Translate this page into:
Microneedling with autologous platelet-rich plasma versus topical insulin for treating postacne scars: A split-face comparison
*Corresponding author: Alpana Mohta, Department of Dermatology, Venereology and Leprology, Sardar Patel Medical College, Bikaner, Rajasthan, India. dralpanamohta10@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mohta A, Yadav MK, Ghiya BC. Microneedling with autologous platelet-rich plasma versus topical insulin for treating postacne scars: A split-face comparison. J Cutan Aesthet Surg. 2024;17:340-2. doi: 10.4103/JCAS.JCAS_20_23
Abstract
Post-acne atrophic scars (PAS) are a common complication of acne, and their treatment can be limited in people of color due to dyspigmentation and scarring risks. This split-face study compared the efficacy of microneedling with topical insulin (TI) on one side of the face with microneedling with platelet-rich plasma (PRP) on the other side for the treatment of PAS. The study included 50 participants with Fitzpatrick skin types III to VI who had never been treated for PAS. Both sides of the face showed significant improvement, with the left side being treated with TI showing a 52% improvement and the right side being treated with PRP showing a 28% improvement. The treatment was well-tolerated, with no significant adverse effects, and no changes in blood glucose levels were observed. The researchers suggest that combining TI or PRP with microneedling can improve PAS treatment, with TI being a superior option due to its ease of use, low cost, and noninvasive nature.
Keywords
Post acne scars
Platelet-rich plasma
Topical insulin
Micro-needling
Postacne atrophic scars (PAS) are a common complication of acne. Peels, platelet-rich plasma (PRP), subcision, dermabrasion, lasers, punch methods, and fillers can be beneficial to PAS. However, many of these can produce dyspigmentation and scarring, limiting their use, especially in people of color.1 In this population, microneedling is safer and is frequently paired with PRP to boost efficacy, but PRP therapy is pricey and requires more technical expertise.2
This split-face study compared the efficacy of microneedling with PRP on one side of the face (group A), with microneedling with topical insulin (TI) on the other side for the treatment of PAS. We initiated the study after obtaining due institutional ethical approval. The study included 50 participants with Fitzpatrick skin types III–VI who had never been treated for PAS. The following were criteria for exclusion: abnormal blood glucose levels, active acne or infections (herpes, impetigo, seborrheic dermatitis, verruca, molluscum, etc.), pregnancy or lactation, current use of isotretinoin, a history of keloidal propensity, and bleeding diathesis.
Microneedling was done on both sides of the face with a 1.5-mm derma roller with 192 needles on a roller drum. On the left side, we administered 1–2 mL of TI (Human Actrapid Insulin, 40 IU/L solution; Novo Nordisk India Pvt Ltd, Bangalore, India). The right side received 1–2 mL of autologous PRP prepared using standard technique. After 30 min, the face was cleansed, and an ice pack was administered to the treated areas. The procedure was carried out under sterile conditions and with topical anesthetic. The blood glucose levels of cases were repeated 2 h before and 2 h after the procedure. There were no harmful consequences observed. Patients were urged to use skin-protective measures. All patients underwent five microneedling treatments monthly and were followed up for 3 months following the last treatment. The Global Acne Scarring System was used to evaluate the treatment’s efficacy.
All 50 cases completed the study. The PAS on the left side of the face improved by 52%, and the right side improved by 28% [Figure 1a-d]. A paired t test revealed that both sides of the face improved significantly (left side: P = 0.01; right side: P = 0.04). An unpaired t test revealed that both sides of the face improved similarly, although ice pick and boxcar scars responded better to TI therapy. The results were maintained until the last 3-month follow-up.
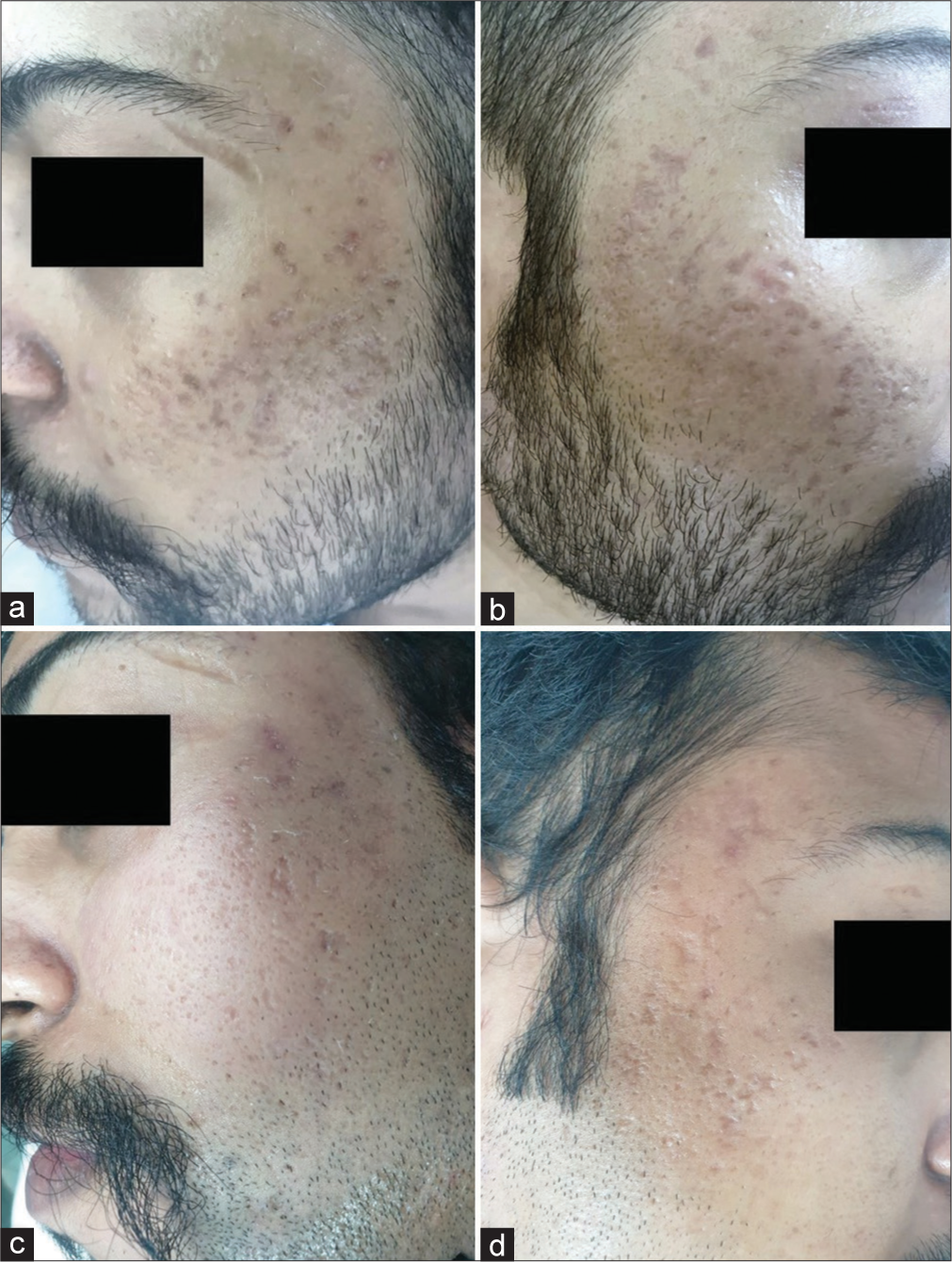
- (a) and (b) Multiple postacne atrophic scars on both sides of the face. (c) and (d) Significant improvement on both sides of the face following microneedling with topical insulin (left side) and platelet-rich plasma (right side).
The treatment was well-tolerated, with no significant adverse effects. Transient erythema, pain, and edema were observed in only a small number of patients, but there was no dyspigmentation or scarring. The researchers did not observe any changes in blood glucose levels.
Type I collagen predominates over type III collagen in a mature PAS.3 Collagen is deposited in a typical lattice pattern following microneedling, and growth factors from PRP can improve PAS healing. Pawar et al.4 highlighted that to enhance vascular endothelial growth factor, TI activates the phosphatidylinositol 3-kinase/protein kinase B (Akt) pathways. Following TI, the production and maturation of collagen fibers, primarily type III, occur in a basket weave-like pattern (similar to normal skin) rather than a crisscross pattern (similar to scar tissue). As a result, combining PRP or insulin with microneedling can improve PAS treatment.
The study’s limitations include limited sample size, a lack of separate assessment of each treatment modality, and a short follow-up period. Employing better dermal delivery systems like tattoo machines could lead to a better depth of drug deposition, as suggested by Ghanian et al.5
In conclusion, combining TI or PRP with microneedling may increase PAS in people of color while still being safe. However, because of its ease of use, low cost, and noninvasive nature, TI is a superior option to PRP.
Authors’ contributions
Alpana Mohta: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Manoj K. Yadav: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Bhikam C. Ghiya: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Ethical approval
The study was conducted after obtaining due approval from the institutional ethical board(s).
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Microneedling in skin of color: A review of uses and efficacy. J Am Acad Dermatol. 2016;74:348-55.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma and its utility in the treatment of acne scars: A systematic review. J Am Acad Dermatol. 2019;80:1730-45.
- [CrossRef] [PubMed] [Google Scholar]
- Acne scars: pathogenesis, classification and treatment. Dermatol Res Pract. 2010;2010:893080.
- [CrossRef] [PubMed] [Google Scholar]
- Microneedling with autologous platelet-rich plasma versus microneedling with topical insulin in the treatment of postacne atrophic scars: A simultaneous split-face comparative study. J Am Acad Dermatol. 2021;84:810-1.
- [CrossRef] [PubMed] [Google Scholar]
- “Microneedling with autologous platelet-rich plasma versus microneedling with topical insulin in the treatment of postacne atrophic scars: A simultaneous split-face comparative study. ” J Am Acad Dermatol. 2021;85:e395-6.
- [CrossRef] [PubMed] [Google Scholar]






