Translate this page into:
Nevus of Ota: Combination Treatment with Q-Switched Neodymium-Doped Yttrium Aluminum Garnet Laser and Fractional CO2 Laser
Address for correspondence: Dr. Khushpreet Kaur Mann, 655, Model Town Phase 1, Bathinda 151001, Punjab, India. E-mail: mann.khushpreet@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Nevus of Ota is a facial dermal melanocytic hamartoma occurring more commonly in Asians. The mainstay of treatment is 1064-nm Q-Switched neodymium-doped yttrium aluminum garnet (Nd:YAG) laser, which has shown variable results in pigmented skin.
Objective:
The aim of this study was to determine whether Q-Switched Nd:YAG laser treatment combined with fractional CO2 laser is more efficacious than Q-Switched Nd:YAG laser alone.
Materials and Methods:
This was a prospective study with 81 patients. The patients were randomly divided into two groups. Group 1 received 1064-nm Q-Switched Nd:YAG laser alone and group 2 in addition received a fractional CO2 laser as well. Both groups received six sittings at monthly intervals. The treatment response was documented with physician global assessment (PGA) and patient’s treatment satisfaction on Wong–Baker Facial Pain Scale (WBFPS). Dermoscopic evaluation was done to see subsurface pigment clearance.
Results:
In the combination group, 25% of patients had more than 50% improvement as compared with 5.71% in group 1. To achieve a mean PGA score of 1.4, it took six sessions for group 1 versus only four for group 2. Dermoscopic evaluation showed faster pigment clearance in the combination group.
Conclusion:
Combining two lasers shows statistically significant faster and greater degree of improvement as compared with Q-Switched Nd:YAG laser monotherapy in nevus of Ota.
Keywords
Fractional CO2 laser
nevus of Ota
Q-Switched Nd:YAG laser
INTRODUCTION
Nevus of Ota is a facial dermal melanocytic hamartoma that presents as bluish/slate gray hyperpigmentation. It is typically seen in children or adolescents and more common in females. It is distributed unilaterally in areas supplied by the ophthalmic and maxillary divisions of trigeminal nerve. Most patients seek treatment due to psychological and cosmetic concerns. Histopathological findings include melanocytes dispersed in a ribbon-like pattern in between collagen fibers and around the neurovascular bundles of mid and upper dermis. Dermoscopy of nevus of Ota reveals bluish gray reticular pigmentation with some areas of white and dark brown color.[1] Treatment options were limited before the advent of lasers with poor outcomes. Q-Switched neodymium-doped yttrium aluminum garnet (Nd:YAG) laser revolutionized the treatment of nevus of Ota and has become the mainstay of therapy.[2] Another concept gaining ground for the treatment is combining fractional lasers with Q-Switched Nd:YAG laser. The aim of our study was to compare the effectiveness of the treatment of nevus of Ota with Q-Switched Nd:YAG laser alone versus combination treatment with Q-Switched Nd:YAG laser and fractional CO2 laser.
MATERIALS AND METHODS
A prospective evaluator blinded controlled study was conducted in a tertiary care center after approval by the institutional review board and informed consent. Eighty-one cases were recruited and patients coming at an even number were allotted for Q-Switched Nd:YAG laser alone (group 1) and patients coming at an odd number were allotted for the combination of Q-Switched Nd:YAG laser and fractional CO2 laser (group 2). A total of 40 patients were recruited in group 1 and 41 patients were recruited in group 2. Fourteen patients were lost to follow-up and not included in the final analysis.
Patients under 12 years age, those who previously received more than three sessions of laser treatment or last laser treatment within 3 months, and patients with contraindications to laser treatment such as active local infection and keloid were excluded from the study. Clinical details of onset, duration, progression of symptoms, eye involvement, treatment, and family history of nevus of Ota were noted. Skin, eye, and oral cavity were examined for the presence of pigmentation.
Standardized clinical photographs were taken at every visit with the same digital camera in the same settings.
Physician global assessment (PGA) evaluation was done based on the quartile grading scale at baseline and after each laser session. Response to treatment in terms of clearance of the lesion was graded by an independent observer as follows:
Grade 1: <25% improvement, minimal improvement; Grade 2: 26%–50% improvement, moderate improvement; Grade 3: 51%–75% improvement, marked improvement; and Grade 4: >75% improvement, near total improvement.
Patients who had no improvement or worsening were also documented.
Patient global assessment evaluation was done based on Wong–Baker Facial Pain (WBFPS) score[3] at each visit:
Face 0 does not hurt at all.
Face 2 hurts just a little bit.
Face 4 hurts a little bit more.
Face 6 hurts even more.
Face 8 hurt a whole lot.
Face 10 hurts as much as you can imagine, although you do not have to be crying to have this worst pain.
Dermoscopy was done using the Dermaindia TLS Ultracam 30X (Videodermoscope) [Figure 1]. Color of pigmentation, pigment network, and any other finding were recorded in both high and low power. It was done at baseline, after third and sixth sessions.

- Points taken to perform dermoscopy. First point around biopsy side, second point is 2 cm medial (or lateral) to biopsy site, third point is 2 cm below the second point, fourth is 2 cm below first point
Depth of melanocytes and distribution pattern were noted at baseline on histopathology.
Broad-spectrum sunscreen was given to all patients and was continued throughout the study.
Laser treatment was done following the application of topical anesthesia with eutectic mixture of lignocaine and prilocaine (Prilox) for 1 h under occlusion before laser.
Group 1 patients were treated with 1064 Q-Switched Nd:YAG laser (Quanta system ASSET Milan, Italy) with pulse width 6 ns, 10 Hz frequency, 4 mm spot size, and started with a minimum fluence of 4 J and increased up to a maximum of 7.5 J as per patient’s response. Fluence of 7.5 J was attained by 65.82% of patients after third session and 77.6% after sixth session. Immediate whitening of the skin on laser irradiation was taken as an end point of treatment. Treatment was performed with minimal overlap (approximately 10%). The entire lesion was covered with a single pass.
Group 2 patients were treated with Q-Switched Nd:YAG laser followed by Fractional CO2 laser (Ultra dream pulse surgical CO2 surgical system, MX 7000 scanner type Daeshin Enterprise Co. Ltd, Korea). Micro Xel scanner mode of Fractional CO2 laser was used. It was started at a minimum dose of 12 mJ and increased up to maximum of 30 mJ depending on patient’s response. Treatment was performed with an overlap of 25%. Depth was 3–5 and density was 4. Density 4 in our laser system corresponds to approximately 890 microthermal zones/cm2. Depth levels 1–5 are available for use in our laser system. Higher values of 3–5 were used depending upon the histopathological depth of pigment: 3––for pigment in papillary and superficial reticular dermis, 4––for pigment in mid reticular dermis, 5––for pigment in deep reticular dermis. As reported by Hantash et al.[4] in their study done by ex vivo histological study using fractional CO2 laser with 8–23 mJ and density of 400 microthermal zones/cm2, they could reach the depth of 480–1000 µm. It corresponds to the maximal depth of superficial to mid-reticular dermis.[5]
In both groups, six sessions were performed at intervals of 4 weeks. The endpoint for treatment was taken as near total improvement or till a maximum of six sessions whichever was earlier. Side effects if any were recorded at each visit. Patients were followed till 1 month after completion of six sessions.
Statistical analysis
The data were entered in MS Excel spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) software program, version 21.0. Quantitative variables were compared using an unpaired t test/Mann–Whitney test (when the data sets were not normally distributed) between the two groups. Qualitative variables were correlated using chi-square test/Fisher’s exact test. A value of P < 0.05 was considered statistically significant.
RESULTS
A total of 81 patients were included in the study, 40 in group 1, and 41 in group 2. The mean age of patients was 23.2 ± 6.6 years. Male-to-female ratio was 1:7.1. Mean duration of the presentation was 17.38 ± 8.69 years. Fifty patients (67.90%) had onset of disease at birth, whereas 25 patients (30.86%) had onset in adolescence. One patient had an onset of lesions on the skin at 26 years of age, whereas her left eye was involved since birth. Eight patients had bilateral involvement. Only two patients had a family history of nevus of Ota. Infraorbital and zygomatic were the most common regions involved. Scleral involvement was seen in 85.19% of patients and palate involvement in 13.58% of patients. Homogenous pigmentation with speckled areas in the periphery was the most commonly observed pattern.
On histopathological examination, the majority of patients (61.25%) had melanocytes extending up to superficial reticular dermis, 36.25% patients had melanocytes up to deep reticular dermis, and 2.5% up to mid reticular dermis [Figure 2]. Melanocytes were distributed in between the collagen bundles.
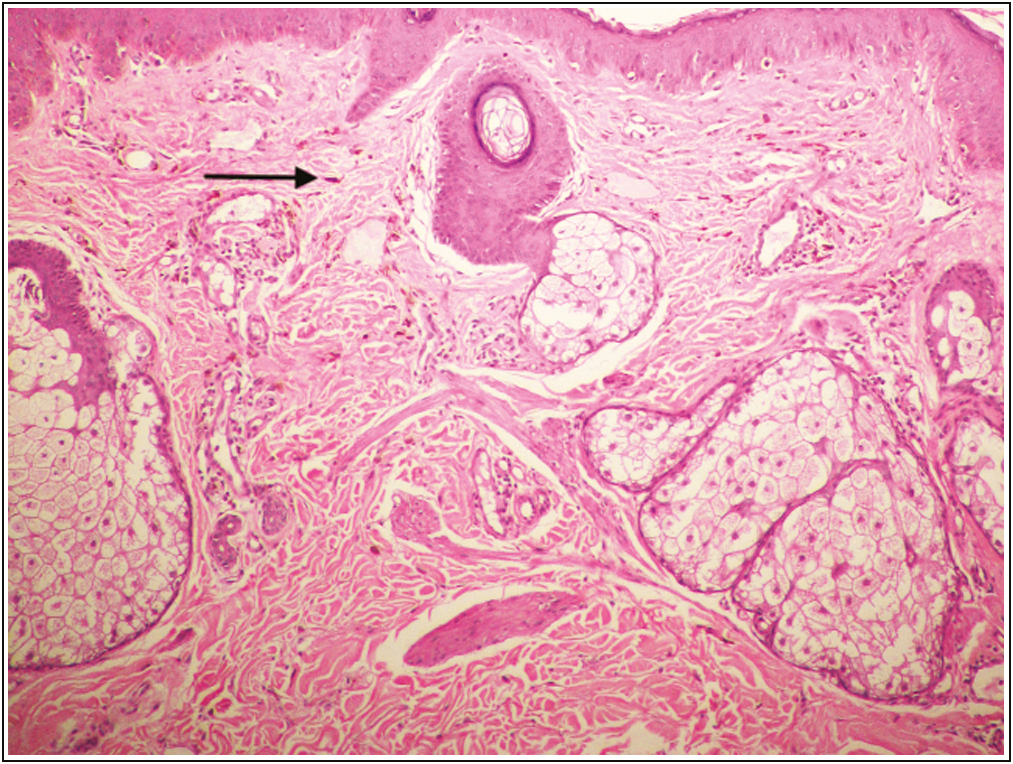
- Histopathology showed bipolar melanocytes (arrow) distributed in between collagen bundles in superficial reticular dermis. 100×
A comparison of PGA and WBFPS scores between group 1 and group 2 patients is shown in Tables 1 and 2.
| Clinical improvement | Group 1 | Group 2 | ||
|---|---|---|---|---|
| After three sessions (n = 39) | After six sessions (n = 35) | After three sessions (n = 40) | After six sessions (n = 32) | |
| No improvement | 4 (10.26%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) |
| PGA 1 (<25% improvement) | 33 (84.62%) | 23 (65.71%) | 29 (72.50%) | 4 (12.50%) |
| PGA 2 (25%–50% improvement) | 2 (5.13%) | 10 (28.57%) | 11 (27.50%) | 19 (59.38%) |
| PGA 3 (50%–75% improvement) | 0 (0.00%) | 2 (5.71%) | 0 (0.00%) | 8 (25%) |
| PGA 4 (75% improvement) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 1 (3.13%) |
After third session, approximately 27% of patients in group 2 compared with 5% in group 1 had grade 2 improvement (P = 0.005). After six sessions, approximately 25% patients in group 2 versus 5% patients in group 1 had grade 3 improvement on PGA scale. Group 2 patients had higher grade of improvement than group 1 patients after six sessions of treatment (P = 0.0001)
| Group 1 | Group 2 | |||
|---|---|---|---|---|
| After three sessions (n = 39) | After six sessions (n = 35) | After three sessions (n = 40) | After six sessions (n = 32) | |
| WBFPS 10 | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) |
| WBFPS 8 | 11 (28.21%) | 2 (5.71%) | 0 (0.00%) | 0 (0.00%) |
| WBFPS 6 | 25 (64.10%) | 13 (37.14%) | 20 (50%) | 1 (3.13%) |
| WBFPS 4 | 1 (2.56%) | 15 (42.86%) | 19 (47.50%) | 6 (18.75%) |
| WBFPS 2 | 1 (2.56%) | 4 (11.43%) | 1 (2.50%) | 23 (71.88%) |
| WBFPS 0 | 0 (0.00%) | 1 (2.86%) | 0 (0.00%) | 2 (6.25%) |
After three sessions, majority of patients (approximately 57%) reported score of 6 on WBFPS scale. Approximately one-third patients in group 1 reported scores of 8 and 10, whereas no patient in group 2 had similar scores. This comparison between two groups was found to be statistically significant (P < 0.0001). After six sessions, approximately 72% patients in group 2 versus 11% patients in group 1 reported WBFPS 2. Higher number of patients in was satisfied with combination treatment than single laser treatment on WBFPS score (P < 0.0001)
Dermoscopy after six sessions showed clearing and lightening of pigment, although the pattern of pigmentation remained the same [Figure 3 and Table 3]. In 53.73% of patients, dermoscopic grade of improvement was similar to clinical improvement [Figure 4]. But in cases with lower clinical improvement (35.82%), dermoscopy showed higher grades of improvement, especially in cases with darker pigmentation.
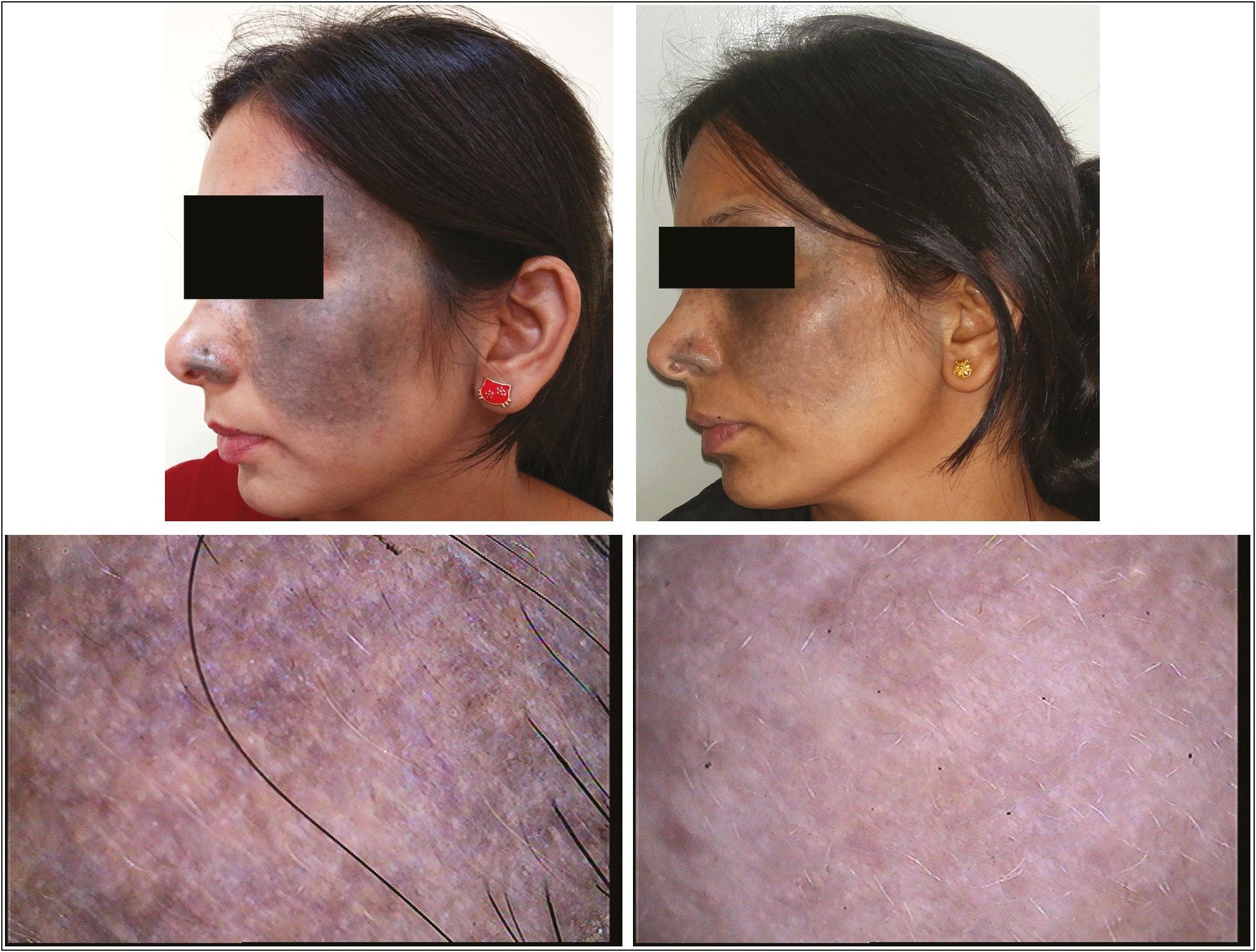
- Pretreatment (A) and posttreatment (B) photographs of group 2 patient showing PGA grade 3 (>50%) improvement. Pre-dermoscopy (C) and post-dermoscopy (D) images of same patient showing grade 3 improvement on dermoscopy after six sessions
| Dermoscopic improvement | Group 1 | Group 2 | ||
|---|---|---|---|---|
| After three sessions (n = 39) | After six sessions (n = 35) | After three sessions (n = 40) | After six sessions (n = 32) | |
| No improvement | 3 (7.69%) | 1 (2.86%) | 1 (2.50%) | 0 (0.00%) |
| Grade1 (<25% improvement) | 31 (79.49%) | 16 (45.71%) | 19 (47.50%) | 1 (3.13%) |
| Grade 2 (25%–50% improvement) | 5 (12.82%) | 12 (34.29%) | 20 (50.00%) | 13 (40.63%) |
| Grade 3 (50%–75% improvement) | 0 (0.00%) | 5 (14.29%) | 0 (0.00%) | 18 (56.25%) |
| Grade 4 (75% improvement) | 0 (0.00%) | 1 (2.86%) | 0 (0.00%) | 0 (0.00%) |
Patients in group 2 (56.25%) showing grade 3 dermoscopic improvement were significantly higher as compared with group 1 (14.29%) (P = 0.01)
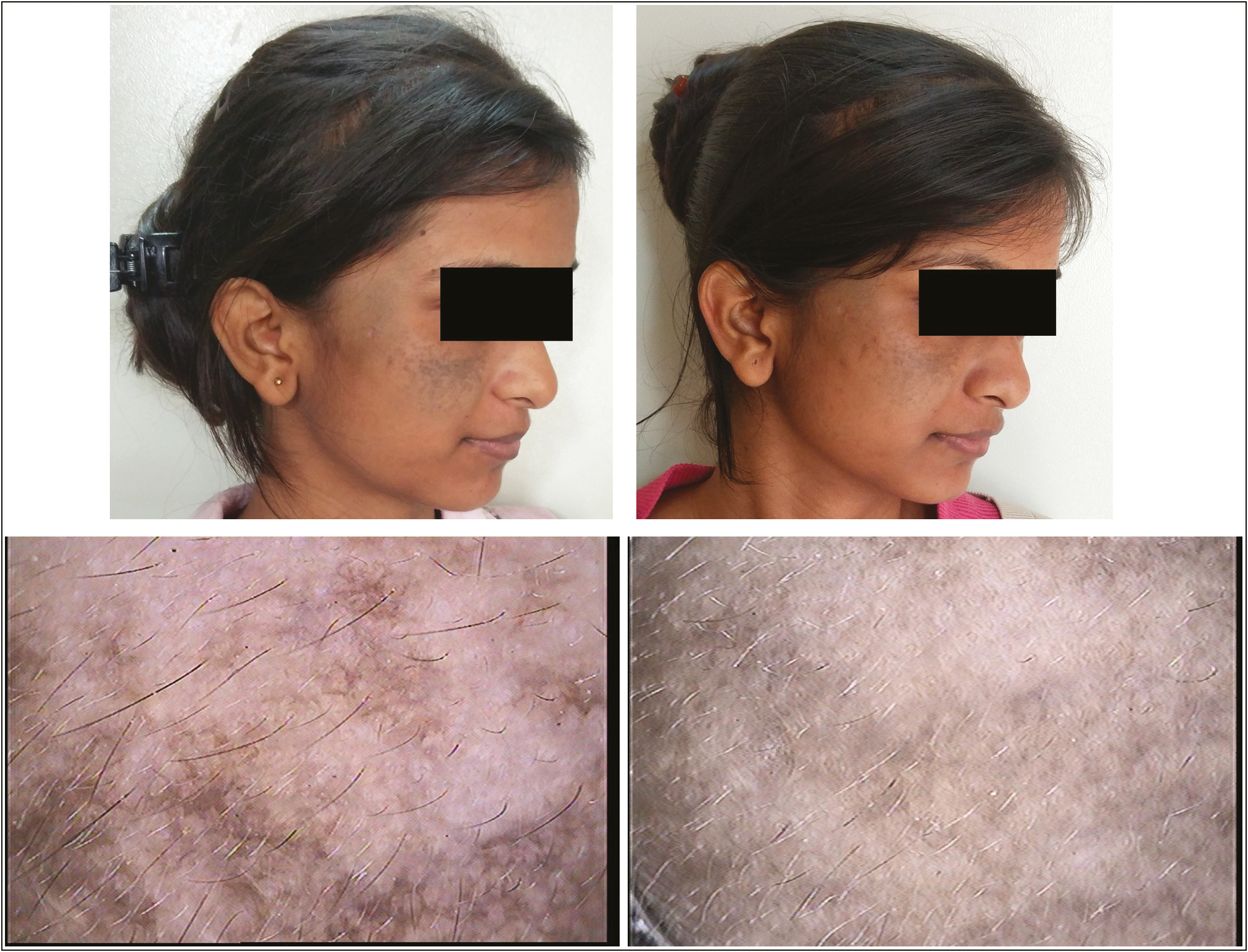
- Pretreatment (A) and posttreatment (B) photographs of group 1 patient showing PGA grade 1 improvement. Pre-dermoscopy (C) and post-dermoscopy (D) images of same patient showing grade 1 improvement on dermoscopy after six sessions
Few reversible side effects were noted such as aggravation of preexisting acne (14.81%), post-inflammatory hyperpigmentation (5.97%), and post-inflammatory hypopigmentation (2.98%). No statistically significant difference was noted in side effects between two groups. Parotido-massetric and buccal regions responded most to treatment with grade 3 improvement in 47.06% and 44.44% of patients, respectively. Orbital was the least responsive region with 73.81% of patients having no improvement (P < 0.0001).
DISCUSSION
Nevus of Ota is a facial dermal melanocytic hamartoma occurring more commonly in Asians. Its onset is typical during childhood or adolescence and nearly all lesions appear by 30 years of age. It is more common in females and male-to-female ratio is 1:4.8.[67] Nevus of Ota is classically distributed unilaterally on areas supplied by the ophthalmic and maxillary divisions of trigeminal nerve. Ocular pigmentation of sclera, cornea, iris, and retina can occur. Hard palate is rarely involved. The pigmentation increases in size and color till puberty.
Histopathological findings show melanocytes dispersed in a ribbon-like pattern in between collagen fibers and around the neurovascular bundles of mid and upper dermis. They run parallel to the skin surface and contain very fine granules of melanin. There is no disturbance of the pattern of collagen and elastic fibers.[8] In our study, the majority of patients had melanocytes extending up to superficial reticular dermis and few patients with extensions up to mid reticular dermis.
Dermoscope is a newer noninvasive diagnostic tool that magnifies subtle surface features of skin lesions and enables visualization of subsurface skin structures normally not visualized with a magnifying glass. Dermoscopy of nevus of Ota has been described by Khopkar as blue grey reticular and globular pigmentation with areas of white and dark brown color.[1] In our study, pseudo-reticular (59.26%) and true reticular (40.74%) patterns were observed along with brown black or blue-black blotches (structureless areas) on dermoscopy.[9] Globular pigmentation or whitish areas were not seen in our patients on dermoscopy. Telangiectasia was present in four patients, which was due to prior topical steroid creams used by these patients.
Before the advent of lasers, nevus of Ota poorly responded to available treatment modalities. QS ruby laser was the first laser reported by Goldberg and Nychay[10] and Geronemus[11] to treat nevus of Ota followed by QS Alexandrite and QS 1064 Nd:YAG lasers.[1213] The Q-switched Nd:YAG laser at a wavelength of 1064 nm is best suited for the treatment of Fitzpatrick types IV–VI as it minimizes the risk of epidermal injury and pigmentary alteration.[14] But the results in pigmented skin are not as good as in fair skin in terms of number of sittings and percentage of improvement because the inherent pigmentation in the epidermis interferes with the laser beam before it targets the nevus cells. Variable results have been reported in Indian studies. Kar et al.[2] showed more than 75% improvement in four out of fifty cases after ten sittings. Sardana et al.[15] noticed a 25% response after ten sittings and Aurangabadkar et al.[7] reported moderate improvement in 33% of patients after six sittings. This difference might be due to use of a subjective quartile system. In our study, we have used multiple evaluation methods such as quartile system PGA, Wong–Baker faces pain rating scale[3] for assessing patients’ satisfaction and dermoscopy to compare results between two groups. Picosecond lasers have shown a more favorable clinical response with fewer treatment sessions and less adverse effects compared with nanosecond lasers.[161718] The comparative data between different Q-switched lasers have shown variable results, one notable fact that emerges is the treatment of pigmentation with combination modalities.[19] The rationale behind the combination therapy is that fractional lasers create micro-thermal zones and micro-ablative zones which allow transepidermal clearance of the pigment along with the micro-epidermal necrotic debris. In addition, creation of microablative zones by fractional lasers allows the release of gases that build up during Q-Switched Nd:YAG laser therapy, thus reducing the chances of blistering.[20] CO2 laser ablation causes scar formation when used alone to treat pigments in reticular dermis. To avoid that, fractional CO2 laser fluences we used were limited to removal of the epidermis and papillary dermis. By doing so, parts of the pigments that were located superficial dermis might have been removed. This makes the deeper pigment more accessible for Q-switched Nd:YAG laser and facilitate their removal. Further, the CO2 laser inflammatory response may enhance phagocytosis and thus help in the removal of Q-switched treated pigment.[20]
In our study, 12 out of 67 patients (17.91%) had more than 50% clinical improvement after six laser sessions. Patients having more than 25% improvement were 2.5 times in combination treatment as compared with monotherapy (87.5% versus 34.28%). Numbers of satisfied patients (score 0 and 2 on WBFPS) were five times (25 versus 5) more in the combination treatment group than in the monotherapy group at the end of six laser sessions (P < 0.005). Group 2 patients achieved mean PGA score of 1.4 after four laser sessions as compared with six sessions in group 1 patients. The combination therapy group achieved 50% improvement after four laser sessions whereas it took six sessions to achieve the same in the monotherapy group. Thus, combination therapy achieves faster clearance than monotherapy by 2 months. Follow-up dermoscopy also showed more statistically significant (P = 0.0001) improvement in the combination treatment group (56.25% with grade 3 improvement) as compared with the monotherapy group (14.29%) after six laser sessions.
Aggravation of preexisting acne is a known side effect of fractional lasers[21] but not seen with Q-Switched Nd:YAG laser. Our study revealed eight patients in group 1 and four patients in group 2 showing aggravation of preexisting acne. It was due to the use of sunscreens by patients in between laser sessions. It was managed conservatively with topical anti-acne medications without skipping the laser session. Transient hyperpigmentation and hypopigmentation can be seen in patients treated with Q-Switched Nd:YAG laser.[27] The incidence of post-inflammatory hypopigmentation was up to 22% after CO2 laser resurfacing as reported in one study.[22] Two patients in group 1 developed hypopigmented lesions over cheeks after the third and fourth laser sessions. The lesions improved spontaneously after skipping one laser session and the treatment was again continued. Although the difference was not statistically significant between the two groups, it was due to higher fluence (7.5 mj/cm2) used in group 1 patients with small spot size and patients who had skin types IV and V. One patient in each group also experienced post-inflammatory hyperpigmentation which was managed with topical kojic acid 2% cream while skipping one laser session. Thus, our study showed ten patients in group 1 and five patients in group 2 with side effects but the difference was not statistically significant (P = 0.199). All patients who were undergoing laser were primed 1 month before starting the laser treatment and higher fluences of CO2 lasers were not used.
Our study showed parotido-massetric and buccal were the most responsive regions to treatment which might be due to relatively thin epidermis allowing more laser light to pass to dermis. Since orbital region was more sensitive to laser injury, lower fluences were used to avoid excessive tissue reaction. It resulted in poor response to treatment. Such has been described as “Panda sign” by Chan et al.[23]
In the majority of patients, clinical improvement (PGA) was similar to the dermoscopic grade of improvement. In patients with darker pigmentation, dermoscopy showed clearance of pigment even though there is less significant clinical improvement. These findings signify that dermoscopy can be a noninvasive objective tool to assess improvement in patients of nevus of Ota treated with laser.
Few limitations were noted in our study, only one patient in our study reported grade 4 improvement on PGA scale. Very few patients (4%) reported WBFPS score of 0 after six sessions of laser therapy. Only one patient reported grade 4 improvement on dermoscopy. All these factors may be attributed to less interval between laser sessions and short duration (1 month) of follow-up period.
CONCLUSION
Treatment of nevus of Ota with the combination of Q-Switched Nd:YAG laser and fractional CO2 laser showed a statistically significant, faster and greater degree of improvement on clinical and dermoscopic evaluation as compared with treatment with Q-Switched Nd:YAG laser alone. Combination therapy can be utilized in larger number of patients with longer duration of follow-up to monitor recurrence of nevus of Ota. Further, dermoscopic evaluation is a noninvasive method and more sensitive indicator of improvement which can be used for the assessment of efficacy of laser treatment.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgement
The authors thank Harsumeet Singh Sidhu for technical help.
References
- Dermoscopy and trichoscopy in diseases of the brown skin atlas and short text (1st ed). New Delhi: Jaypee Brothers Medical Publishers; 2012. p. :60-1.
- 1064 nm Q switched Nd:YAG laser treatment of nevus of Ota: An Indian open label prospective study of 50 patients. Indian J Dermatol Venereol Leprol. 2011;77:565-70.
- [Google Scholar]
- Ex vivo histological characterization of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007;39:87-95.
- [Google Scholar]
- Fractional CO2 laser resurfacing of photoaged facial and non-facial skin: Histologic and clinical results and side effects. J Cosmet Laser Ther. 2009;11:190-201.
- [Google Scholar]
- QYAG5 Q-switched Nd:YAG laser treatment of nevus of Ota: An Indian study of 50 patients. J Cutan Aesthet Surg. 2008;1:80-4.
- [Google Scholar]
- Rook’s textbook of dermatology Vol 54. (8th ed). West Sussex UK: Blackwell Publishing; 2010. p. :8-9.
- Standardization of terminology in dermoscopy/dermatoscopy: Results of the third consensus conference of the international society of dermoscopy. J Am Acad Dermatol. 2016;74:1093-106.
- [Google Scholar]
- Q-switched ruby laser treatment of nevus of Ota. J Dermatol Surg Oncol. 1992;18:817-21.
- [Google Scholar]
- Treatment of nevus of Ota by the Q-switched alexandrite laser. Dermatol Surg. 1995;21:592-6.
- [Google Scholar]
- Argon and Q-switched yttrium-aluminum-garnet laser treatment of nevus of Ota. Ann Plast Surg. 1995;35:150-3.
- [Google Scholar]
- Laser treatment of tattoos in darkly pigmented patients: Efficacy and side effects. J Am Acad Dermatol. 1996;34:653-6.
- [Google Scholar]
- Are Q-switched lasers for nevus of Ota really effective in pigmented skin? Indian J Dermatol Venereol Leprol. 2012;78:187-9; author reply 189-90.
- [Google Scholar]
- Picosecond pulse duration laser treatment for dermal melanocytosis in Asians: A retrospective review. Laser Ther. 2016;25:99-104.
- [Google Scholar]
- Usefulness of picosecond pulse alexandrite laser treatment for nevus of Ota. Laser Ther. 2018;27:251-5.
- [Google Scholar]
- Comparison of a picosecond alexandrite laser versus a Q-switched alexandrite laser for the treatment of nevus of Ota: A randomized, split-lesion, controlled trial. J Am Acad Dermatol. 2020;83:397-403.
- [Google Scholar]
- Combining fractional resurfacing with Q-S ruby laser for tattoos. Dermatol Surg. 2010;36:1-3.
- [Google Scholar]
- Combination of CO2 and Q-switched Nd:YAG lasers is more effective than Q-switched Nd:YAG laser alone for eyebrow tattoo removal. J Cosmet Laser Ther. 2015;17:65-8.
- [Google Scholar]
- Side effects and complications of fractional laser photothermolysis: Experience with 961 treatments. Dermatol Surg. 2008;34:301-5; discussion 305-7.
- [Google Scholar]
- The short- and long-term side effects of carbon dioxide laser resurfacing. Dermatol Surg. 1997;23:519-25.
- [Google Scholar]
- Nevus of Ota: A new classification based upon the response to laser treatment. Laser Surg Med. 2001;28:267-72.
- [Google Scholar]






