Translate this page into:
Nail unit incision lines: A tool to minimize nail unit scarring
*Corresponding author: Chander Grover, Department of Dermatology and STD, University College of Medical Sciences and GTB Hospital, Dilshad Garden, Delhi 110095, India. chandergroverkubba@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Grover C, Bansal S, Gupta S. Nail unit incision lines: A tool to minimize nail unit scarring. J Cutan Aesthet Surg. 2024;17:343-7. doi: 10.4103/JCAS.JCAS_67_23
Abstract
Langer’s lines, lines of cleavage, and biodynamic excisional skin tension (BEST) lines have been defined for cutaneous surgery to ensure excisional wound closure with the least tension on any part of the body and minimize scarring. This article describes nail unit incision lines (NUIL) with a similar perspective. NUIL are followed by nail surgeons to help regrowth of a normal nail; however, they are not widely understood or respected during nail surgery. Within the anatomically small nail unit, the orientation of these lines varies depending on the area being operated upon. Nail bed incisions should be oriented longitudinally, while nail matrix incisions should be oriented horizontally. Being the germinative portion, the nail matrix should be dealt with more cautiously, avoiding the lunular margin. Lateral nail fold incisions should be longitudinal, while proximal nail fold incisions should be radial. Distal nail fold (hyponychial) incisions should preferably be oriented parallel to the distal nail ridge. Knowledge and compliance with NUIL can help minimize scarring outcomes in nail surgery.
Keywords
Biodynamic excisional skin tension lines
Cleavage lines
Nail surgery
Relaxed skin tension lines
Learning Points
Surgical wound closure should avoid tension to avoid disfiguring outcomes in cutaneous surgery. Nail unit incision lines help ensure this during nail surgery.
Nail bed incision lines run longitudinally, parallel to the nail bed ridges.
Nail matrix incision lines are horizontally oriented and avoid the lunula margin.
Nail fold incision lines are longitudinal in lateral nail folds and radial in proximal nail fold. Distal nail fold (hyponychial) incisions are oriented parallel to the free edge of the nail plate.
Knowledge of and compliance with nail unit incision lines (NUIL) can help minimize the chances of post-operative nail dystrophy.
Onycho-surgery (surgery of the nail unit) is a rapidly evolving field of dermatosurgery. It comprises various incisional and excisional surgeries, all confined to the anatomically small but complex nail unit. Depending on the type and extent of excisions, nail surgeries entail surgical wound closure on many occasions. As with other cutaneous surgeries, primary closure of the surgical wound, without tension, is necessary to ensure a good surgical outcome.
It is a well-established fact that cutaneous surgical excision wounds should be closed without tension to avoid scar stretching and disfiguring outcomes. This means that surgical incisions should be planned well; however, differing views and descriptions have existed regarding this planning.1 Various incision lines have been described for use in cutaneous surgery. Langer’s lines (best described as cleavage lines) are lines along which the skin splits when traumatized.2 Kraissl lines are based on the orientation of wrinkles, using the premise that they are determined by muscle contraction. These lines were thought to be ideal for surgical excisions.3 Borges proposed “relaxed skin tension lines” for surgical excisions, considering both the ridges and furrows in skin.4 Biodynamic excisional skin tension (BEST) lines are based on the measurement of skin tension measured by a tensiometer during various excisional cutaneous surgeries.5 These lines have been methodically mapped along the least tension.
Many books and authoritative texts depict cleavage lines and Langer’s lines (though slightly differently) to be used as a ready reference before cutaneous surgical excisions in different body parts. Many of us also have them pasted in our operation theaters for quick guidance. BEST lines for surgical excisions across the human body have also been mapped and are available for easy reference and preoperative consultation. However, similar descriptions or diagrams are not available for nail surgery or onycho-surgery.
The nail is better described as the “nail unit” consisting of the nail plate (product portion) attached to the nail bed; nail matrix (germinative portion); nail folds (proximal, distal, and lateral); apart from the underlying phalanx. Its anatomical complexity is based on the different types of epithelia comprising it as well as undergoing different modes of keratinization. The transition from the nail matrix epithelium to the nail bed epithelium is abrupt at the lunula. Distal to the lunula margin lies the nail bed epithelium with its characteristic longitudinal ridges, which are instrumental in ensuring adherence of the nail bed to the nail plate. Proximal to it is the shiny white, tenacious, but smooth nail matrix epithelium. In contrast, the nail fold epithelia tend to have dermatoglyphic markings like normal skin, except for the proximal nail fold epithelium, which rather folds on itself.
Owing to this complex anatomy, packed in a small space, operative incisions should be oriented as per the anatomical area being operated upon.6 We described these incision lines as NUIL, schematically depicted in Figure 1.
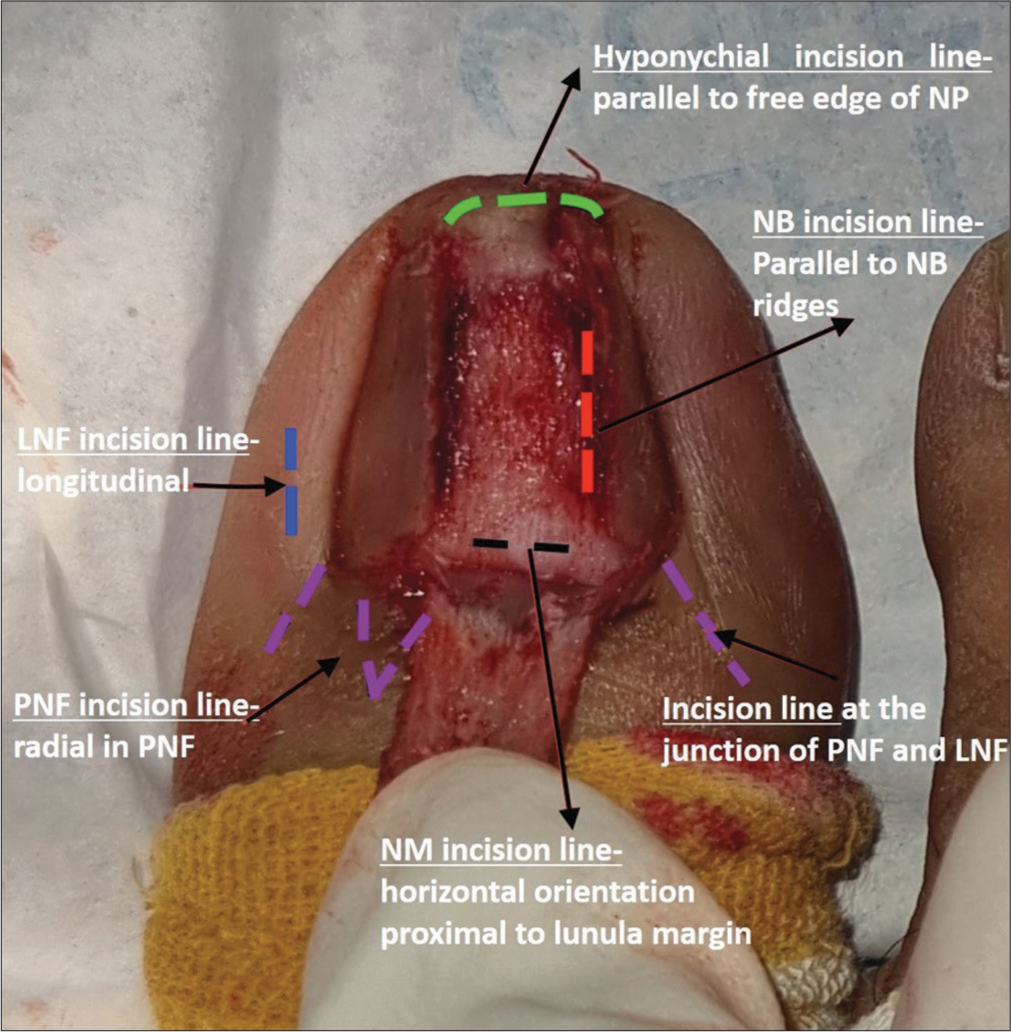
- Nail unit incision lines (NUIL) during nail surgery (represented as broken lines), to be followed in various anatomic areas of the nail unit. Nail bed (NB) incision line (red), nail matrix (NM) incision line (black), proximal nail fold incision (PNF) lines (purple), lateral nail fold (LNF) incision line (blue), and hyponychial incision line (green) are depicted. NP: Nail plate.
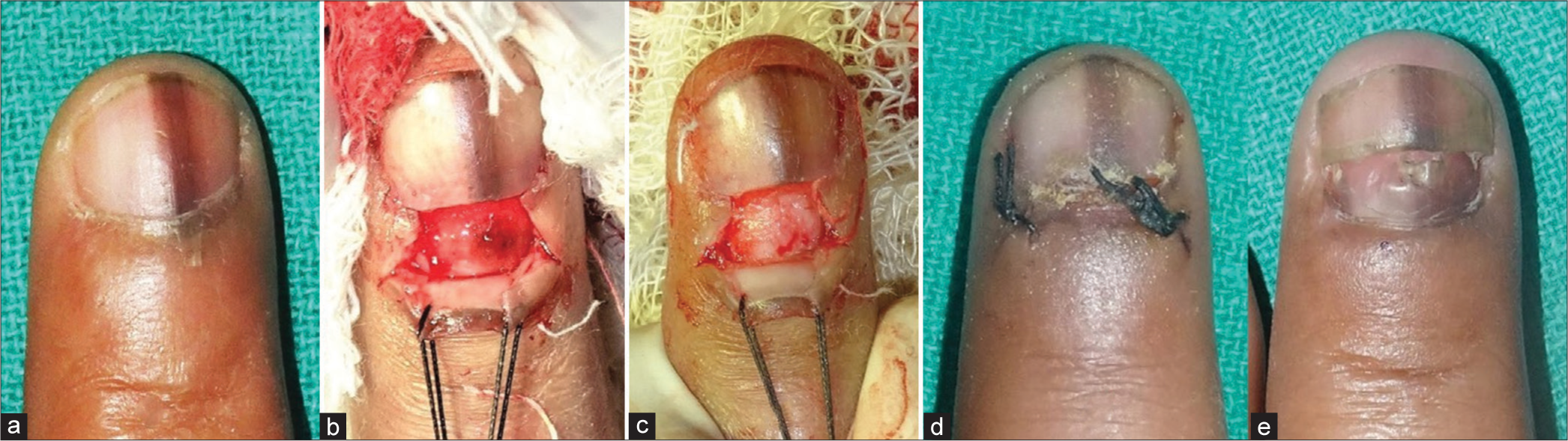
Nail bed incisions are often indicated for exploring and excising nail bed tumors, including glomus tumor [Figure 2a-e]. Such incisions should always be oriented longitudinally, parallel to the nail bed ridges, which themselves correspond to the undersurface of the nail plate, and help ensure its proper adherence. Nail bed excisions done longitudinally help ensure easier primary closure of the defect with the least tension. The regrowing nail plate is also able to attach properly, thus preventing any persistent foci of onycholysis. While every attempt should be made to close nail bed defects, excisions up to 3 mm are left unsutured at times if closure is difficult, e.g., a punch biopsy [Figure 3a-c]. Suturing larger defects may require lateral release incisions at times.
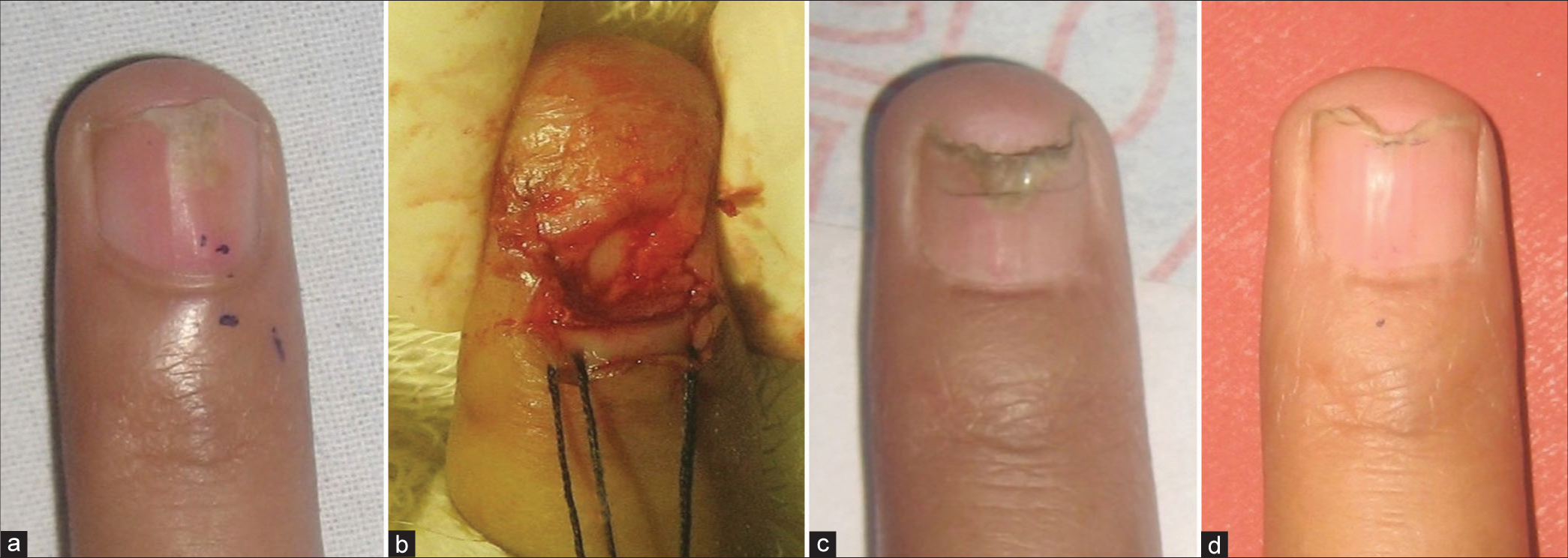
Nail matrix, being the germinative portion of the nail unit, should be dealt with more cautiously. Excisions in this location are primarily for nail matrix tumors, including glomus tumor. Incisions in the nail matrix should be oriented horizontally [Figure 4] and also closed similarly. As far as possible, the matrix incisions should be confined to the distal matrix rather than the proximal matrix. Incisional lines should not cross the lunula margin as well. This helps prevent any postoperative distortion of the matrix, preventing a dystrophic nail plate in turn. Another common cause for excisional surgery in a matrix is the removal of the origin of longitudinal melanonychia. For this, tangential excision has been described, which does not require closure as well [Figure 5a-e].
Lateral nailfold incisions should be oriented longitudinally [Figure 6], i.e., parallel to the dermatoglyphic pattern in this location. Such incisions can often be closed primarily easily. Indications include a biopsy of a primary dermatosis or a dermal growth in this location.
Proximal nail fold (PNF) incisions are oriented radially [Figure 7]. Any excision in this location is preferably a crescentic excision, with its long axis kept perpendicular to the free edge of the PNF. This enables primary closure with the least distortion of the complex curved anatomy of the PNF. A common reason for excision in this location is the myxoid cyst. Radial incisions are also required while reflecting the PNF for better visualization of the nail matrix [Figure 8].
Distal nail fold (hyponychial) incisions are oriented horizontally, parallel to the distal nail ridge or to the free edge of the nail plate. These incisions are used for the management of distal ingrown nail or hypertrophic nail folds.
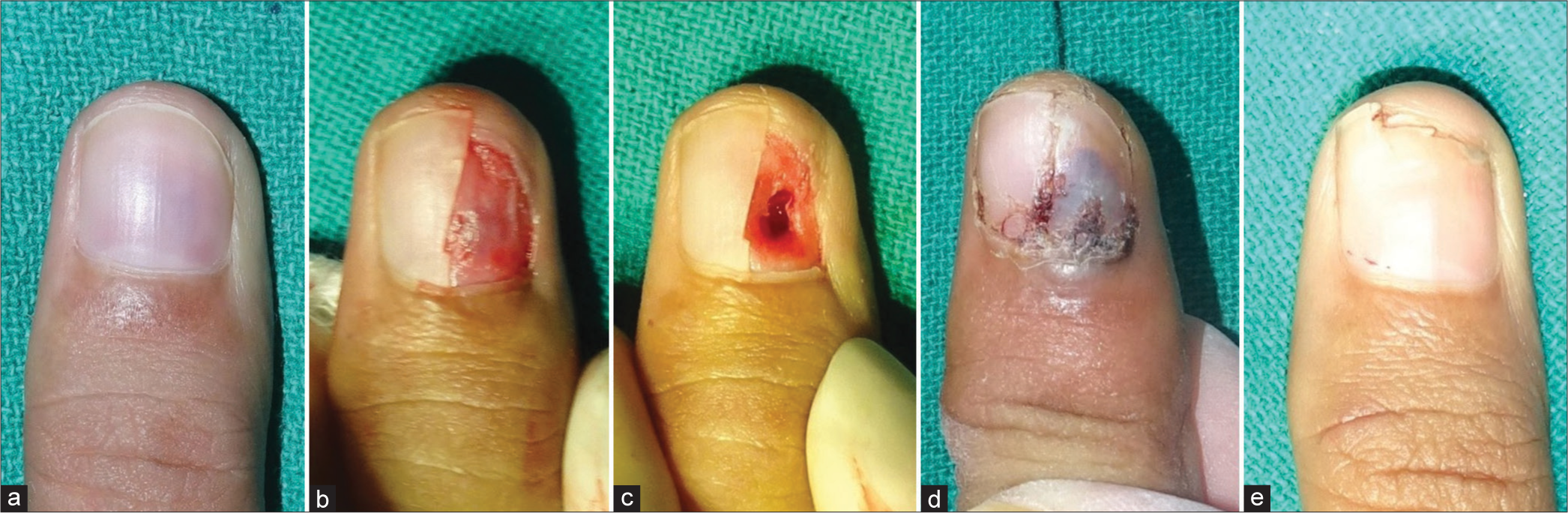
- (a-e) Longitudinal nail bed incision to remove a glomus tumor in this location. (a) Nail bed glomus tumor is seen as a bluish discoloration through the nail plate. (b) Lateral partial nail avulsion to expose the nail bed tumor. (c) Longitudinal excision of the tumor with the resultant nail bed defect. (d) Primary closure with nail plate repositioning, as seen at one week. (e) Regrowth of normal nail plate 5 months postoperatively.
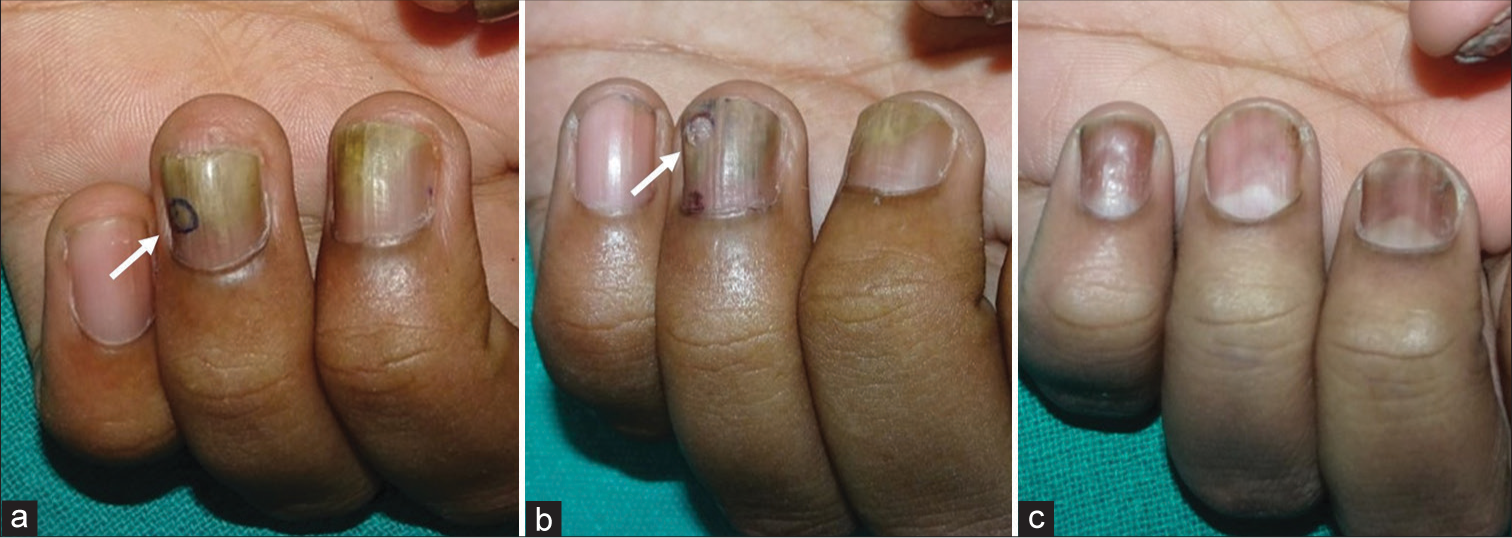
- (a-c) Nail bed punch biopsy. (a) Patient with suspected nail psoriasis. The chosen biopsy site has been marked (white arrow). (b) Growing out nail plate at 2 months after a 3 mm punch biopsy (which was not sutured) (white arrow). (c) Normal appearance of the nail at 4 months (patient is on treatment for nail psoriasis) with growing out of the biopsy created defects.
- (a-d) Horizontal nail matrix incision to remove a nail matrix glomus tumor. (a) Nail matrix glomus tumor with a distal onycholysis. (b) Nail plate avulsion with retraction of the proximal nail fold (held back by stay sutures) to expose the nail matrix tumor, which has been excised. (c) Regrowth of the normal nail plate at 3 months. The laterally placed nail fold incisions have also healed without substantial scarring. (d) Normal appearing nail, without onycholysis or median split, at 5 months.
- Tangential biopsy of the nail matrix for longitudinal melanonychia. (a) Longitudinal melanonychia involving the index finger. (b) Proximal partial avulsion with retraction of the proximal nail fold to expose the origin of the pigmented band. (c) Tangential shave excision was done to remove the nail matrix lesion. (d) Replacement and suturing of the proximal nail fold. (e) Regrowth of nail at 2 months. Note: The laterally placed nail fold incisions have also healed without scarring.

- Lateral nail fold tumor (black circle) requires a longitudinal incision for complete surgical removal.

- Radial incision in the proximal nail fold to expose the underlying tumor.

- Separation of lateral nail fold and proximal nail fold done with the help of two radial incisions given at their junction. This enables complete retraction of the proximal nail fold, which is often required for proximal nail avulsion and/or exploration of the proximal nail matrix.
It has been our experience over the years that operating along NUIL enables a tension-less primary closure of the surgical wound. This is one of the factors for ensuring the regrowth of a normal nail post-operatively, with least distortion of this delicate architectural unit. Proper direction of incisions helps ensure proper direction of healing, which determines whether scarring of the nail bed/matrix occurs. While operating on nail unit malignancy or traumatic lacerations, it may not be possible to plan incisions or suturing based on these suggestions. However, these incision lines should be followed as far as possible while dealing with benign pathology. The use of appropriate sutures and repositioning the nail plate after surgery as far as possible are the other important factors determining long-term cosmetic outcomes. An in-depth understanding of surgical nail unit anatomy and compliance with NUIL can help minimize scarring outcomes in nail surgery.
Authors’ contributions
All the authors contributed to the research study. Chander Grover: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Shikha Bansal: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review. Somesh Gupta: Concepts, design, definition of intellectual content, literature search, manuscript preparation, manuscript editing, and manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- On the anatomy and physiology of the skin. Br J Plast Surg. 1978;31:393185273-8106199278.
- [CrossRef] [Google Scholar]
- The selection of appropriate lines for elective surgical incisions. Plast Reconstr Surg. 1951;8:1-28.
- [CrossRef] [PubMed] [Google Scholar]
- Relaxed skin tension lines (RSTL) versus other skin lines. Plast Reconstr Surg. 1984;73:144-50.
- [CrossRef] [PubMed] [Google Scholar]
- Biodynamic excisional skin tension lines for surgical excisions: Untangling the science. Ann R Coll Surg Engl. 2018;100:330-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nail biopsy: A user's manual. Indian Dermatol Online J. 2018;9:3-15.
- [CrossRef] [PubMed] [Google Scholar]






