Translate this page into:
Mastering Surgical Skills Through Simulation-Based Learning: Practice Makes One Perfect
Address for correspondence: Dr. Niti Khunger, Department of Dermatology and STD, Safdarjung Hospital and Vardhman Mahavir Medical College, New Delhi - 110 029, India. E-mail: drniti@rediffmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Simulation-based learning in surgery is a learning model where an environment similar to real life surgical situation is created for the trainee to learn various surgical skills. It can be used to train a new operator as well to assess his skills. This methodology helps in repetitive practice of surgical skills on nonliving things so that the operator can be near-perfect when operating on a live patient. Various models are available for learning different dermatosurgery skills.
Keywords
Simulation-based learning
surgical skills
dermatosurgery
teaching models
INTRODUCTION
Methods of teaching and mastering surgical skills are changing in today's competitive environment. Previously, there was hardly any formal training in basic surgical skills and most medical students and residents had their first lessons by observing and then practicing their skills on the patients, using the formula, see one, do one, teach one.[1] But this is no longer easy, as clinical pressures nowadays require the highest degree of efficiency and leave no room for shoddy work or errors in the operation theatre. Besides, lack of valuable operating time leaves very little time for the surgeon to teach students inside the operating environment. In addition, surgical skills cannot be mastered by simple observation. Additionally, cadaver training is not easily available. To overcome these difficulties, simulation-based learning becomes a viable method. Besides, it additionally provides an opportunity to teach and then assess medical students objectively and in addition, gives the students a chance to practice extensively and gain confidence before they enter the operating room and operate on live patients. In addition, it is a useful method for older practitioners wanting to upgrade their surgical skills.
TEACHING TOOLS FOR SURGICAL SKILLS
Various teaching tools can be used for surgical training. Suturing techniques are the basic surgical skills required by all residents practicing surgery. The rapid expansion and demand for dermatosurgery has compelled postgraduate students to learn surgical skills as well as older dermatologists to upgrade themselves. Mastering suturing skills is the cornerstone of surgical procedures. The traditional teaching methods include didactic lectures, clinical discussions, and audiovisual presentations. However, these are one-way programs and are not very useful for the development of technical surgical skills. The “mentored” approach of learning surgical skills is another conventional method, where the postgraduate student observes the procedure being done by the mentor, gradually learns the procedure, then performs under supervision, and soon performs it independently. The main drawback with this approach is that it may not always be possible for the mentor to teach when the patient load is high or when there are too many students observing the procedure. In addition, learning surgical skills on a live person can have medical, legal, and ethical issues. The use of simulation has shifted the learning of basic surgical skills from the operation theatre to the laboratory to practice and hone surgical skills.
WHAT IS SIMULATION-BASED LEARNING?
Simulation is an instructional strategy used to teach technical skills, procedures, and operations, by presenting learners with situations that resemble reality.[2] Surgical simulation involves the use of objects, devices, electronic and/or mechanical surgical simulators, cadavers, animals, and animal organs to reproduce or represent, under test conditions, situations that are likely to occur in actual performance. Simulation-based learning has many advantages such as:
-
It allows the person to acquire the skills before operating on a live person
-
The surgeon later is more competent to handle intraoperative complications
-
The surgeon can practice less commonly performed surgeries beforehand
-
A trainee can be tested and objectively by seniors on their efficiency
-
It helps to increase speed, efficiency, automaticity, and precision
HOW TO INTRODUCE SIMULATION
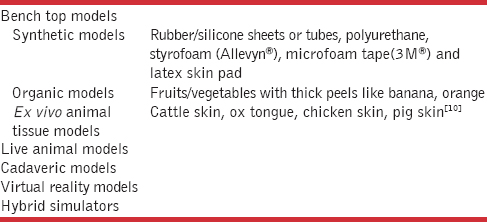
There are various types of simulation techniques[34] [Table 1]. Newer methodologies to teach surgical skills and assess students objectively have been developing as well. These include virtual reality, robotics, telemedicine, computer games,[5] artificial skin, and wound closure pads [Figure 1]. Their success depends on how close they are to reality in terms of the texture and handling. There are various shapes and sizes that are available.
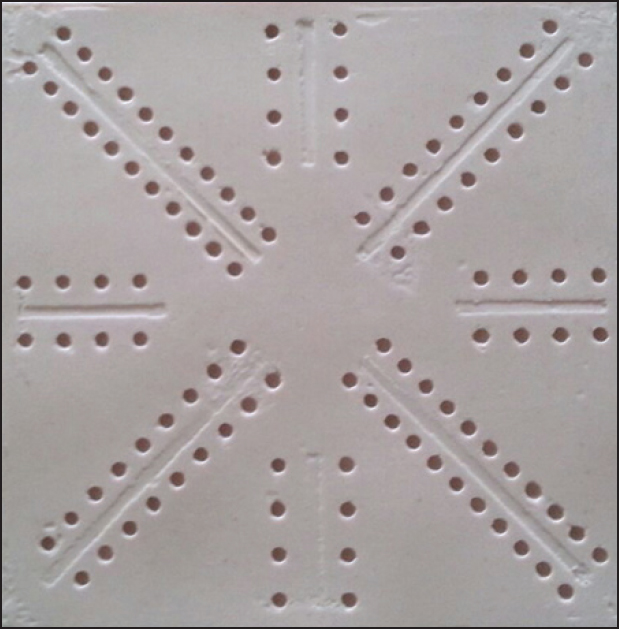
- Artificial rubber pad for learning suturing techniques
Benchtop models include synthetic or nonlive animal tissue models such as organic fruits or vegetables, chicken thighs or wings, and others. To assess learning of surgical skills on benchtop models, objective assessment of technical skills (OSATS) was developed by Reznick et al. at the University of Toronto[6] and is now widely used by different surgical specialties. Simulation models can be high fidelity (as real as living human tissue) such as live animals and fresh human cadavers or low fidelity (less real as compared to living human tissues) such as synthetic bench models.[7] Even though high fidelity models are as close to reality as possible, but they have disadvantages of limited availability, low cost, risk of infections, and ethical issues. By contrast, low fidelity models are easily available and can be repeatedly used. Studies have shown that simulation-based learning is definitely better than didactic lectures.[6789] Even though students feel that surgical skill acquisition may be better with high fidelity models, there is not much difference between the two.[78] Fruits and/or vegetables with thick peels, being simple, versatile, portable, reproducible, affordable, easy to purchase, and of low cost, are a good alternative as well and they provide a three-dimensional (3D) platform to work on.[10] These flat bench models can be used for learning incisions, biopsy, and suturing. For excision of lipomas or cysts, Denadai et al. have used styrofoam balls or mini balloons filled with ink placed within chicken thighs or wings making the learning experience as real as possible.[4] Cadaver training and the use of pigskin may be done, but it is not always practical. A study showed that there was significant improvement in competence of prefinal year medical students in performing basic surgical skills after they were taught those skills through simulation-based learning on fresh human skin model.[11] Virtual reality is an advanced human-computer interface such as a 3D computer-generated world that mimics the real world and allows participants to interact with and navigate it, using components of their five senses in real time.[3] It has been used in studying cellular compartments of neural tissues and in other fields.[12] Virtual reality models help in generating skill-based surgical behavior that is highly integrated and automated.[13] These models have been used for laparoscopic surgeries.[14]
HOW TO TEACH
The various stages of simulation-based learning include:
-
Verbal learning directed by the instructor, based on learning materials, diagrams, books, online tools, and videos narrated by experts;
-
Instructor-led training on bench models;
-
Self-directed training outside the classroom, for example, at home;
-
Training focused on procedures performed out-of-class by an instructor — After the out-of-class practice.[14]
In the first step of teaching, the students can be taught by an expert or even a multimedia software computer-assisted-learning, (CAL). The gold standard currently used for evaluating a person learning surgical skills through simulation is OSATS. OSATS consists of two subscales: Task-specific checklist and Global Rating Scale (GRS).[3] Dendai et al. have proposed a curriculum on learning skills involving the skin, in which they propose the approximate training time for learning surgical knots is 2 weeks, incision and suture techniques is 2 weeks, biopsy techniques is 3 weeks, skin grafts is 3 weeks, surgical flaps is 5 weeks, and management of cutaneous lesions is 4 weeks.[4] The same authors have additionally adapted the GRS for cutaneous procedures for assessment of the trainees’ performance that includes respect for tissue, time in motion, instrument handling, elliptical excision skill, suture training, flow of operation, knowledge of procedure, final product, and overall performance.[4]
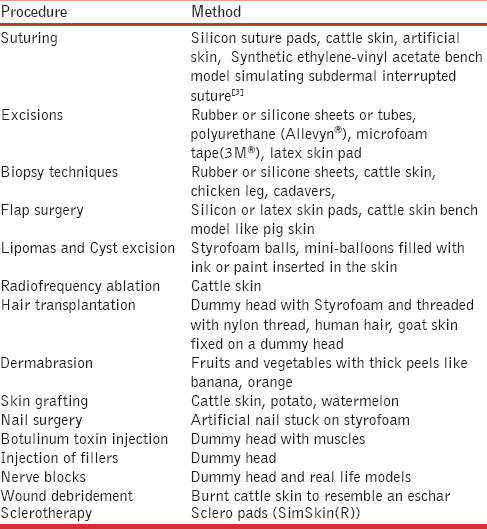
SURGICAL SIMULATION IN DIFFERENT DERMATOLOGICAL PROCEDURES
Various dermatological procedures can be taught by inanimate models [Table 2]. Excision of cysts and subcutaneous tumors are taught in various institutions. Here, subcutaneous tumors or cysts are simulated using cut finger of glove filled with toothpaste or balloons filled with ink or small lemons. These are inserted into chicken thigh or pig muscle and used as bench models. A computational formulation of the finite element method has been used for various flap designs of Z-plasty, rotation, rhomboid flaps, S-plasty, and related techniques in three-dimensional operation on skin sheets and scalp flaps.[16] A game called Z-DOC which has touch-based interactions has been developed for training plastic surgery residents the steps of Z-plasty procedure.[17]
Similarly simulation surgery can be used for learning hair transplantation where artificial hair may be transplanted onto pig skin. Other hair traansplant simulations include fixing goat skin on a dummy head or fixing black kite thread or discarded human hair on a styroform base fixed to a dummy head [Figures 2a–d and 3] In vitiligo surgery, pig skin or cow skin may be used as both donor and recipient site for learning mini punch grafting and split skin thickness grafting.

- Dummy head covered with styrofoam and implanted with cut human hair (Photo courtesy:Dr Aman Dua & Dr Kapil Dua)

- Dummy head covered with styrofoam and implanted with cut kite thread (Photo courtesy:Dr Aman Dua & Dr Kapil Dua)

- Dummy head covered with goat skin (Photo courtesy:Dr Aman Dua & Dr Kapil Dua)

- Close-up of goat skin showing few extracted hair follicule units (Photo courtesy:Dr Aman Dua & Dr Kapil Dua)

- Implantation of hair follicles on a styrofoam covered dummy head (Photo courtesy:Dr Aman Dua & Dr Kapil Dua)
Sclerotherapy pads containing several vessels of various diameters ranging from 0.2-3 mm are also available for training for sclerotherapy (SimSkin Sclero pad, Chicago, USA, www.Simskin.com) [Figure 4].

- Sclero pad with vessels which blanch on injection for teaching sclerotherapy (Simskin(R) USA)
THE FUTURE OF LEARNING SURGICAL SKILLS
The future of simulation-based learning in dermatological haptic virtual reality surgeries are virtual reality models. These will create a situation similar to that in the operation theatre. Haptic systems or haptics are a part of advanced virtual reality systems that interacts with the user's sense of touch. 3D printing has been used in urology where organs (the kidney, renal pelvis, and ureter) were created with a 3D modeling software, printed with a Spectrum Z510 3D printer (Z Corporation, 3D Systems, USA), and cast with Dragon Skin 30 silicone rubber (Smooth-On, Inc. Macungie PA 18062, USA). The model was secured in a laparoscopy box trainer for use.[15] Similar models can be developed for dermatological procedures.
CONCLUSION
Simulation-based training is becoming an increasingly popular tool to teach suturing skills. It helps medical students, surgical residents in various specialties including dermatology, and additionally older practitioners to learn and master surgical techniques. Simulation enables the trainee to avoid the early error-prone and difficult part of the surgical training curve and in addition, to gain confidence before entering the surgical operating environment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The role of simulation in surgical training. Annals of The Royal College of Surgeons of England. . 2000;82:88-94.
- [Google Scholar]
- Surgical simulation and virtual reality: The coming revolution. Ann Surg. 1998;228:635-7.
- [Google Scholar]
- Basic plastic surgery skills training program on inanimate bench models during medical graduation. Plast Surg Int 2012 2012 651863
- [Google Scholar]
- Evolving educational techniques in surgical training. Surg Clin North Am. 2016;96:71-88.
- [Google Scholar]
- Teaching elliptical excision skills to novice medical students: A randomized controlled study comparing low- and high-fidelity bench models. Indian J Dermatol. 2014;59:169-75.
- [Google Scholar]
- Does bench model fidelity interfere in the acquisition of suture skills by novice medical students? Rev Assoc Med Bras. 2012;58:600-6.
- [Google Scholar]
- Bench model surgical skill training improves novice ability to multitask: A randomized controlled study. Stud Health Technol Inform. 2011;163:192-8.
- [Google Scholar]
- Organic bench model to complement the teaching and learning on basic surgical skills. Acta Cir Bras. 2012;27:88-94.
- [Google Scholar]
- Evaluation of medical students› attitudes and performance of basic surgery skills in training program using fresh human skin, excised during body contouring surgeries. J Surg Educ. 2015;72:868-74.
- [Google Scholar]
- Three-dimensional immersive virtual reality for studying cellular compartments in 3D models from EM preparations of neural tissues. J Comp Neurol. 2016;524:Spc1.
- [Google Scholar]
- Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: A randomized educational trial. BMC Med Educ. 2012;12:7.
- [Google Scholar]
- Low-fidelity bench models for basic surgical skills training during undergraduate medical education. Rev Col Bras Cir. 2014;41:137-45.
- [Google Scholar]
- Use of 3-dimensional printing technology and silicone modeling in surgical simulation: Development and face validation in pediatric laparoscopic pyeloplasty. J Surg Educ. 2014;71:762-7.
- [Google Scholar]
- A Real-Time Local Flaps Surgical Simulator Based on Advances in Computational Algorithms for Finite Element Models. Plast Reconstr Surg. 2016;137:445e-52e.
- [Google Scholar]
- Z-DOC: a serious game for Z-plasty procedure training. Stud Health Technol Inform. 2013;184:404-6.
- [Google Scholar]






