treatment option for patients with treatment-resistant SD

INTRODUCTION
SD is a chronic, recurring inflammatory skin disorder. The distribution of SD involves the scalp, hairline, eyebrows, glabella, nasolabial folds, ears, upper chest, back, axillae, and groins.
The treatment of SD is focused on reducing the inflammation with topical antifungal and anti-inflammatory agents, lithium gluconate/ succinate, coal tar, salicylic acid, selenium sulfide, sodium sulfacetamide, glycerin, benzoyl peroxide, aloe vera, mud treatment, and phototherapy. Rarely systemic therapies (antifungal, low-dose isotretinoin) are needed for resistant cases.[1] In certain situations, some patients do not respond to available treatments, treatment options are not available, or certain treatments cannot be employed because of limiting factors.
Case History
A patient with treatment-resistant SD was treated at an outpatient dermatology clinic (|**) and he was given LED-LT as a treatment option. He was an otherwise-healthy male (age 42 years) with type V skin according to Fitzpatrick skin classification, having SD involving the face, scalp, back, and chest. He had been previously treated with topical (antifungal, steroids, calcineurin inhibitors, coal tar, salicylic acid, selenium sulfide) and systemic (antifungal) therapies alone and in combination for more than one year without achieving complete remission. He was severely affected by pruritus and social embarrassment. He did not have photosensitivity disorders.
The patient was subjected to treatment with LED light (blue, yellow, and red combined) with a power of 60 mW/cm2 for 20 min in continuous mode. He was reviewed at every three weekly intervals. The patient showed clinical improvement in relation to pruritus, scaling, pigmentation, texture of the skin, and sebum secretion. Also, he showed a 50% improvement after the first treatment [Figures 1–3] and he had three sessions of LED-LT. At the end of the third session, the patient was almost completely better and he was maintained on topical emollients and sunscreens. He did not have any adverse effects and was satisfied with the results.

- Improvement of patients with treatment-resistant SD with LED-LT. (A) Before LED-LT. (B) After the LED-LT (front view of the face)
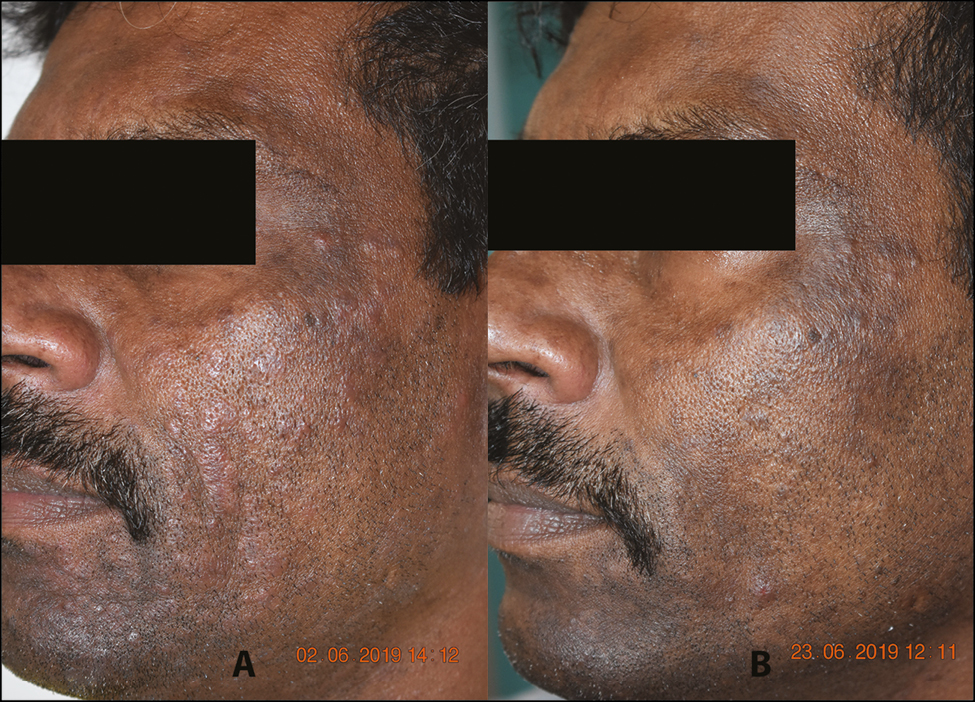
- Improvement of patients with treatment-resistant SD with LED-LT. (A) Before LED-LT. (B) After the LED-LT (left view of the face)

- Improvement of patients with treatment-resistant SD with LED-LT. (A) Before LED-LT. (B) After the LED-LT (right view of the face)
DISCUSSION
LED is a noninvasive, nonthermal, nonablative light treatment that uses noncoherent, noncollimated light in the ultraviolet (UV), visible, and near-infrared ranges of the electromagnetic spectrum (≈255–1300 nm).[2] Changes of the skin due to LED treatment have been shown to be due to alteration of skin cellular proliferation, differentiation, migration, inflammation, and collagen production (photobiomodulation).[3] LED is being increasingly used in a wide range of dermatological conditions, including acne vulgaris, herpes simplex/zoster, acute wound healing, eczema, and facial rejuvenation. Evidence for use of LED for SD is scarce.
LED-LT consists of a variety of lights with different wavelengths that determine the depth of penetration.[4] We used three colors, that is, blue, yellow, and red.
The blue color (400–490 nm) penetrates only to the epidermis (<1 mm) and is beneficial for skin conditions in the epidermal layer. Yellow light (570–590 nm) penetrates up to the papillary dermis (0.2 to 2 mm) and is beneficial in photoaging and skin conditions with erythema, swelling, and other effects related to pigmentation. The red color (630–700 nm) penetrates deeper than the reticular dermis (2–3 mm) and is beneficial for skin rejuvenation, wound healing, and post-laser recovery.[45] LED with blue and red light has antibacterial activity and anti-inflammatory effects with inhibitory action on Propionibacterium acnes.[67]
UV light induces cell apoptosis through DNA damage, cellular damage, and induction of reactive oxygen species accumulation in Candida albicans.[8] A study has shown the antifungal effects of electromagnetic radiation with 380 ± 2 and 392.5 ± 1 nm wavelengths.[9] The authors of that study suggest that LED can be used as an adjunctive therapeutic light tool against Malassezia yeast-related cutaneous diseases such as SD. The wavelength of 392.5 nm was the border between the visible light spectrum (400–700 nm) and UV spectrum (320–400 nm). However, evidence for clinical application of LED to treat SD of the face is limited.
The pathogenesis of SD is not completely understood. Some postulate that the condition is associated with colonization of the skin of affected individuals with species of the genus Malassezia. The disease tends to be localized to sebum-rich areas, leading to the hypothesis that fungal metabolites react with triglycerides released from sebaceous glands producing inflammatory mediators. Another theory is that the fungi make the keratinocyte release inflammatory cytokines.[10] Therefore, the treatment of SD should be directed toward reducing the inflammation.
Although the effectiveness of LED in SD has not been studied, there is evidence for its effectiveness in acne. As both SD and acne are related to sebum production and secretion, it could be argued that LED has a role in the treatment of SD.[11]
A study investigating the effect of 415 nm blue light and 630 nm red light on lipid production showed that 415 nm blue light significantly suppressed sebocyte proliferation whereas 630 nm light only slightly inhibited it. The levels of peroxisome proliferator-activated receptor gamma (PPAR-γ), a potential modulator of lipid production in human sebocytes, were also significantly reduced by red-light exposure.[12] Another study on the clinical and histological effects of the combination of blue-red LED phototherapy for mild-to-moderate acne vulgaris demonstrated a decrease in sterol regulatory element-binding protein 1 (SREBP-1), (master regulator of lipid synthesis in sebaceous glands), the mean sebaceous gland size, and lipid production.[13] Another review also highlighted the fact that LED light leads to a reduction of pore size and size of the sebaceous gland and improvement in acne.[11]
These findings may explain the improvement in our patient, as pathogenesis of SD involves sebocytes and sebum production.
The inflammation, pigmentation, and pruritus in our patient improved with LED therapy with a combination of three colors. Therefore, single colors and a combination of two colors can be studied. To get the maximum effects from LED therapy, several factors, including power, wavelength, mode (pulsing or continuous), the interval between treatments, and the total number of treatments, should be known for a particular indication. The molecular basis of improvement has to be studied, and correct parameters of light therapy for SD have to be determined in future studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/ have given his/ her/ their consent for his/ her/ their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Treatment of seborrheic dermatitis: A comprehensive review. J Dermatolog Treat. 2019;30:158-69.
- [Google Scholar]
- High fluence light emitting diode-generated red light modulates characteristics associated with skin fibrosis. J Biophotonics. 2016;9:1167-79.
- [Google Scholar]
- Light-emitting diodes: A brief review and clinical experience. J Clin Aesthet Dermatol. 2015;8:36-44.
- [Google Scholar]
- Photodynamic and photobiological effects of light-emitting diode (LED) therapy in dermatological disease: An update. Lasers Med Sci. 2018;33:1431-9.
- [Google Scholar]
- Eradication of propionibacterium acnes by its endogenic porphyrins after illumination with high intensity blue light. FEMS Immunol Med Microbiol. 2003;35:17-24.
- [Google Scholar]
- Phototherapy with blue (415 nm) and red (660 nm) light in the treatment of acne vulgaris. Br J Dermatol. 2000;142:973-8.
- [Google Scholar]
- Studies on the relationship between pulsed UV light irradiation and the simultaneous occurrence of molecular and cellular damage in clinically-relevant candida albicans. J Microbiol Methods. 2011;84:317-26.
- [Google Scholar]
- The antifungal effect of light emitting diode on malassezia yeasts. J Dermatol Sci. 2012;67:3-8.
- [Google Scholar]
- The effects of narrowbands of visible light upon some skin disorders: A review. Int J Cosmet Sci. 2016;38:325-45.
- [Google Scholar]
- Propionibacterium acnes activates the IGF-1/IGF-1R system in the epidermis and induces keratinocyte proliferation. J Invest Dermatol. 2011;131:59-66.
- [Google Scholar]
- The clinical and histological effect of home-use, combination blue-red LED phototherapy for mild-to-moderate acne vulgaris in korean patients: A double-blind, randomized controlled trial. Br J Dermatol. 2013;168:1088-94.
- [Google Scholar]





