Translate this page into:
Nail Surgery: General Principles, Fundamental Techniques, and Practical Applications
Address for correspondence: Dr. Catarina Queirós, Serviço de Dermatologia do Hospital de Santa Maria, Centro Hospitalar e Universitário de Lisboa Norte, Avenida Prof. Egas Moniz, Lisbon 1649-035, Portugal. E-mail: catarina.squeiros@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Despite being an integral part of dermatologic surgery, nail surgery is infrequently performed in daily practice. Indeed, it is frequently considered difficult, time-consuming, and the results take a long time to be observed. Nonetheless, nail pathology is a frequent cause of dermatology consultation, so dermatologists should be familiar with its diagnosis and therapeutic approach, which often involves surgical procedures. This article provides a review of nail surgery, focusing on the anatomy of this region, anesthesia of the ungual apparatus, common surgical techniques, reconstruction of defects in these locations, and a general approach to the most frequently encountered conditions in clinical practice.
Keywords
Dermatologic surgery
nail diseases
nail surgery
PART I
Introduction
Despite being an integral part of dermatologic surgery, nail surgery is infrequently performed as it is considered by many practitioners to be difficult and time-consuming. However, if we consider the frequency and diversity of nail pathologies, it is easy to understand that dermatologists should be familiar with, at least, the most frequent procedures.[1] In this sense, a thorough knowledge of nail anatomy is essential, as this has clear implications not only in the choice of the technique but also when considering the expected results.[2] If performed correctly, nail surgery leads to satisfying functional and aesthetic results in the majority of instances.[3] This article aims, therefore, at providing a review on nail surgery, focusing on the anatomy, anesthesia, and most common surgical techniques used in this particular anatomic and functional area.
Anatomy
The nail organ consists of four different components: the nail plate, nail folds, matrix, and nail bed [Figure 1]. The nail is also intimately associated with the distal interphalangeal joint and its capsule, ligaments, and tendons.[2]
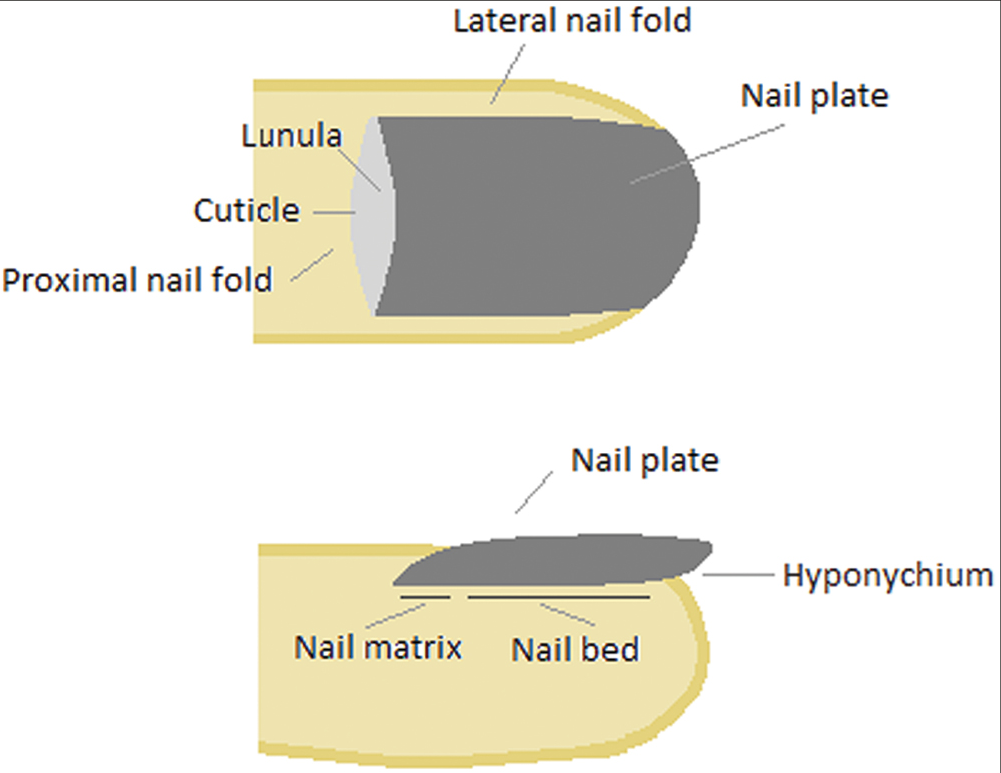
- Anatomy of the nail apparatus: (A) front view and (B) lateral view
The nail plate arises from the matrix and is a laminated keratinized structure overlying the nail bed and matrix. It has longitudinal ridges that fit complementary grooves on the nail bed, to which it is bonded. Moreover, the nail plate is curved in both the longitudinal and transverse axes, which allows it to be embedded in nail folds at its proximal and lateral margins, providing further attachment.[1] The proximal nail fold, in particular, is bound to the nail plate through the eponychium, the free end of which is the cuticle. These structures provide a protective layer over the matrix, which, if damaged, has a risk of permanent nail scarring.[1] A distal nail fold forms only when the overlying nail plate is lacking.[2]
The tissues under the nail plate are divided into the matrix (15–25%) and the nail bed (75–85%). Clinically, the distal part of the matrix is visible in some digits as the whitish lunula. The matrix is responsible for the production of all or most of the nail plate. With regard to this function, the proximal matrix has a more important role, being responsible for the production of around 80% of the nail plate, mainly its dorsal portion[2]; the distal matrix, the place where most melanocytes are located, is responsible for the production of only around 20% of the nail plate, mainly its ventral aspect.[45] Therefore, surgery to the distal matrix is less likely to cause scarring than more proximal surgery. The matrix also has lateral matrix horns that reach further proximally than the central part of the matrix. This is important when taking a lateral longitudinal nail biopsy, as explained later.
The nail bed is the distal continuation of the matrix, extending from the distal margin of the lunula to the hyponychium. The hyponychium, in turn, marks the end of the epithelial nail organ and is important for a healthy nail bed-nail plate adhesion, protecting against the penetration of foreign bodies and pathogens.[12]
Due to the proximal-to-distal growth of the matrix, biopsies of this structure should always be done with the long axis of the biopsy in the transverse direction, in order to avoid a longitudinal scar that would not produce nail substance and cause a split in the nail. Moreover, due to its sensitivity to trauma, any defect wider than 3 mm leads to permanent nail dystrophy.[2]
Arterial supply
A rich arterial supply and a dense innervation provide various sensory and autonomic functions to the nail organ.[2] The arterial supply of fingers and toes is largely the same. Four arteries supply each digit, two on either side. The volar digital arteries provide the main blood supply to the digits. At approximately the level of the distal interphalangeal joint, the volar and dorsal arteries form anastomoses. The dorsal nail fold arch (superficial arcade) supplies the nail fold and extensor tendon insertion. The subungual region is supplied by distal and proximal subungual arcades. This complex and vast vascular network around the nail unit provides a valuable arterial supply in the face of surgery or trauma [Figure 2].[1]
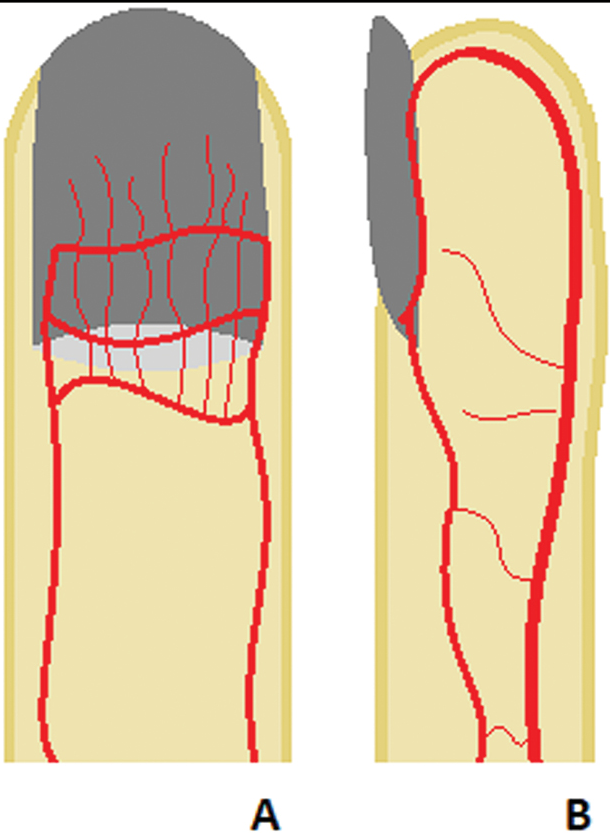
- Vascular supply of the nail apparatus. (A) frontal view with the three arcades that give rise to longitudinally running fine vessels for the proximal nail fold, matrix, and nail bed. (B) Lateral view highlighting the palmar artery, which supplies most of the blood to the nail apparatus and anastomoses with the thinner dorsal artery
Venous drainage
Venous drainage of the finger involves deep and superficial systems. The deep system corresponds to the arterial supply. The dorsal and palmar digital veins exist superficially and form a prominent branching network, particularly on the dorsal aspect.[1]
Nerve supply
The innervation is variable between the different digits. The nails of the long fingers are innervated by the volar proper digital nerves, which divide distally into three branches, whereas the thumb and little finger nails are innervated by the dorsal proper digital nerves [Figure 3].[2] Regarding the toes, the periungual soft tissues are innervated by dorsal branches of paired digital nerves. Corresponding palmar or plantar branches supply the palmar and plantar surfaces, including the digit pulp up to the margin with the hyponychium.[1]

- Innervation of the nail apparatus. (A) The thumb and fifth finger are innervated mainly by the dorsal proper digital nerve. (B ) The remaining fingers are innervated mainly by the volar proper digital nerves
Before surgery
As with any surgery, adequate patient selection is critical to achieve the desired results. Therefore, a thorough patient history should be collected in order to avoid unnecessary complications and to identify potential contraindications, such as serious impairment of the peripheral arterial blood supply. It is also important that the patient understands the risks of the procedure and has realistic expectations regarding the final result and the postoperative period. Preoperative examinations are reserved to particular cases.[3]
Nail surgery also requires several particular instruments that are not usually used in common dermatologic surgery. These include a dental spatula or Freer elevator, which is useful to separate the nail plate from the underlying nail bed and the overlying cuticle; a nail-extraction forceps, which is used subsequently for avulsion of the nail plate; a nail splitter, which is particularly useful for the partial nail avulsion procedure; a nail clipper, which is used for nail trimming; and a tourniquet, which provides hemostasis during the surgery.
Regarding closure after surgery, monofilament sutures are usually employed, mainly absorbable but also nonabsorbable in some settings. In general, defects with a diameter of less than 3 mm do not require a surgical closure. For proximal nail fold and lateral nail fold surgery, absorbable sutures (such as Vicryl®) should be used, usually 4-0 for toes and 5-0 for fingers. Defects in the nail matrix and bed should be sutured with a thin absorbable suture (such as Vicryl® 6-0 for the former and Vicryl® 5-0 for the latter).
Anesthesia
The two most commonly used techniques for nail anesthesia are the distal wing block and the traditional digital block [Figure 4]. The distal wing block involves direct anesthesia infusion into the periungual tissues and digital tip, with an almost immediate effect; hemostasis results from volume load (rather than from the use of epinephrine).[6] Several types of distal nail blocks can be performed, which include the distal digital block (needle insertion 3 mm proximal to the junction of the proximal and lateral nail fold), distal anesthesia through the proximal nail fold (needle insertion in the middle of the proximal nail fold), and distal anesthesia through the hyponychium (needle insertion in the lateral hyponychial area).[7]
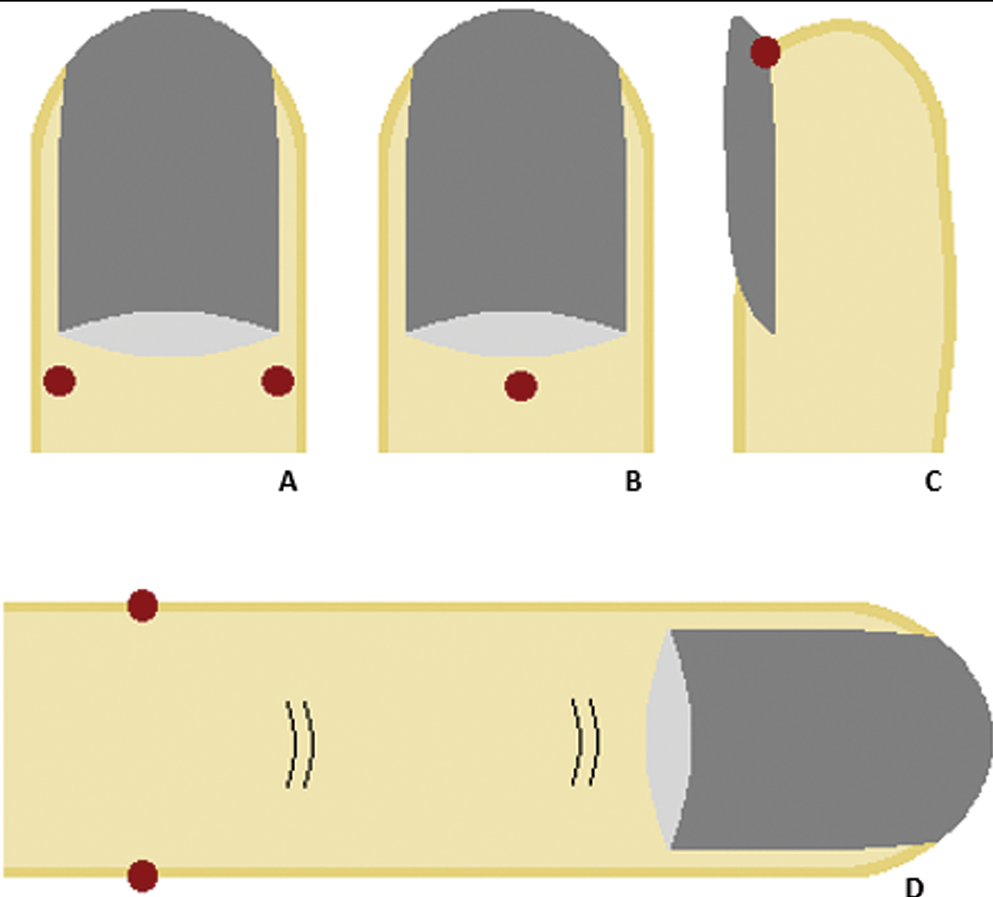
- Anesthesia of the nail apparatus. (A) Distal digital block. (B) Distal anesthesia through the proximal nail fold. (C) Distal anesthesia through the hyponychium. (D) Traditional digital anesthesia
The traditional digital anesthesia is a nerve block of the dorsal and ventral lateral digital nerves. The anesthetic is infused in the lateral digit, between the metacarpophalangeal/metatarsophalangeal joint and the proximal interphalangeal joint.[6] This technique requires several minutes to achieve its effect and may be used with low concentrations of epinephrine to aid in hemostasis, in patients without comorbidities such as diabetes mellitus, Raynaud’s disease, peripheral vascular disease, and tobacco use.[68]
In both techniques, needle insertion is the most painful aspect, and it can be diminished by the application of topical cryogen spray, which is used for 1 to 2 sec prior to this moment. Lidocaine is the most commonly used anesthetic for distal wing blocks; ropivacaine and bupivacaine may be used for traditional digital blocks. Once anesthetized, a tourniquet may be applied in the base of the digit, in order to achieve a bloodless field.[6] Which technique of digital anesthesia is used depends on the type of surgery and personal preference.[36]
Surgical techniques
Intralesional injection
Intralesional injection of corticosteroids is a useful therapy for several inflammatory diseases of the nail unit, such as psoriasis, lichen planus, and chronic paronychia. In general, nail fold and matrix injection is easier, less painful, and more effective than nail bed injection, and it should therefore be the chosen approach. In the case of mild nail bed disease, proximal nail fold and matrix injections may also be helpful, as the corticosteroid diffuses through adjacent tissues.[6] Besides corticosteroids, various other drugs can be injected in the nail unit. These include methotrexate, bleomycin, and cyclosporine, among others.[9]
As in anesthesia, the pain associated with needle insertion can be diminished by the application of a topical cooking spray. A 30-gauge needle is usually used to inject 0.05 to 0.1 mL of triamcinolone 2.5 mg/mL, diluted with plain lidocaine. The injections are usually repeated at monthly intervals, although different schemes have been proposed. When a desired improvement is seen, the frequency of injections is tapered in order to maintain a response and prevent relapses.[69] In the case of methotrexate injections, the intervals between treatments are shorter than for the other drugs.[9]
Ungual biopsy
Although not commonly performed, nail biopsies are the gold standard for the diagnosis of several nail disorders.[3] In this setting, biopsies can be performed in the matrix, nail bed, and plate [Table 1].
| Type of biopsy | Indications | Advantages | Disadvantages |
|---|---|---|---|
| Nail bed biopsy | Diagnosing inflammatory, infectious, and neoplastic disorders | Partial nail plate avulsion usually possible
No need for repair Generally heal without permanent dystrophy or scarring |
Not suitable for diagnosis of melanonychia |
| Matrix biopsy | Workup of melanonychia and nail melanoma | Total nail plate avulsion is neither performed nor required | Risk of permanent dystrophy |
| Nail fold biopsy | Diagnosis of neoplasms, chronic paronychia, or connective tissue diseases | Primary closure easily achieved | Risks matrix damage and permanent dystrophy due to the proximity to the matrix |
| Nail plate biopsy | Diagnosis of onychomycosis or other nail dermatoses | No need for suturing
No risk of dystrophy |
Not suitable for diagnosis of melanonychia |
| Shave biopsy | Sample wide pigmented bands that are presumably benign | Heals with minimal scarring | Occasional longitudinal erythronychia or superficial nail plate longitudinal thinning |
Nail bed biopsy
Nail bed biopsies are useful for diagnosing inflammatory, infectious, and neoplastic disorders. In most instances, partial nail plate avulsion is possible and avoids a more invasive total plate avulsion.[10] A 3-mm punch is usually adequate, but alternatively one can perform a fusiform biopsy that is oriented longitudinally.[3] Forceps should not be used, as they tend to crush the tissue without providing additional benefit. These defects do not require repair and generally heal without permanent dystrophy or scarring, with only occasional onycholysis.[6]
Matrix biopsy
Matrix punch biopsies are particularly important in the workup of melanonychia and nail melanoma. In the case of larger lesions, an incisional biopsy can be performed; however, in this location, it should be oriented transversally in order to prevent a split nail.[3] In cases where a biopsy of the proximal matrix is needed, the possibility of permanent dystrophy even with a 3-mm punch should be explained to the patient, communicating the critical need to sample matrix epithelium in the appropriate clinical setting.[611] Nonetheless, as previously explained, most pigmented bands originate from the distal matrix and are, therefore, less prone to permanent scarring with punch biopsies. As in nail bed biopsy, the use of forceps is strongly discouraged. Total nail plate avulsion is neither performed nor required for this procedure, as adequate matrix sampling is easily accomplished without the trauma of plate avulsion. After specimen collection, the proximal nail fold is returned to its anatomic position over the proximal plate. Suturing, steri-stripping, or simply applying a pressure dressing are all appropriate options.[6]
Nail fold biopsy
The proximal nail fold is contiguous on its ventral surface with the proximal matrix and directly overlies the mid to distal matrix. Therefore, any procedure in this location risks matrix damage and permanent dystrophy. Nail fold biopsy is usually required in the setting of neoplasms, chronic paronychia or to help in the diagnosis of connective tissue diseases. To protect the underlying matrix, a nail elevator is inserted under the cuticle and directed proximally to the planned incision margins.[612] The biopsy is then undertaken, either with a punch or by performing a fusiform transverse elliptical incision, parallel to the relaxed skin tension lines and at least 3 mm beyond the distal interphalangeal joint, to avoid cutting the tendon.[4] The elevator is withdrawn, and the wound is usually left to heal by secondary intention.[6]
For lateral nail fold biopsy, the incision is made longitudinally along the lateral nail fold. After removal of the affected nail fold, primary closure of the surgical incision is easily achieved.[412]
Nail plate biopsy
A biopsy of the nail plate and a portion of the hyponychium may be useful for the diagnosis of onychomycosis or other nail dermatoses. This technique may be performed by using scissors or a scalpel to remove a wedge of tissue containing the distal hyponychium and the overlying nail plate. Alternatively, a punch advanced to the periosteum can also be used to obtain a biopsy of the nail plate. Pressure or application of a small piece of oxidized cellulose is used to provide hemostasis.[46]
The Shave Biopsy
The shave technique is used to sample wide pigmented bands that are considered benign. Reflection of the proximal nail fold is initially performed, followed by a transverse cut at the border between the proximal and the middle third on the nail, which allows its opening in a trapdoor manner to expose the pigmented lesion.[37] Then, a superficial vertical incision is made to circumscribe the lesion to be sampled with 2-mm margins. The lesion is then shaved with a tangential movement of the blade. Superficial excisions of this type heal with minimal scarring, only with occasional longitudinal erythronychia or superficial nail plate longitudinal thinning.[7] This technique is, therefore, ideal for the diagnosis of superficial lesions, of both the matrix and the nail bed, with the additional benefit of also being often therapeutic.[3]
Nail plate avulsion
Avulsion of the nail plate may be necessary to expose the nail bed and the matrix, not only for diagnostic purposes but also as a therapeutic intervention. Regarding diagnosis, nail avulsion may be undertaken as a preliminary step for exploration of the nail bed and the nail matrix or as a means to enable the performance of a biopsy on the nail bed or the matrix. As a therapeutic procedure, nail avulsion is frequently undertaken before a chemical or surgical matricectomy and in cases of ingrown nails or onychogryphosis, chronic onychomycosis, traumatic nail injuries, chronic paronychia, retronychia, pincer nails, or tumors of the nail apparatus.[13]
Partial nail plate avulsions
Partial nail plate avulsion removes or reflects only the portion of the nail plate that is required to achieve adequate exposure of the underlying anatomy, and it should always be preferred if feasible, as total nail plate removal may result in prolonged pain and morbidity. Several types of partial nail avulsions can be performed, according to individual circumstances.[37,1214]
Distal avulsions
Distal avulsions are used to distal nail bed surgical approaches. They may be central, lateral, or involve avulsion of the distal half of the nail plate and can be used to explore the distal nail bed, remove a foreign body, or perform a biopsy. The portion of the nail plate to be avulsed is freed from its nail bed and attachment by inserting a nail elevator between the nail bed and the nail plate, which is then sectioned to the desired size.[714]
Proximal avulsions
Proximal avulsions are used to expose the matrix; they may involve the whole proximal nail plate, one third, one half, or only a lateral portion of the nail plate. The nail plate is freed from its matrix and proximal nail fold attachment by inserting the nail elevator between the proximal nail fold and the nail plate. Then, the nail plate is freed from the distal nail matrix laterally by inserting the nail elevator in the lateral nail sulcus, at the level of the lunula. The nail plate is partially cut transversally and lifted up to perform surgery. After surgery, the nail plate is either removed or positioned back in place. If repositioned, a 2-mm transversal cut may be needed for drainage.[7]
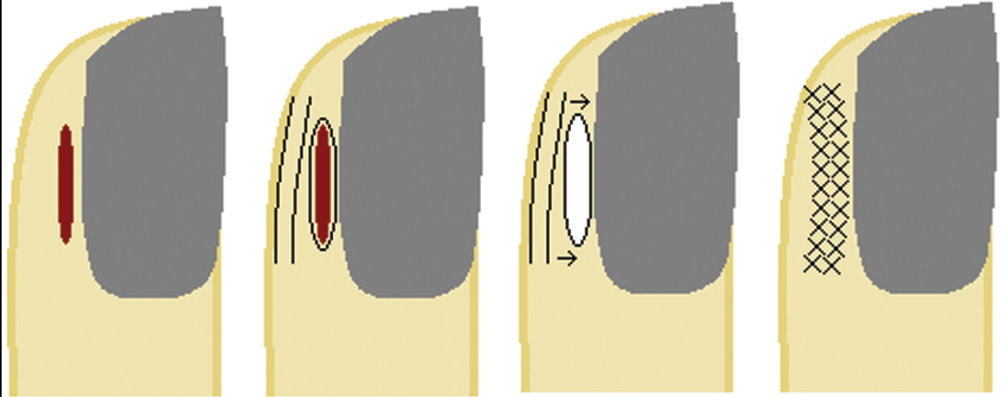
Longitudinal avulsions
Longitudinal avulsions may be used to expose the nail bed or the matrix in the lateral or central aspect of the nail. Initially, the nail plate and the proximal nail fold are separated with the use of a nail elevator, which is pushed back toward the cuticle and laterally dislodged. Then, the elevator is introduced under the nail plate at the level of the hyponychium and pushed toward the lunula, in order to separate the nail plate from the nail bed. The nail plate is then sectioned and removed with a mosquito hemostat or a nail-pulling forceps.[7]
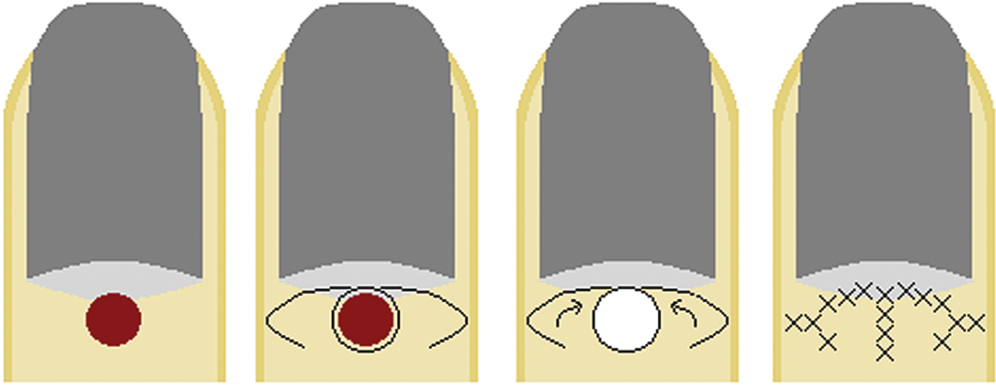
Window nail plate avulsion
Window nail plate avulsions may be used for localized procedures of the central nail bed or distal matrix, such as the evacuation of hematomas, the removal of foreign bodies, or to biopsy a neoplasm located in the nail bed. A 5-mm circular punch is used to drill the nail plate, which is then removed as a lid.[714]
Trap door technique
This type of avulsion starts by undermining the free edge of the nail plate with a nail elevator. The instrument is advanced proximally until the nail plate has been completely detached from the underlying bed and matrix. The nail plate is then lifted upward similar to a trap door, exposing the hyponychium, the entire nail bed, and the distal matrix. Slightly more proximal exposure can be gained by making two oblique incisions in the proximal nailfold. The trap door technique is ideal for a biopsy of longitudinal erythronychia, where the pathology originates in the distal matrix, and for cases of longitudinal melanonychia of a distal matrix origin.[14]
After partial nail plate avulsions, the nail plate should be repositioned back whenever possible, as it protects the wound and the nail bed or the matrix as a biologic dressing, decreasing postoperative morbidity.[14] If this is the case, openings should be made to ensure drainage. Nail repositioning should be avoided in the case of local infection, increased risk of surgical field contamination, or when there is a need for greater drainage.[7]
Total Nail Plate Avulsion
In some cases, total nail plate avulsion is necessary. After its removal, the plate is kept in povidone iodine. When surgery is completed, the nail plate is cut laterally (1 mm on each side) and proximally (3–4 mm) to facilitate postoperative drainage and is then repositioned. One stitch is placed laterally on each side to secure the lateral nail plate to the corresponding lateral nail fold.[37]
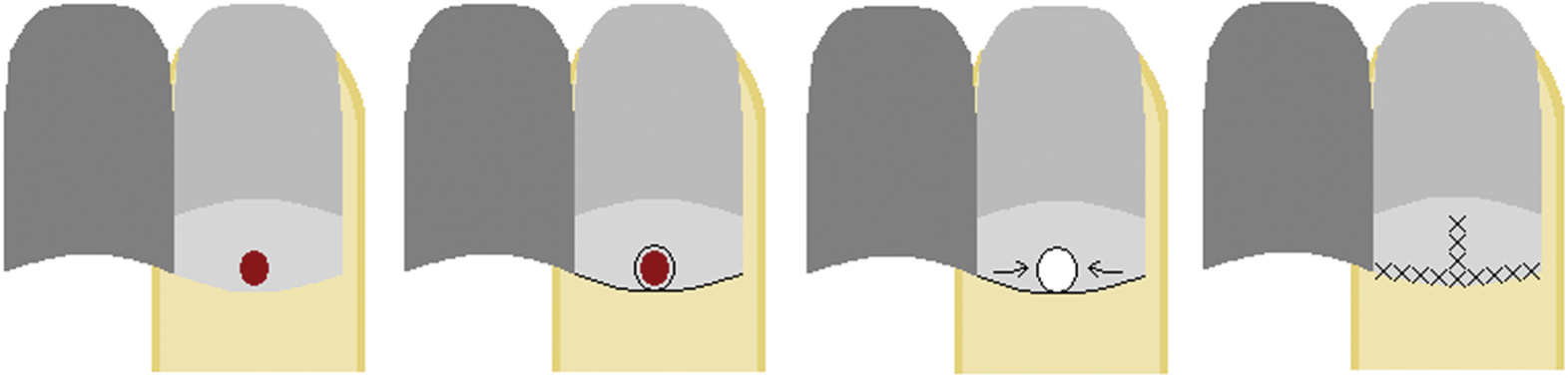
Matricectomy
Matricectomy is the destruction or removal of the nail matrix, thereby preventing regrowth of the nail plate. It can be performed as either a partial or total matricectomy. Partial matricectomy is the destruction of that portion of the nail matrix that is responsible for causing limited nail unit disease. Because only a portion of the matrix is removed, the uninvolved matrix remains viable and capable of producing a nail plate. On the other hand, total matricectomy removes the entire nail matrix, making it unable to regenerate a nail plate. Partial matricectomy is particularly helpful in the treatment of ingrown nails and persistent split nails, whereas total matricectomy is frequently applied in severely dystrophic or chronic painful nails such as pincer nails or onychogryphosis.[415]
In this section, the most common techniques used for matricectomy are discussed. Nonetheless, it is important to remember that there are other ways of destroying the nail matrix, such as chemical ablation, electrosurgery, and CO2 laser, among others.[15161718]
Partial (lateral) surgical matricectomy
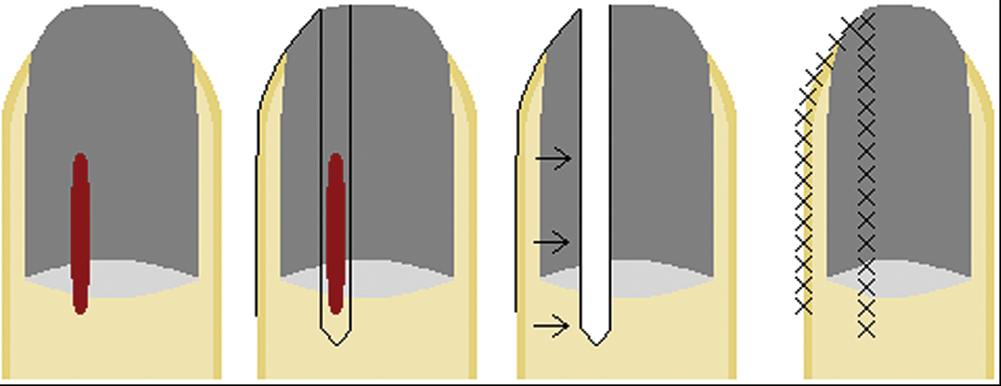
In partial matricectomy, the incision is made longitudinally from the most proximal portion of the matrix to the distal portion of the exposed matrix. This incision is then extended to the lateral nail fold and proximally along the nail groove to the lateral horn, which, if not removed, will result in a nail spicule [Figure 5]. Incisions are carried out on the depth of the periosteum, and the wedge of tissue containing the matrix is removed by using curved scissors.[4]

- Nail dystrophy after incomplete removal of the lateral matrix horn. A separated lamina of nail plate is observed laterally and separated from the main one, originating from one lateral matrix horn, which was not completely removed during previous matricectomy
Total surgical matricectomy
Total matricectomy involves complete removal of the matrix, from the proximal nail groove to the distal portion of the lunula, allowing the surgical wound to heal by secondary intention. The main disadvantage of scalpel excision matricectomy is the relatively high rate of nail plate regrowth in the lateral nail horn area, due to incomplete removal of the lateral matrix horns. Therefore, the proximal nail fold must be dorsally reflected in order to provide better exposure of these structures. After matricectomy, the proximal nail fold is repositioned and sutured at its junction with the lateral nail fold.[4]
Segmental phenolization
Selective nail unit destruction with phenol is a technique that is mainly used to correct lateral ingrowing nails of both juvenile and pincer nail types, with success rates around 95% and recurrence rates as low as 1.1% to 3.9%.[1920] The procedure begins with a unilateral or bilateral 3-mm longitudinal avulsion of the nail plate [Figure 6]. The lateral nail bed and matrix are then dried with a piece of gauze. The concave side of a 3-mm nail elevator is soaked in phenol (88%), with any excess phenol being absorbed on a piece of gauze. Then, the tiny phenol layer covering the inferior part of the elevator is applied to the lateral matrix, the ventral part of the proximal nail fold, and the corresponding nail bed. This procedure is usually repeated three to four times. A total phenol application time of 60 sec may be sufficient for complete destruction of the germinal nail matrix, although longer application times are usually employed (3 to 4 min).[20]
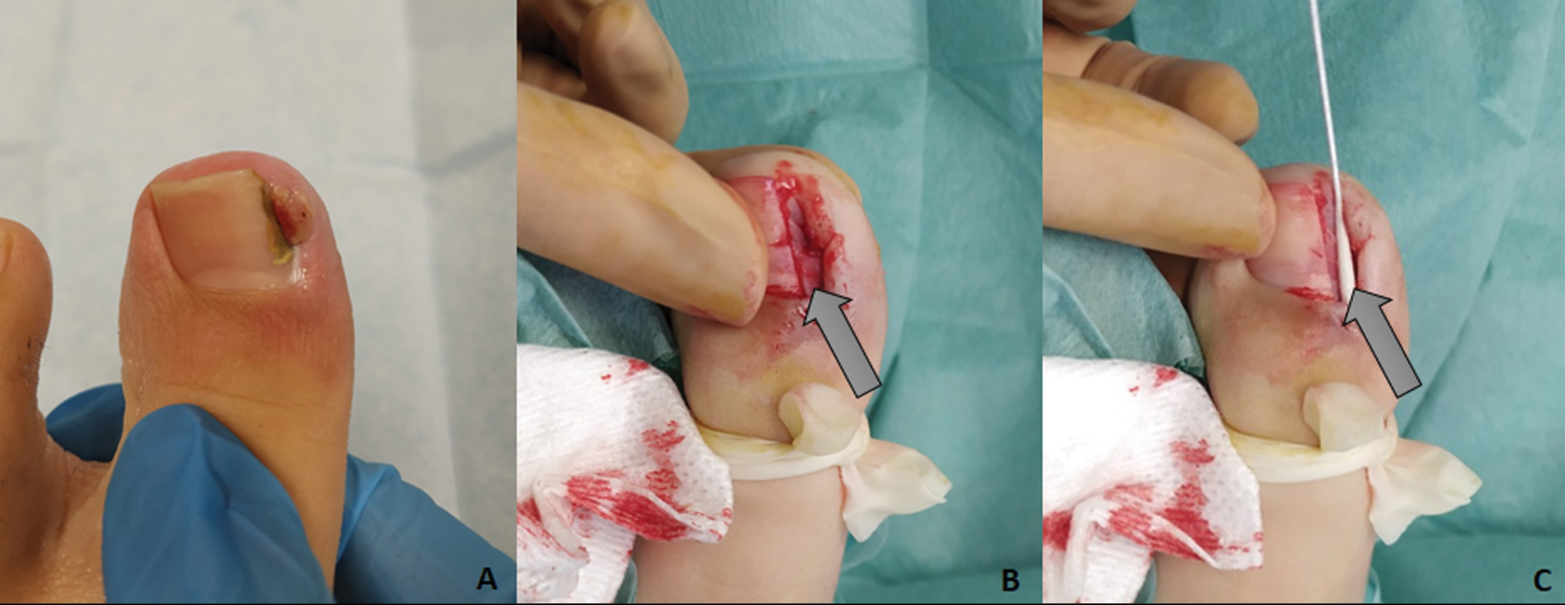
- Segmental phenolization: (A) Ingrown nail before surgery, (B) unilateral 3-mm longitudinal avulsion of the nail plate, and (C) phenol application
In this procedure, it is important to remember to treat the lateral horns of the matrix and to avoid contact of phenol with the surrounding skin, as it has toxic effects in this tissue.[7] This technique is relatively safe, simple, minimally traumatic, and successful, with no need for specialized instruments.[420] Moreover, it can be safely performed in children and patients with diabetes.[3]
Longitudinal matrix excision
Longitudinal matrix excision is a special type of matricectomy that is used for the excision of melanonychia. In this technique, the proximal nail matrix is exposed, and a longitudinal elliptic excision of the lesion is done, with incisions carried out on the depth of the periosteum. Small lesions may be closed without any undermining, whereas lesions larger than 3 mm usually require some undermining. Closure with absorbable suture material should be achieved without tension whenever possible. If the tension is excessive, a flap may be needed (see below). The nail plate is then repositioned, and the proximal nail fold is closed.[721]
PART II
Flaps
As previously explained, nail surgery, particularly when involving the matrix, may lead to permanent nail deformities. Soft tissue rearrangement of the nail tissues, in the form of nail flaps, can be used to reconstruct the nail in order to preserve a more normal nail plate. Other nail flaps can also be used to correct congenital malalignment, to cover full-thickness nail unit defects, and for nail fold reconstruction.[21]
These surgeries can be subdivided into total nail unit flaps, nail fold flaps, nail matrix flaps, and other flaps of the nail apparatus. Conversely, flaps are rarely needed in nail bed surgery. The thin epithelium and fibrous dermis of this region tear easily when suturing and fail to mobilize even with significant undermining. Moreover, nail bed defects heal predictably well with second intention healing, which make flaps unnecessary in most instances. This is in dramatic contrast to the matrix, which sutures easily and can be displaced from its deep connective tissue, allowing significant movement with simple undermining. Further, matrix defects often result in a split nail when left to heal by second intention, further highlighting the importance of a correct reconstruction of this area.[21]
Total nail unit flaps
Schernberg flap
The Schernberg flap, first described in 1985, addresses the reconstruction of midline or paramedian longitudinal defects involving all sections of the nail unit. This type of surgery is typically performed in the setting of longitudinal melanonychia or erythronychia,[2223] where the excisional defect will invariably lead to a split nail if reconstruction is not performed.[1221]
The Schernberg flap is cut from the distal end of the defect on the hyponychium and fingertip and carried toward the closest lateral nail fold, extending proximally to a point between the cuticle and the distal interphalangeal crease [Figure 7]. The entire heminail flap is elevated off the periosteum, rotated, advanced into the defect, and finally sutured in place.[21]
- Schernberg flap: (A) paramedian longitudinal lesion involving all sections of the nail unit; (B) flap design, (C) flap is cut and advanced into the defect, and (D) flap sutured in place
In this flap, it is important that the limits of the defect remain tapered proximally (rather than square) and that the matrix epithelium is meticulously realigned. Nonetheless, one should keep in mind that even with meticulous surgical design, a split nail may result.[21]
Unguodermal flap
A similar, albeit larger flap involving the entire nail apparatus is used for correcting congenital malalignment of the great toenail. This condition presents in infancy as a laterally malaligned nail plate; as a result of the malalignment, the nail plate loses attachment with the bed, thickens, and may resemble an oyster shell.[24] Although this condition may spontaneously improve over time, surgical correction remains an option for cases who do not improve, being particularly indicated between two and five years of age.[21]
The unguodermal flap is performed by making a fish-mouth incision from one side of the digit to the other, extending approximately 5 mm beyond the level of the nail bed and 3 to 4 mm proximal to the proximal nail fold. A Burow’s triangle may be executed at the medial proximal flap origin in order to allow tension-free rotation. The entire skin and nail apparatus is undermined above the dorsal distal phalanx, rotated to a normal orientation, and finally sutured into place [Figure 8].[21]
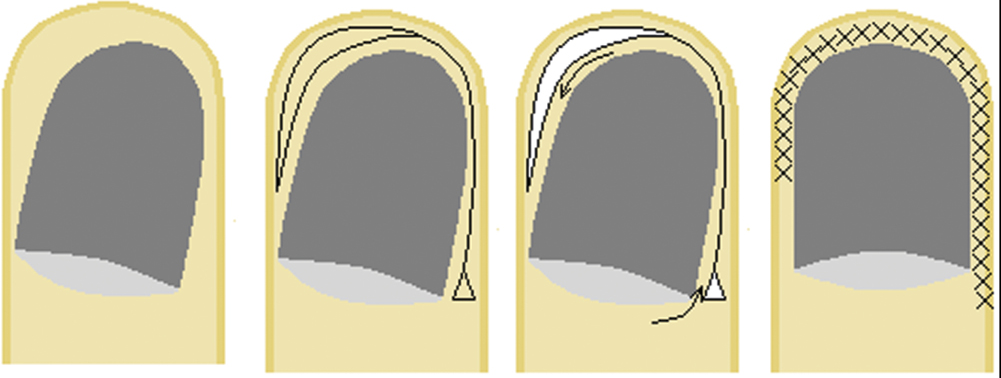
- Unguodermal flap: (A) congenital malalignment of the great toenail, (B) flap design, (C) flap is cut and rotated into a normal orientation (as the nail unit is very firmly attached to the base of the distal phalangeal bone, dissection must be performed in this plan in order to enable rotation of the nail apparatus), and (D) flap sutured in place
Cross finger flap
The cross-finger flap is an alternative to full-thickness skin grafting in the case of total nail unit excision defects. This flap may be performed as either a two- or three-staged interpolation flap, with or without a first step of flap elevation and maturation.[2526] This step maximizes flap viability and minimizes the possibility of ischemic necrosis, which is particularly important in the case of peripheral vascular disease, vasospastic disease, or radiation exposure, where the flap should be elevated and allowed to mature for 7 to 10 days prior to transfer to the adjacent digit.[21]
The flap is cut as a U with the digits opposed to each other and the base of the flap away from the defect, and it is then meticulously undermined. For thumb defects, the proximal phalanx skin of the index finger is used; for other fingers, the middle phalanx skin is utilized.[2125]
Once the flap is elevated (either as a primary surgery in a two-stage procedure or as an intermediate surgery in a three-stage surgery), it is sutured over the defect [Figure 9]. Great care should be taken to avoid tension, crush with forceps, or excessive electrosurgical hemostasis. The secondary defect is typically repaired with a full-thickness skin graft. The flap is left in place for approximately three weeks, after which it is divided. This final-stage surgery is performed relatively simply, with minimal flap thinning and simple suturing of the stump and flap base.[21]
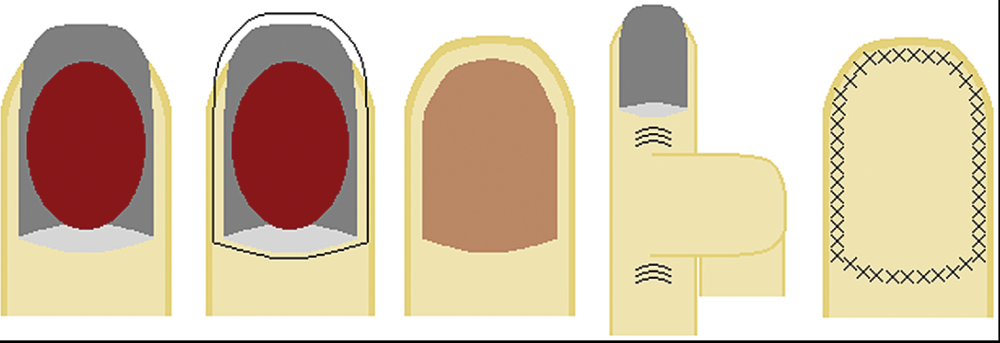
- Cross finger flap: (A) large lesion occupying most of the nail unit, (B and C) the entire nail apparatus is removed, (C) flap is cut as a “U” from an adjacent digit, and (D) flap sutured in place
The cross-finger flap should be reserved for the reconstruction of larger and more complicated defects or for selective situations where skin grafts are contraindicated, and should be performed by experienced hand and nail surgeons.[21]
Nail fold flaps
Proximal nail fold
Proximal nail fold surgery is usually performed for the diagnosis and/or treatment of nail fold or subungual neoplasms, the treatment of chronic paronychia, or posttraumatic reconstruction. It is known that when surgically removed, the proximal nail fold can regenerate to a certain extent, reforming a functional barrier. Therefore, when possible, primary closure and secondary intention healing are simple options, with a high likelihood of an excellent cosmetic and function result on healing.[21] When these techniques are unsuitable, closure with local flaps is required. Skin grafts in the proximal nail fold are usually unsuccessful and should, therefore, be avoided.[27]
Bilateral advancement flap
When larger wedge-type excisions are performed, the defect can be reconstructed with a bilateral advancement flap. Relaxing incisions are made on either side of the defect, the flaps are cut to full thickness, and the primary defect is sutured under no tension [Figure 10]. In most cases, the secondary defects can be closed primarily, utilizing tissue laxity from the digital sides.[21] If this is not possible, the secondary defects are left to heal by secondary intention.
- Bilateral advancement flap: (A) lesion on the proximal nail fold, (B) flap design, (C) flap is cut and advanced into the defect, (D) flap sutured in place (if the secondary defects cannot be closed directly, they are left to heal by secondary intention)
V–Y rotation advancement flap
The V–Y rotation advancement flap represents a good reconstructive flap choice for the total proximal nail fold and eponychium defects. After excision of the lesion, a full-thickness defect is formed at the proximal nail fold region. The flaps should then be designed and marked bilaterally, and skin incisions should be made. The proximally based flaps are carefully elevated, without damaging the vascular network and nail matrix under the flap and without denuding the flap too much. Closure is subsequently done with absorbable sutures [Figure 11].[27]
- V–Y rotation advancement flap: (A) large lesion on the proximal nail fold, (B) flap design, (C) flap is cut, rotated, and advanced into the defect, and (D) flap sutured in place
Lateral nail fold
Bipedicle lateral nail fold flap
A bipedicle lateral nail fold flap can be used to close lateral nail unit defects, which may arise after a wide lateral longitudinal excision or excisional procedure on the lateral nail unit.[28] When these defects cannot be closed primarily, they may be left to heal by second intention or repaired with a bipedicle lateral nail fold flap.[21]
To perform this flap, an incision is made in the mid-lateral line and the flap is undermined, retaining its proximal and distal attachments. The resulting primary defect is closed easily under no tension, and the secondary defect is either sutured (if possible) or left to heal by second intention [Figure 12].[21]
- Bipedicle lateral nail fold flap: (A) lesion on the lateral nail fold, (B) flap design, (C) flap is cut and advanced into the defect, retaining its proximal and distal attachments, and (D) flap sutured in place
Nail matrix flaps
Matrix surgery may be incisional (cut and reflected to access dermal neoplasms, such as glomus tumors or subungual myxoid cysts) or excisional (when attempting to extirpate the entire lesion, such as longitudinal melanonychia or erythronychia).[2129]
Incisional surgery is repaired with simple careful resuturing of the matrix epithelium in its anatomic position, an easy procedure as there is no tension on the epithelium and it is simple to realign the margins. Excisional surgery, particularly when full thickness, leaves a matrix defect that risks nail splitting if not surgically repaired, a fact that is particularly true for proximal and mid-matrix defects.[21]
Narrow defects in these regions (less than 3 mm wide) can usually be repaired primarily, as long as an adequate undermining is accomplished. Defects wider than 3 mm, however, are usually difficult to close primarily. There are several sliding matrix flaps that address such defects, and due to the robust circulation of the nail apparatus, flap necrosis is unusual.[2130]
These matrix flaps are best utilized for fusiform defects, which is important as most nail disorders have a longitudinal orientation. They are usually reserved for defects in the midline or paramedian nail rather than the lateral nail unit, where lateral longitudinal excisional surgery is preferable.[2128]
Matrix bipedicle flap
The most useful of these flaps is the matrix bipedicle flap. An incision is performed just lateral to the matrix in the lateral nail sulcus, and then undermining is performed from the defect to this incision, until the blade tip is visible. This creates a bipedicle flap, with perfusion to the flap from proximal and distal circulation. The surgery can be unilateral or bilateral, in cases where more tissue mobility is needed [Figure 13].[21]
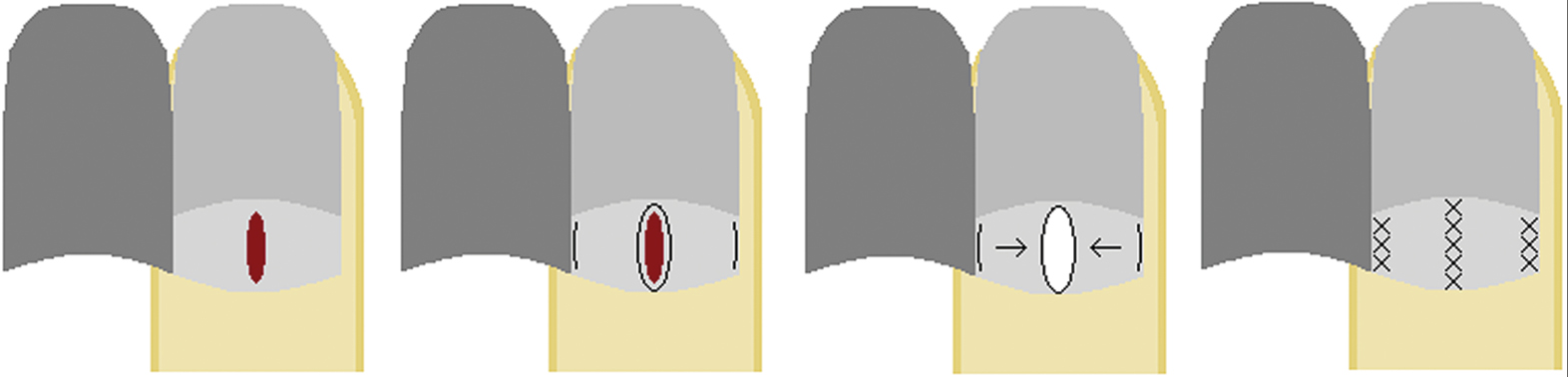
- Matrix bipedicle flap: (A) midline lesion arising from the nail matrix, (B) flap design, (C) flap is cut and advanced into the defect, retaining its proximal and distal attachments, and (D) flap sutured in place
A possible complication of this flap occurs when the incision in the lateral sulcus transects the lateral matrix horn, leaving a spicule lateral to the flap. To avoid this, the surgeon must take great care to reflect the lateral nail fold away from the flap in order to correctly visualize and perform the incision adjacent to the lateral matrix epithelium.[21]
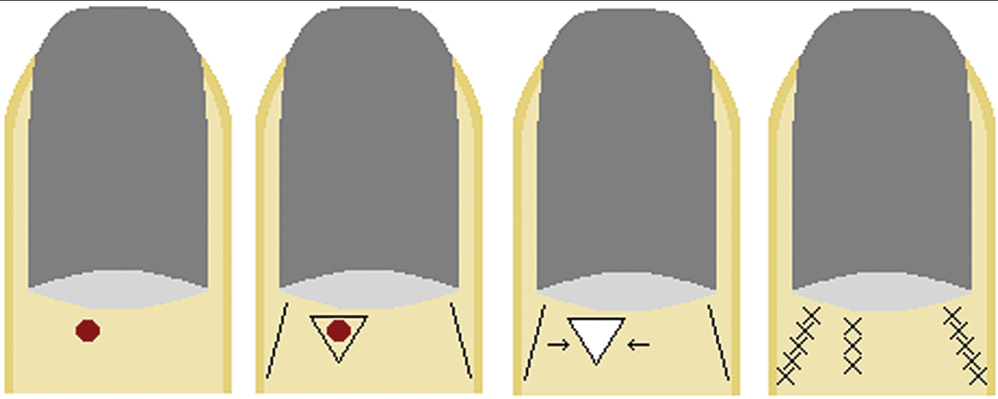
Unilateral or bilateral sliding (advancement and rotation) flap
The unilateral or bilateral sliding (advancement and rotation) flap can be performed to reconstruct mid- and distal matrix defects, which are often encountered after longitudinal erythronychia or melanonychia excision. In this flap, an incision is performed along the junction between the matrix and the bed to the lateral sulcus on one or both sides of the defect, depending on the degree of tissue movement required. The flap is undermined, and the matrix epithelium is sutured together without tension [Figure 14].[21]
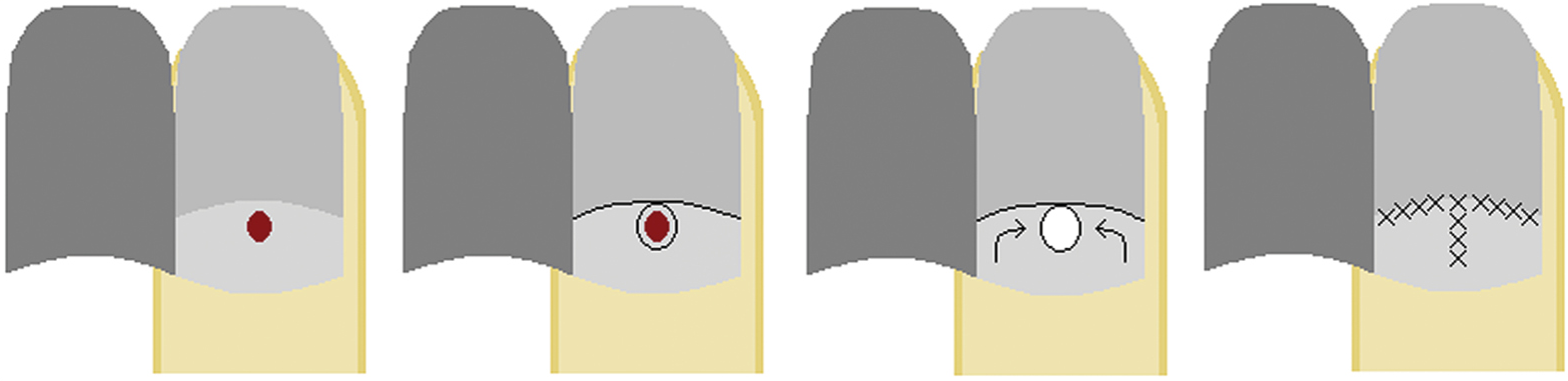
- Bilateral sliding (advancement and rotation) flap: (A) lesion arising from the mid to distal nail matrix, (B) flap design, (C) flap is cut, rotated, and advanced into the defect, and (D) flap sutured in place
Bilateral A-to-T advancement flap
For true proximal matrix defects, such as localized pigmented lesions, warts, glomus tumors, or subungual myxoid cysts, a bilateral A-to-T advancement flap can be utilized. This is the least commonly used of the three flaps limited to the matrix, and it should be reserved to defects that will invariably heal with a split nail unless adequately repaired.[21]
The flap is cut along the proximal matrix margins, where it transitions to the eponychium.[30] Care must be taken to avoid injury to the underlying extensor tendon. The flap is then undermined in the subdermal plane and sutured in standard fashion with interrupted absorbable sutures [Figure 15]. Given that the proximal matrix may extend onto the proximal eponychium, this flap may transect the matrix and lead to lamellar splitting of the nail plate, evidenced by onychoschizia.[21]
- Bilateral A-to-T advancement flap: (A) lesion arising from the proximal nail matrix, (B) flap design, (C) flap is cut, rotated, and advanced into the defect, and (D) flap sutured in place
Post surgery care
Postoperative care is essential for successful nail surgery. After finishing the procedure, a dressing of petrolatum impregnated gauze should be applied directly on the surgical site, followed by multiple 2 × 2 cm gauzes, folded in half and wrapped over the nail unit transversely and longitudinally. These should then be secured with adhesive tape, avoiding circumferential taping. The original dressing should be left in place for 24–48 h, after which it can be changed everyday or every other day.[6]
As with every surgery, it is important to assess infection risk and prescribe antibiotics accordingly. Pain medication should always be prescribed, as postoperative pain is expected to be significant.[21] The patient should be advised to keep the affected limb elevated in order to minimize pain and swelling. Activities involving the operated limb, especially in the case of toenails, should be avoided for at least two weeks.[13]
Approach to the most common clinical scenarios
Paronychia
-
-
-
-
Chronic paronychia: Surgical management is only indicated in recalcitrant cases of chronic paronychia.[32] The most commonly used technique is simple eponychial marsupialization, in which, under local anesthesia, a bevelled excision of the distal half of the proximal nail fold is performed. The wound created heals within six to eight weeks, and a new cuticle forms, sealing the nail pocket.[3] En bloc excision of the proximal nail fold is another treatment option, which is usually performed together with nail plate avulsion.[32] The Swiss roll technique can also be used in cases of chronic and severe acute paronychia with infection involving the nail folds, as it exposes the nail bed, allowing the drainage of any residual infection.[32]
-
-
Subungual felon: A subungueal felon represents a painful area with underlying pus. In these cases, the nail plate has to be fenestrated over the affected area or partially avulsed. After the procedure, the finger should be soaked twice daily in antiseptic solutions and oral antibiotics may be given.[3]
Trauma
-
-
Hematomas: A hole should be made in the nail plate over the fresh hematoma, in order to allow the blood to escape. This reduces the pressure and, consequently, the pain.[3]
-
-
Subungual foreign bodies: Careful separation of the overlying nail will allow the foreign body to be seen, and it can then be removed either with a fine needle or with a scalpel.[3]
Onychogryphosis
Nail avulsion is usually the first approach in cases of onycogryphosis [Figure 16]. Although it can be difficult from the distal aspect, this procedure is very easy if a proximal approach is used.[3]

- Onychogryphosis of the first toenail
Ingrowing nails
Infancy
There are three kinds of ingrowing toenails presenting before the age of two years:
Distal toenail embedding with normally directed nail: Conservative management should be employed, by gently massaging the distal nail wall in a distal-plantar direction.
Congenital hypertrophic lip of the hallux: This may disappear spontaneously after several months, but in very pronounced cases, resection of the hypertrophic lip with second-intention healing is indicated.
Congenital dystrophy of the big toenail (malaligned hallux nail): A crescentic wedge excision, larger on the medial than on the lateral aspect, is carried out back proximal to the nail bed and nail matrix. The entire nail organ is dissected from the underlying bone, rotated into its correct position, and finally sutured in place.[3]
Juvenile ingrown toenail
Treatment for the early stage is conservative. Surgical treatment is aimed at definitive cure and is preferred in moderate and severe cases.[33]
As previously mentioned, phenolization is a simple and highly effective method with low recurrence rates, thus being preferred in most cases.[33] Selective lateral matrix excision is a more demanding but also effective alternative, as well as CO2 laser ablation of the lateral matrix tissue.
Other surgical techniques traditionally performed in the setting of ingrown nails include:
-
-
partial nail avulsion, either combined with surgical partial matricectomy or with physical (electrofulguration) matricectomy (Ross procedure);[33]
-
-
wedge excision of a nail fold together with the matrix and nail bed (Winograd procedure);[34]
-
-
total nail avulsion combined with total (chemical or surgical) matricectomy (Zadik procedure);[35]
-
-
-
-
rotational flap technique of the nail fold.[38]
Avulsion of the nail plate is not a suitable long-term treatment option for ingrown nails, as it is almost invariably followed by recurrence. Moreover, nail avulsion may result in distal nail embedding of the hallux nail, as the pulp of the hallux is pushed dorsally during gait, creating a distal nail fold. When this distal wall does not regress with taping and massaging back in a distal-plantar direction, a fish-mouth incision can be carried out parallel to the distal groove on the tip of the toe, such that its closure pulls the distal nail wall down [Figure 17].

- Performance of a fish-mouth incision parallel to the distal groove on the tip of the toe, such that its closure pulls the distal nail wall down
Retronychia
The surgical technique of choice consists of cautious avulsion of superimposed nail plates and excision of granulation tissue [Figure 18].[39] It is important to note that the treatment of retronychia must also include the management of associated predisposing factors, including adequate footwear and correction of static disorders of the foot.[40]
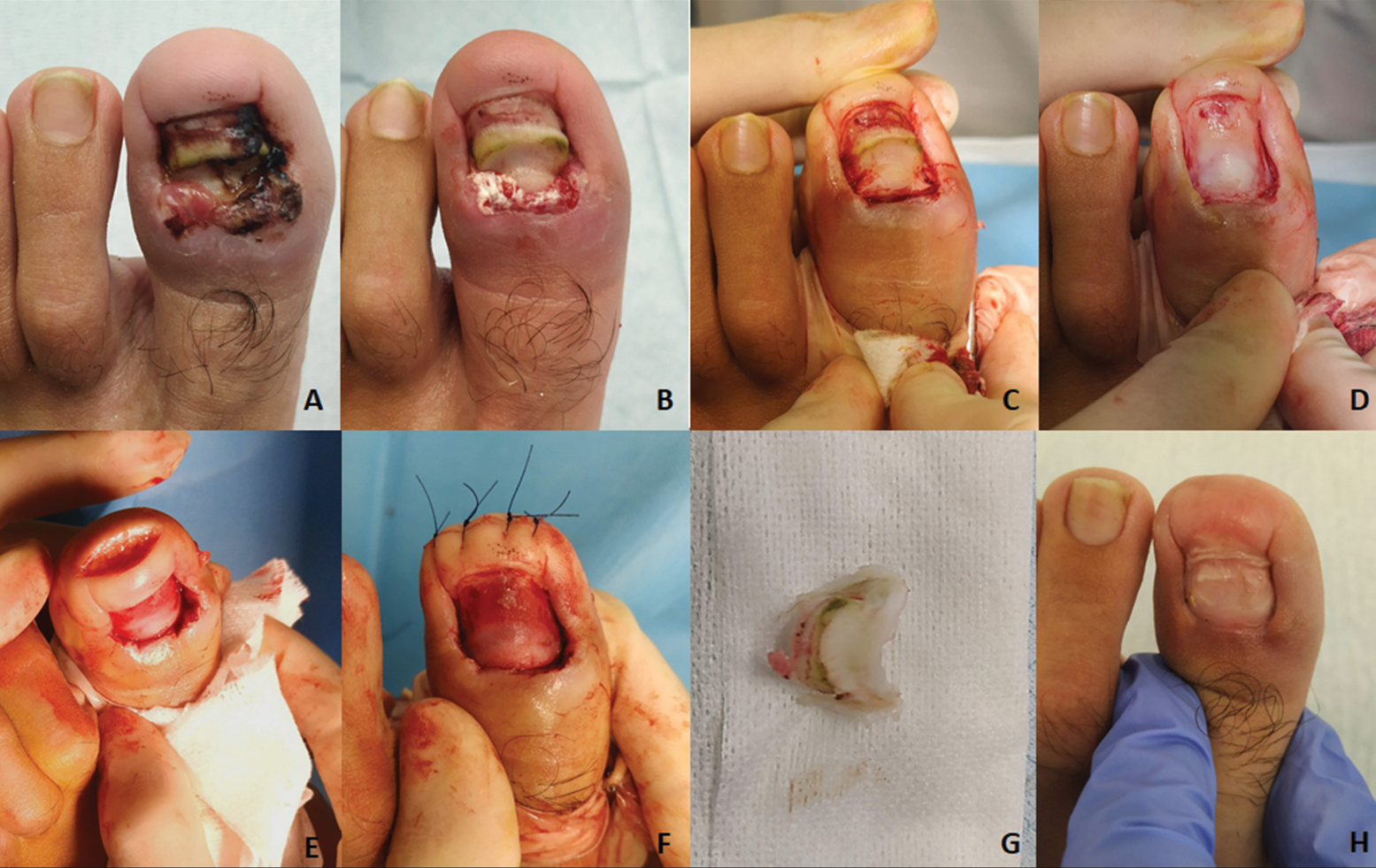
- Retronychia: (A) initial appearance, (B) appearance of the nail apparatus after removal of the first nail plate, (C) appearance of the nail apparatus after removal of another nail plate and curettage of granulation tissue, (D) nail plate avulsion complete, (E) plasty of the digital pulp using Howard Dubois technique, (F) result by the end of the surgery, (G) image of some of the nail plates removed, and (H) follow-up six months later, with satisfying cosmetic and functional results
Pincer nails
Pincer nails are characterized by an excessive transverse curvature of the nail plate that increases distally.[41] In mild cases, conservative management may be performed to uncurve the nail distally. Definitive treatment involves cauterization of both lateral matrix horns, leading to narrower, less overcurved nails.[3] This technique may be combined with softening of the nail plate with thioglycolic acid solution and shaping with two anticonvex sutures.[41] The nail plate and bed reconstruction technique is another proposed option to correct this deformity.[42]
Verrucae
Cryosurgery is the most common method used for the treatment of common warts.[4] An alternative approach involves keratolysis with monochloroacetic acid plus 50% salicylic acid under occlusion, hot baths, and repeated curettage of the necrotized keratotic masses. Curettage or CO2 laser under local anesthesia or the use of pulsed dye laser are alternatives. Bleomycin, an antibiotic that causes DNA strand scission, is particularly useful for recalcitrant ungual warts. It can be directly injected into the warts or applied over them followed by puncture with a lancet.[43] Electrosurgery should not be used in the nail region, as it may lead to keloids.[3]
Ungual fibrokeratomas
The removal of ungual fibrokeratomas involves cutting around them down to the bone and dissecting them by using curved pointed scissors. Healing is fast, and sequelae are rare.[3]
Digital myxoid pseudocyst
Digital myxoid pseudocyst is one of the most common nail tumors, and it usually presents as a proximal nail fold tumefaction associated with an irregular longitudinal groove of the nail plate. The treatment approach with lowest recurrence rates involves an intraarticular injection of sterile methylene blue to visualize the potential stalk to the joint, which has to be ligated in addition to dissection of the lesion. Other alternatives include simple repeated punctures, injections of steroids or sclerosants, cryosurgery, laser evaporation, infrared coagulation, or simple excision with sutures [Figure 19].[3]
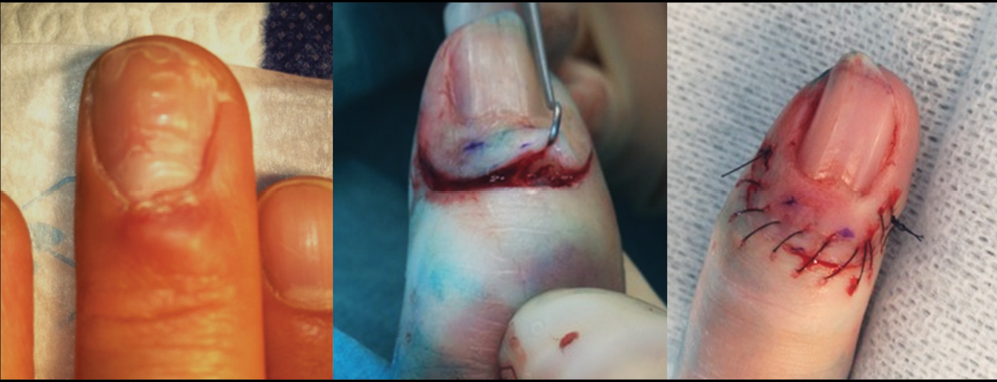
- Digital myxoid pseudocyst. Simple excision with ligation of the pedicle in the distal interphalangeal joint
Subungual exostoses
The overlying skin is incised, and the exostosis is dissected and clipped off at its base, with a nail clipper or bone rongeur [Figure 20]. If the lesion is located more proximally under the nail plate, this may be partially avulsed to permit access to it. Primary suturing is usually possible.[3]
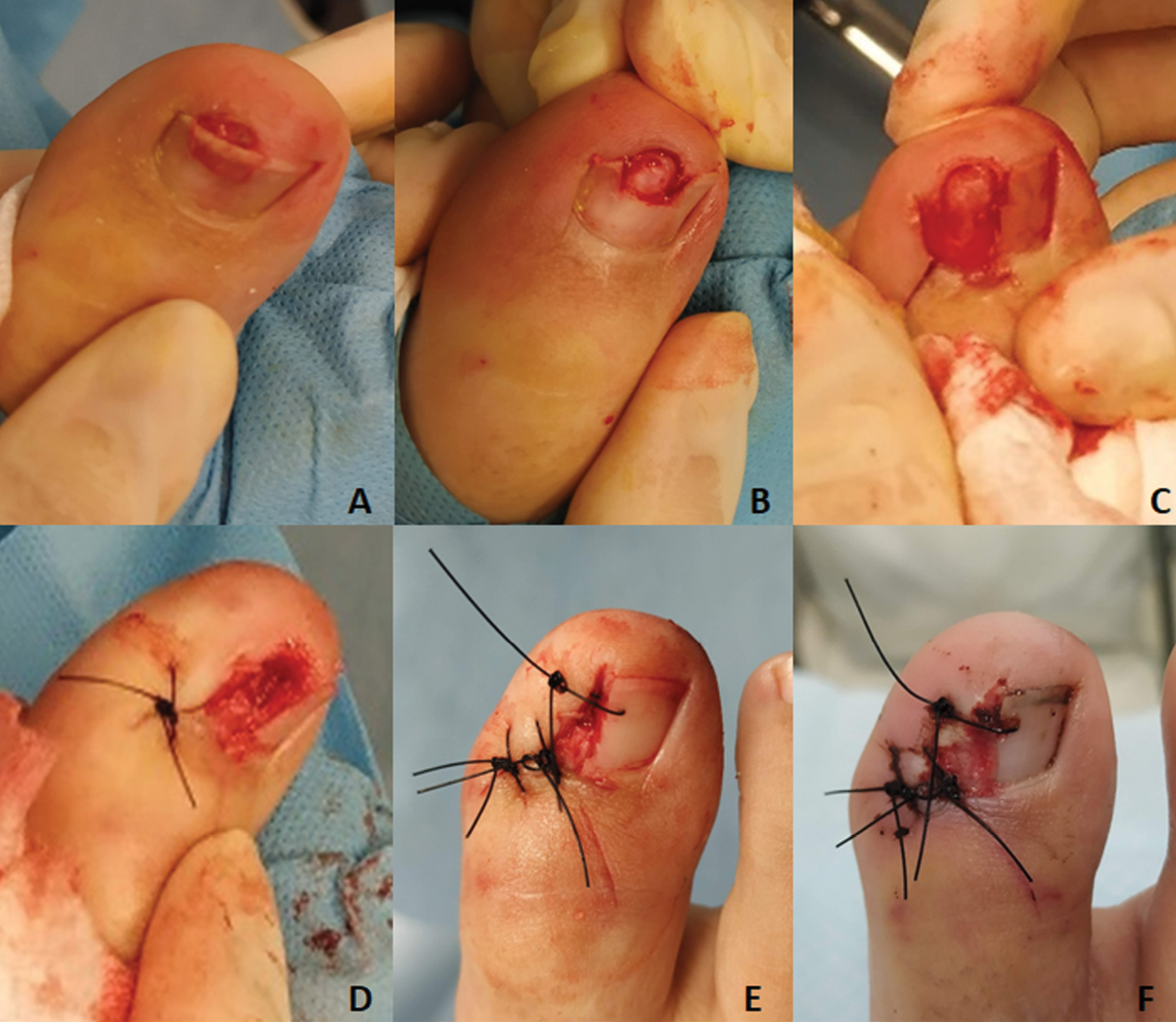
- Subungual exostoses. (A) A lesion is observed under the distal nail plate; B: bone consistency is perceived after removing part of the nail plate. (C and D) Overlying skin is incised and the exostosis is dissected and clipped off at its base. (E) Result by the end of the surgery. (F) Result two weeks after surgery
Subungual glomus tumor
Subungual glomus tumors are round to oval violaceous spots causing a longitudinal erythematous band. When located in the lateral third of the nail bed or matrix, they are extirpated via the lateral aspect of the phalanx; an L-shaped incision is performed, and the nail bed is dissected from the bone. When located in a central location, they are removed after cutting a hole in the nail plate or partially separating it from the matrix and nail bed and incising the latter longitudinally or the former transversally, respectively. The lesion is dissected, the defect sutured, and the nail plate put back to speed up healing.[3]
Bowen’s disease and squamous cell carcinoma
Bowen’s disease and squamous cell carcinoma of the nail region constitute the second most frequent nail malignancy, after ungual melanoma. Lesions should be excised with safety margins. If the defect is no wider than half of the nail, a bridge flap is formed from the lateral aspect of the distal phalanx and sutured to the nail, thus creating a new lateral nail wall. This will result in a narrow nail, but a functionally intact distal phalanx. Larger defects are repaired with full-thickness skin graft or cross-finger flaps.[3]
Ungual melanoma
Melanoma of the nail apparatus is probably the most frequent malignant nail neoplasm, and it most commonly presents as a longitudinal melanonychia. The approach to longitudinal melanonychia depends on its size and appearance. Streaks with a width of less than 3 mm and homogeneous pigmentation may be followed carefully, whereas streaks measuring more than 3 mm in width or with heterogeneous pigmentation should be biopsied. In these cases, the surgical technique varies according to their location in the nail: Laterally positioned streaks are treated by a lateral longitudinal nail biopsy; median ones are treated by a punch or fusiform biopsy or horizontal excision. When the diagnosis is certain, the melanoma is completely removed by excision of the entire nail organ and the defect is repaired with a cross-finger flap or skin graft.[3]
CONCLUSION
In order to accurately perform nail surgery, it is essential that the surgeon has complete knowledge regarding the anatomy and physiology of this particular structure. Once this knowledge is acquired, nail surgery is usually not complex, and the quality of life of patients can easily be improved in many instances. In this article, a review of the main surgical techniques for approaching each anatomical area of the nail apparatus was made. Subsequently, the techniques most frequently used in the treatment of the most common pathologies were addressed. Being an area with an important surgical component, it is essential that dermatologists are familiar with these techniques and feel free to put them into practice whenever necessary.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Digital anesthesia with epinephrine: An old myth revisited. J Am Acad Dermatol. 2004;51:755-9.
- [Google Scholar]
- A compendium of intralesional therapies in nail disorders. Indian Dermatol Online J. 2018;9:373-82.
- [Google Scholar]
- Punch biopsies of nails: A simple, valuable procedure. J Dermatol Surg Oncol. 1978;4:528-30.
- [Google Scholar]
- Nail avulsion: Indications and methods (surgical nail avulsion) Indian J Dermatol Venereol Leprol. 2012;78:299-308.
- [Google Scholar]
- Total nail ablation for onychodystrophy with optimized gauze-phenol application. J Eur Acad Dermatol Venereol. 2010;24:936-42.
- [Google Scholar]
- Avulsion and partial matricectomy with the carbon dioxide laser for pincer nail deformity. Dermatol Surg. 2004;30:456-8.
- [Google Scholar]
- Phenol alcohol technique for permanent matricectomy. Arch Dermatol. 1984;120:348-50.
- [Google Scholar]
- Follow-up study of patients treated for ingrown nails with the nail matrix phenolization method. Plast Reconstr Surg. 1995;95:719-24.
- [Google Scholar]
- Diagnosis and management of nail pigmentations. J Am Acad Dermatol. 2007;56:835-47.
- [Google Scholar]
- Longitudinal erythronychia: Suggestions for evaluation and management. J Am Acad Dermatol. 2011;64:167.e1-11.
- [Google Scholar]
- Reversed cross finger subcutaneous flap: A rapid way to cover finger defects. Indian J Plast Surg. 2008;41:55-7.
- [Google Scholar]
- Proximal nail fold reconstruction with bilateral V-Y rotation advancement flaps. Dermatol Surg. 2016;42:121-2.
- [Google Scholar]
- Matrix biopsy of longitudinal melanonychia and longitudinal erythronychia: A step-by-step approach. Cosmet Dermatol. 2009;22:130-6.
- [Google Scholar]
- Midline/paramedian longitudinal matrix excision with flap reconstruction: Alternative surgical techniques for evaluation of longitudinal melanonychia. J Am Acad Dermatol. 2010;62:627-36.
- [Google Scholar]
- Best evidence topic report. Incision and drainage preferable to oral antibiotics in acute paronychial nail infection? Emerg Med J. 2005;22:813-4.
- [Google Scholar]
- Operative treatment of the ingrown toenail with a less-invasive technique: Flashback to the original winograd technique. Foot Ankle Spec. 2018;11:138-41.
- [Google Scholar]
- Operative treatment of ingrown toenail by nail fold resection without matricectomy. J Am Podiatr Med Assoc. 2015;105:295-301.
- [Google Scholar]
- Nonrandomized assessment of ingrown toenails treated with excision of skinfold rather than toenail (NAILTEST): an observational study of the vandenbos procedure. J Pediatr Surg. 2017;52:832-6.
- [Google Scholar]
- Lateral fold rotational flap technique for treatment of ingrown nail. Plast Reconstr Surg. 2007;120:2131-3.
- [Google Scholar]
- Retronychia of the toenails: A review with emphasis on pathogenesis, new diagnostic and management trends. Arch Dermatol Res. 2019;311:505-12.
- [Google Scholar]
- Triple combination therapy for pincer nail deformity: Surgical matricectomy, thioglycolic acid, and anticonvex sutures. Dermatol Surg. 2017;43:1474-82.
- [Google Scholar]
- Nail plate and bed reconstruction for pincer nail deformity. Clin Orthop Surg. 2018;10:385-8.
- [Google Scholar]






