Translate this page into:
Maximizing keloid treatment efficacy: Enhanced results through the synergy of erbium glass laser and intralesional steroids
*Corresponding author: Yogesh M. Bhingradia, Shivani Skin Care and Cosmetic Clinic, Surat, Gujarat, India. yogeshbhingradia@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhingradia YM, Preethi P, Sadhwani M, Pravin A. Maximizing keloid treatment efficacy: Enhanced results through the synergy of erbium glass laser and Intralesional steroids. J Cutan Aesthet Surg. doi: 10.25259/JCAS_69_2024
Abstract
Objectives
Keloids are benign hyperplasias precipitated by tissue injury, usually refractory to several treatment modalities. Therefore, there is always a search for novel combination therapeutic options. In this study, we sought to analyze keloid treatment efficacy by combining intralesional steroid (ILS) and erbium glass laser. The study aims to compare the efficacy and outcome of erbium glass laser plus ILS for the treatment of keloids. This is a retrospective, single-center, uncontrolled, open-label study.
Material and Methods
A total of 44 patients with keloids at various sites were included in the study according to the inclusion criteria. Each lesion was treated with a single pass of Erbium glass laser (1540 nm), without overlap, followed by 40 mg/mL of ILS in the same sitting. Six sessions were carried out at monthly intervals. The modified Vancouver scar scale (VSS) was used for the assessment of keloidal scar reduction. Scars were reassessed after 6 months of the last session. The Statistical Package for the Social Sciences software Windows version 23.0 was used to analyze the data. Fisher’s exact test was used and P ≤ 0.05 was considered significant.
Results
30 patients came for regular follow-up. During the follow-up after cessation of treatment, only two patients showed recurrence. There was a statistically significant mean difference between the modified VSS score at baseline and that after 6 months of therapy.
Conclusion
Combining erbium glass laser with ILS can have promising results for the treatment of keloids with fewer treatment sessions, alleviating pain and pruritus, lesser recurrence rate, and thereby resulting in higher patient satisfaction.
Keywords
Erbium glass laser
Intralesional steroid
Keloid
INTRODUCTION
The term keloid was originally described in the 1800s as “cheloid,” derived from the Greek word “chele” which means “crab claw.” Trauma that creates tissue loss gives rise to the repair process and eventually ends with scar tissue.1 ILS is the gold standard and well-established therapeutic modality for keloids.2 However, administering ILS into keloidal tissue poses difficulty due to its hard and thick nature, thereby leading to spillage and uneven diffusion of steroids in the tissue. Furthermore, in terms of outcome, combination therapies have proven to be superior to monotherapy with ILS.3 As Erbium glass laser is a non-ablative fractional laser and well tolerated by the Indian skin,4 this article explores the potential synergistic effects of combining erbium glass laser therapy with intralesional steroid injections to maximize the efficacy of keloid treatment.
MATERIAL AND METHODS
A total of 44 patients belonging to type IV and V skin types on the Fitzpatrick scale were taken in this study between June 2022 and June 2024. All patient demographics were taken from clinic medical records and analyzed. The diagnosis of keloid was made on a clinical basis. All patients above 12 years of age who had not taken any treatment for keloids were included in the study. Exclusion criteria were age under 12 years, patients’ refusal to allow steroid therapy, pregnant females, infected keloids, and patients with underlying diseases such as diabetes mellitus were also excluded, as wound healing would be hindered in them.
All the available clinical history was noted. All patients were treated with a single pass of erbium glass laser (QQ laser, German 1540 nm fiber laser) with parameters of 100 dots per area, fluence: 45 J/cm2 without overlap, followed by injection of 1:1 mixture of triamcinolone acetonide (40 mg/mL) and lidocaine hydrochloride 2% (400 mg/20 mL) into the lesion intradermally (0.1 mL/1 cm2). Air cooling was done during the procedure. Silicone gel was not used in between two treatment sessions. Patients were followed up every 4 weeks for subsequent sessions. A total of six sessions were carried out without any local or topical anesthesia.
In each visit, the steroid injection dose was adjusted according to requirements based on the reduction of size and thickness. Treatment outcomes were assessed based on keloid size reduction, symptomatic improvement, and recurrence rates. The modified vancouver scar scale (VSS) was used to assess objective improvement in the keloidal scars. Any adverse effects were also documented. Photographs were obtained during each visit to evaluate the results. Patients were followed up to 6 months after the last session to assess the reduction in size of keloids as well as any recurrence, if any. Written informed consent was obtained from all patients. Results were analyzed with the Statistical Package for the Social Sciences software Windows version 23.0 and Fisher’s exact test was applied. P ≤ 0.05 was considered significant.
RESULTS
Out of 44 patients in the study, 27 (61.4%) were males and 17 (38.6%) were females. The mean age of patients was 34.55 ± 11.58 years. The predominant site of keloid was chest (25%) in our study, and only 8 (18.2%) study participants had pain and pruritus each [Table 1 ]. Post-procedure burning sensation was seen in 4 (9.1%) 4 (9.1%) patients experienced patients and post-treatment pain. Thirty patients came for follow-up regularly and completed the protocol [Figure 1a and b]. Only two patients showed recurrence during the follow-up and five patients were lost to follow-up. The outcome of study participants is summarized in Table 2.
| Variables | n | % | Total (%) |
|---|---|---|---|
| Site | |||
| Earlobe | 6 | 13.6 | 44 (100) |
| Arm | 1 | 2.3 | |
| Axilla | 1 | 2.3 | |
| Back | 4 | 9.1 | |
| Breast | 3 | 6.8 | |
| Buttock | 2 | 4.5 | |
| Chest | 11 | 25.0 | |
| Face | 6 | 13.6 | |
| Forearm | 1 | 2.3 | |
| Hand | 4 | 9.1 | |
| Knee | 1 | 2.3 | |
| Legs | 2 | 4.5 | |
| Shoulder | 1 | 2.3 | |
| Waist | 1 | 2.3 | |
| Pain | |||
| Yes | 8 | 18.2 | 44 (100) |
| No | 36 | 81.8 | |
| Pruritus | |||
| Yes | 8 | 18.2 | 44 (100) |
| Variables | n | % | Total (%) |
|---|---|---|---|
| Follow-up | |||
| Irregular | 9 | 20.5 | 44 (100) |
| Regular | 30 | 68.2 | |
| Lost to follow-up | 5 | 11.4 | |
| Recurrence | |||
| Present | 2 | 4.5 | 44 (100) |
| Absent | 37 | 84.1 | |
| Lost to follow-up | 5 | 11.4 | |
| Condition at 12 months | |||
| Need further session | 4 | 9.1 | 44 (100) |
| No need further session | 35 | 79.5 | |
| Not known | 5 | 11.4 | |

- (a) A 35-year-old female with left ear lobe keloid. (b) More than 90% clearance after 6 sessions of Erbium YAG laser with ILS. YAG: Yttrium aluminium garnet, ILS: intralesional steroid.
There was a significant change observed in VSS value when compared at baseline and VSS value after the 3rd and 6th sessions shown in Table 3. The mean value of VSS at baseline was 8.07, which was 5.02 after 3 sessions and 2.57 after 6 sessions [Figure 2a and b]. Furthermore, we have compared the relation of baseline size, site, and recurrence of keloid [Table 4] with VSS value after 6 sessions [Table 5] to know the percentage of change and its significance in our study [Figure 3a-c].
| VSS baseline | VSS - After 3 sessions | VSS - After 6 sessions | ||||
|---|---|---|---|---|---|---|
| Count | Column n % | Count | Column n % | Count | Column n % | |
| 0–3 | 0 | 0.0 | 8 | 19.5 | 25 | 80.6 |
| 4–6 | 11 | 25.0 | 26 | 63.4 | 4 | 12.9 |
| >6 | 33 | 75.0 | 7 | 17.1 | 2 | 6.5 |
| Total | 44 | 100.0 | 41 | 100.0 | 31 | 100.0 |
VSS: Vancouver scar scale
| VSS baseline | ||||
|---|---|---|---|---|
| 4–6 | >6 | |||
| Count | Row n % | Count | Row n % | |
| Site | ||||
| Axilla | 0 | 0.0 | 1 | 100.0 |
| Back | 0 | 0.0 | 4 | 100.0 |
| Breast | 2 | 66.7 | 1 | 33.3 |
| Buttock | 1 | 50.0 | 1 | 50.0 |
| Chest | 2 | 18.2 | 9 | 81.8 |
| Earlobe | 4 | 66.7 | 2 | 33.3 |
| Face | 1 | 16.7 | 5 | 83.3 |
| Forearm | 0 | 0.0 | 1 | 100.0 |
| Hand | 1 | 20.0 | 4 | 80.0 |
| Knee | 0 | 0.0 | 1 | 100.0 |
| Legs | 0 | 0.0 | 2 | 100.0 |
| Shoulder | 0 | 0.0 | 1 | 100.0 |
| Waist | 0 | 0.0 | 1 | 100.0 |
| Recurrence | ||||
| Nil | 9 | 32.1 | 19 | 67.9 |
| Present | 0 | 0.0 | 2 | 100.0 |
| Size | ||||
| <3 | 9 | 45.0 | 11 | 55.0 |
| 3–5 | 2 | 11.8 | 15 | 88.2 |
| Above 5 | 0 | 0.0 | 7 | 100.0 |
VSS: Vancouver scar scale
| VSS - after 6 sessions | ||||||
|---|---|---|---|---|---|---|
| 0–3 | 4–6 | > 6 | ||||
| Count | Row n % | Count | Row n % | Count | Row n % | |
| Site | ||||||
| Axilla | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Back | 1 | 33.3 | 1 | 33.3 | 1 | 33.3 |
| Breast | 3 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Buttock | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Chest | 6 | 75.0 | 2 | 25.0 | 0 | 0.0 |
| Earlobe | 5 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Face | 3 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Hand | 3 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Knee | 0 | 0.0 | 0 | 0.0 | 1 | 100.0 |
| Legs | 1 | 50.0 | 1 | 50.0 | 0 | 0.0 |
| Shoulder | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| Recurrence | ||||||
| Nil | 23 | 82.1 | 3 | 10.7 | 2 | 7.1 |
| Present | 1 | 50.0 | 1 | 50.0 | 0 | 0.0 |
| Size | ||||||
| <3 | 15 | 100.0 | 0 | 0.0 | 0 | 0.0 |
| 3–5 | 10 | 90.9 | 1 | 9.1 | 0 | 0.0 |
| Above 5 | 0 | 0.0 | 3 | 60.0 | 2 | 40.0 |
VSS: Vancouver scar scale

- (a) A 45-year-old female with chest keloid for 2 years. (b) 62.5% reduction in modified vancouver scar scale (VSS) after 6 treatment sessions.
![(a) A 14-year-old boy with extensive midline chest keloids (vancouver scar scale [VSS]: 12). (b) After 3 sessions of Erbium YAG laser with ILS. (c) VSS reduced to 4 after 6 sessions. YAG: Yttrium aluminium garnet, ILS: intralesional steroid.](/content/173/2025/0/1/img/JCAS-69-2024-g003.png)
- (a) A 14-year-old boy with extensive midline chest keloids (vancouver scar scale [VSS]: 12). (b) After 3 sessions of Erbium YAG laser with ILS. (c) VSS reduced to 4 after 6 sessions. YAG: Yttrium aluminium garnet, ILS: intralesional steroid.
The VSS was divided into two categories of ≤6 and >6 for better analysis of the outcome. At baseline, VSS ≤6 was seen in 30% of patients and >6 in 70% of cases; after 3 sessions VSS ≤6 was in 83.3% and >6 in 16.7% of cases; after 6 sessions VSS ≤6 in 93.3% patients and >6 in 6.7% cases, which thereby showed a significant reduction in the VSS score by the end of 6 sessions. The distribution of study participants at baseline, 3rd session, and 6th session is depicted in Figure 4, which showed that a greater number of study participants had VSS of 8 at the baseline, VSS of 4 after 3 sessions, and VSS of 2 in this study.
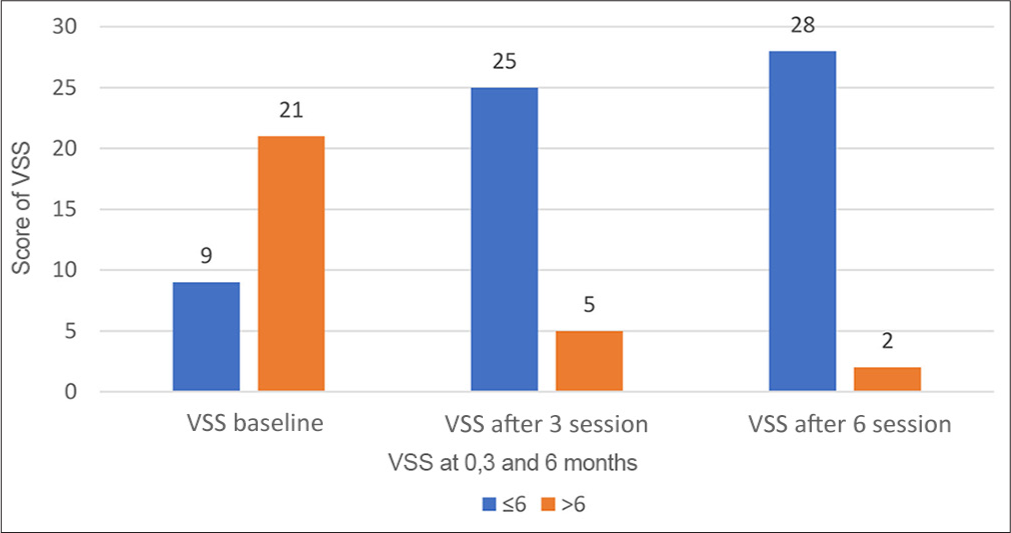
- Distribution of study participants at vancouver scar scale (VSS) baseline, 3rd and 6th session.
Most patients showed improvement of keloid in terms of scar height, vascularity, contour, reduced pruritus, and pain [Figures 5a and b; 6a and b]. No patient reported worsening of their keloid, increase in pain, or infection. Giving intralesional steroid injections during follow-up visits became easy, had no spillage, was relatively painless, and required less dose with each session.
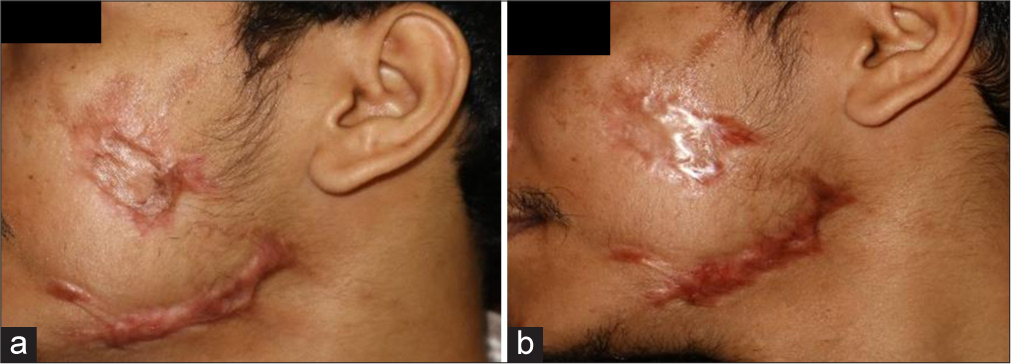
- (a) A 31-year-old male with post-traumatic keloid over left cheek. (b) Reduction in vancouver scar scale (VSS) from 6 to 2 after 6 sessions.
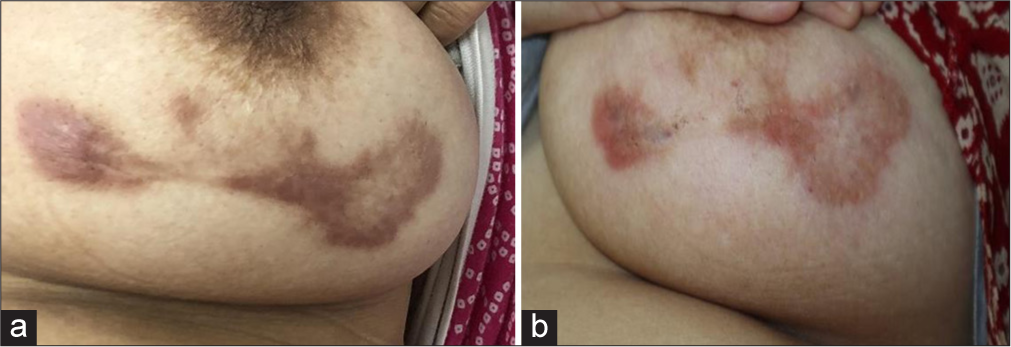
- (a) A 40-year-old female with keloid over breast. (b) Significant reduction in erythema and induration after completion of treatment.
DISCUSSION
As there is no single best treatment for keloids, an increasing number of studies are being conducted by combining different modalities for a synergistic effect, as these combinations provide favorable outcomes compared to monotherapy. Many previous studies for keloids were focused on pulsed dye lasers5-7 and ablative co2 lasers8,9 but numerous studies have reported the effectiveness of non-ablative fractional lasers (NAFLs).10-13
NAFL, despite causing collagenolysis and neocollagenesis, also reduces the fibrotic changes in the scar, thereby causing less hardening and thickening. A review of several studies showed that NAFL also efficiently improved skin outcomes with less pigmentation and vascular changes in scars.14,15
Erbium glass laser is a non-ablative, mid-infrared range laser that targets intracellular water to a depth of 0.4–2 mm. At this wavelength, there is minimal absorption of energy by melanin, hence it is safer to use in darker skin types. Its emitted wavelength of 1540 nm shows high water absorption. This is a flashlamp-pumped system. The wavelength is obtained from a specific co-doped Yb-Er: phosphate glass material, optimized for high-efficiency pumping absorption, and delivered by optic fiber.16
Erbium glass laser creates non-contiguous columns of microscopic thermal zones (MTZ) in the dermis.17 These zones produce localized epidermal necrosis and collagen denaturation at 125 or 250 MTZ/cm2. As the tissue surrounding each MTZ column is intact, the surrounding normal epidermal and dermal cells migrate into the zone of damage to produce rapid healing. This wound-healing response has been shown by conducting immunohistochemical studies and by verifying the accumulation of collagen III, heat shock proteins 70, 72, and 47 and alpha-smooth muscle cell actin fibers.18 An added advantage of this laser is that it creates microchannels, which aid in the even distribution of ILS, apart from making the keloid tissue soft and pliable.
When compared with the study done by Shin et al.,4 where the POSAS scale was used for assessment, a significant difference in terms of fewer treatment sessions in the combined group (treated with 1550 nm erbium glass laser and ILS) was seen and also a significant difference in the recurrence rate in the combined group was seen as compared to control group (treated with ILS alone). These findings are similar to our current study. In another study conducted by Verhaeghe et al.,10 to evaluate the efficacy of 1540-nm NAFL therapy in the treatment of hypertrophic scars, it was revealed that there was a significant difference on the physician global assessment scale at baseline (P = 0.006) and that of 3 (P = 0.02) months after last treatment.
This synergistic approach addressed multiple aspects of keloid pathogenesis, including inflammation, fibroblast proliferation, and extracellular matrix deposition, thereby improving treatment outcomes, reducing recurrence rates, and improving the quality of life for affected individuals. Furthermore, the erbium glass laser facilitated targeted delivery of corticosteroids into the dermis, enhancing their penetration and bioavailability, thereby reducing the dose and number of sessions of ILS required and so potentially decreasing the side effects of corticosteroid therapy, including skin atrophy, telangiectasia, and hypothalamic-pituitary-adrenal axis suppression.
Limitations
No control groups were assigned in our study. We need more comparative studies with a relatively larger sample size to assess the efficacy of combination therapy of erbium glass laser with ILS.
CONCLUSION
The combination of erbium glass laser therapy and intralesional corticosteroid injections represents a promising approach for maximizing keloid treatment efficacy. This synergistic modality offers superior keloid size reduction, symptomatic improvement, and reduced recurrence rates compared to monotherapy alone. Adverse effects are generally manageable and transient. Further prospective studies are warranted to validate these findings and optimize treatment protocols for keloid management.
Author contributions
All authors have contributed towards concept, design, data analysis, manuscript preparation and review.
Ethical approval
The Institutional Review Board approval is not required as this is a retrospective study analysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Morphological and immunochemical differences between keloid and hypertrophic scar. Am J Pathol. 1994;145:105-13.
- [Google Scholar]
- Medical and surgical therapies for keloids. Dermatol Ther. 2004;17:212-8.
- [CrossRef] [PubMed] [Google Scholar]
- Standard guidelines of care: Keloids and hypertrophic scars. Indian J Dermatol Venereol Leprol. 2011;77:94-100.
- [CrossRef] [PubMed] [Google Scholar]
- Combination therapy using non-ablative fractional laser and intralesional triamcinolone injection for hypertrophic scars and keloids treatment. Int Wound J. 2019;16:1450-6.
- [CrossRef] [PubMed] [Google Scholar]
- New combination of triamcinolone, 5-fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg. 2006;32:907-15.
- [CrossRef] [PubMed] [Google Scholar]
- Prevention of thyroidectomy scars in Korean patients using a new combination of intralesional injection of low-dose steroid and pulsed dye laser starting within 4 weeks of suture removal. Dermatol Surg. 2014;40:562-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effectiveness of nonablative fractional laser versus pulsed-dye laser in thyroidectomy scar prevention. Ann Dermatol. 2014;26:615-20.
- [CrossRef] [PubMed] [Google Scholar]
- Therapeutic efficacy of intralesional steroid with carbon dioxide laser versus with cryotherapy in treatment of keloids: A randomized controlled trial. Dermatol Surg. 2016;42:1188-98.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of carbon dioxide laser ablation followed by intralesional steroids on keloids. J Cutan Aesthet Surg. 2011;4:2-6.
- [CrossRef] [PubMed] [Google Scholar]
- Nonablative fractional laser resurfacing for the treatment of hypertrophic scars: A randomized controlled trial. Dermatol Surg. 2013;39:426-34.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of nonablative fractional laser treatment in scar reduction. Lasers Med Sci. 2017;32:1629-35.
- [CrossRef] [PubMed] [Google Scholar]
- Combined therapeutic strategies for keloid treatment. Dermatol Surg. 2019;45:802-10.
- [CrossRef] [PubMed] [Google Scholar]
- Fractional nonablative 1540 nm laser resurfacing for thermal burn scars: A randomized controlled trial. Lasers Surg Med. 2009;41:189-95.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of burn scars with the 1,550 nm nonablative fractional erbium laser. Lasers Surg Med. 2012;44:441-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effectiveness of ablative and non-ablative fractional laser treatments for early stage thyroidectomy scars. Arch Plast Surg. 2016;43:575-81.
- [CrossRef] [PubMed] [Google Scholar]
- Nonablative laser and light treatments: Histology and tissue effects--a review. Lasers Surg Med. 2003;33:30-9.
- [CrossRef] [PubMed] [Google Scholar]
- The spectrum of laser skin resurfacing: Nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol. 2008;58:719-37.
- [CrossRef] [PubMed] [Google Scholar]
- Immunohistochemical evaluation of the heat shock response to nonablative fractional resurfacing. J Biomed Opt. 2010;15:68002.
- [CrossRef] [PubMed] [Google Scholar]







