Translate this page into:
Novel treatment of Hori's nevus: A combination of fractional nonablative 2,940-nm Er:YAG and low-fluence 1,064-nm Q-switched Nd:YAG laser
Address for correspondence: Dr. Brian Wei Cheng Anthony Tian, Singapore General Hospital, Outram Rd, Pin 169608, Singapore. E-mail: briananthonytian@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
To demonstrate a combination laser therapy to treat Hori's nevus.
Design:
A prospective study.
Setting:
A Singapore-based clinic.
Participants:
Five female patients, aged 30-46 years, with bilateral malar Hori's nevus.
Measurements:
Photographs were taken before treatment and 1 month after laser treatment was completed. These were graded by three independent physicians. The patients were also asked to grade their treatment response subjectively. They were followed up for a total of 3 months after laser treatment to monitor recurrence.
Materials and Methods:
The fractional nonablative 2,940-nm Er:YAG laser with a fluence of 0.7 J/cm2, spot size 12 mm, and frequency 15 Hz was used to perform a full-face single-pass treatment. Subsequently, a second pass and third pass over Hori's nevi were done bilaterally till the clinical endpoint of skin whitening. The 1,064-nm Q-switched (QS) Nd:YAG at a fluence of 2.0 J/cm2, frequency 2 Hz, and 4-mm spot size was used to deliver multiple passes over Hori's nevus till erythema with mild petechiae appeared. We repeated the treatment once a week for 3 more consecutive weeks.
Results:
All five patients had above 80% improvement in their pigmentation and two (skin type III) achieved complete 100% clearance. Based on the patients’ subjective assessments, all five of them expressed satisfaction and felt that their pigmentation had improved. There were no complications noted.
Conclusion:
The fractional nonablative 2940 nm Er:YAG laser and Q-switched 1064nm laser Nd:YAG combination is an effective and safe treatment for Hori's nevus.
Keywords
Hori's nevus
facial pigmentation
combination laser
nonablative Er:YAG laser
Q-switched Nd:YAG laser
INTRODUCTION
Acquired bilateral nevus of Ota-like macules (Hori's nevus) is common among Asian women.[12] Clinically, it resembles the nevus of Ota characterized by bilateral blue-brown macules on the forehead, malar, and nasal areas.[3] However, the nevus of Ota is a congenital lesion, whereas Hori's nevus appears in the third to fifth decades of life. Hori's nevus also does not involve the conjunctivae and mucous membranes. Histologically, melanocytes are distributed evenly throughout the dermis in the nevus of Ota while melanocytes are in the papillary and middle portions of the dermis in Hori's nevus.[45]
Lasers have been effective in treating nevus of Ota.[6789] These include QS Nd:YAG, ruby laser, and alexandrite laser.[101112] Dermabrasion has been found to be effective as well.[13] However, treatment responses have been noted to be less effective for Hori's nevus.[12] For Hori's nevus, multiple expensive laser treatments have to be used. This takes a long time and complete resolution is not always possible.
Two reports have described combination laser therapy for Hori's nevus. Manuskiatti et al. used a scanned CO2 laser and QS Nd:YAG laser[14] while Hock et al. used a 532-nm potassium titanyl phosphate (KTP) laser and QS Nd:YAG laser.[15] Both showed better results with combination therapy than with Nd:YAG alone.[1415]
In this paper, we present a novel technique of using a fractional 2,940-nm Er:YAG and a 1,064-nm QS Nd:YAG laser to successfully treat a series of Hori's nevus.
MATERIALS AND METHODS
Five Chinese women were enrolled in the study. Exclusion criteria included chemical peel, laser, intense pulsed light treatment in the last year, and pregnancy. The age of the patients ranged 30-46 years. Only those subjects with bilateral malar lesions were included. Four patients had Fitzpatrick skin type III and one had skin type IV. Informed consent was obtained.
The patients had their faces cleansed before the treatment. There was no anesthesia involved. We used the fractional nonablative 2,940-nm Er:YAG laser (SP Spectro, Fotona, Ljubljana, Slovenia) with a fluence of 0.7 J/cm2, spot size 12 mm, and frequency 15 Hz. We carried out a full-face single-pass treatment. Subsequently, we performed a second pass and third pass over Hori's nevi bilaterally till the clinical endpoint of skin whitening was observed. No wiping was performed between the passes. We then used the 1,064-nm Q-switched (QS) Nd:YAG laser. (RevLite, Cynosure Co., Fremont, CA, USA) at a fluence of 2.0 J/cm2, frequency 2 Hz, and spot size 4 mm. We used multiple passes over Hori's nevus till erythema with mild petechiae appeared. The Er:YAG laser was performed as a singular session. The QS Nd:YAG laser treatment was repeated weekly for 3 more consecutive weeks.
The skin was kept cool during treatment with cryogen spray. After laser treatment, the patients applied topical fusidic acid for 3 days and sunscreens during daytime (for the entire study duration).
Photographs were taken before treatment and 1 month after the last laser treatment. These were evaluated by three independent physicians. The degree of improvement was graded into the following five levels of response: no change (0%), noticeable lightening (<25% improvement), mild lightening (25-50% improvement), moderate lightening (50-75%), and marked lightening to complete clearance (75-100%).[14] The patients also graded their treatment responses subjectively. They were followed up clinically for a total of 3 months after the laser treatment for monitoring of postinflammatory hyperpigmentation (PIH) and recurrence.
RESULTS
All the patients experienced 5-7 days of erythema and skin scaling following the first treatment session. This downtime was attributed to the Er:YAG. When the scaling resolved within the week, the patients reported noticing a lightening of the Hori's nevus. At the end of 1 month after the laser treatment started, three independent physicians scored them.
All the physicians reported that all the patients had >80% improvement in their pigmentation, with two patients (skin type III) achieving complete 100% clearance [Figures 1 and 2]. Based on the patients’ subjective assessment, all the five patients expressed satisfaction and felt that their pigmentation had improved. The patients were to be followed up for another 2 months (without further treatment). No PIH, hypopigmentation, or recurrence was seen.
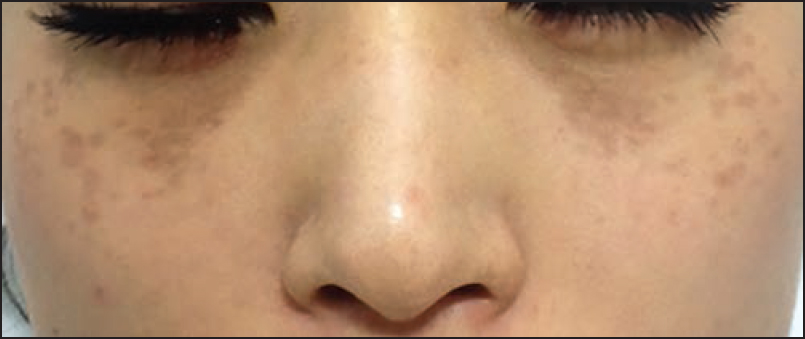
- Pretreatment photo

- After 1 month of laser treatment
DISCUSSION
There are reports on the use of lasers to clear Hori's nevus.[101112] However, obtaining a satisfactory response takes multiple treatments and complete clearance is not always possible. Research on methods to improve the therapeutic effectiveness of lasers on Hori's nevus have shown that response rates have improved with combination lasers.[1415161718] However, there are no reports on the Er:YAG and Nd:YAG laser combination.
In this study, we demonstrated that the Er:YAG and Nd:YAG combination is safe with minimal downtime and no complication. The results were also very good (>80% improvement) and the condition did not recur after 3 months of follow-up. Such clearance rates with minimal treatment session are unprecedented.
Combination laser therapy is synergistic and effective. The following are postulated mechanisms: First, when the Er:YAG laser is used prior to the Nd:YAG laser, it partially ablates the epidermis that removes epidermal melanin. This allows less competition and less scattering of the Nd:YAG laser, leading to more effective penetration.[14151819] Second, the occurrence of an increased collagen fiber density due to the effects of the Er:YAG may mask the residual underlying dermal melanocytes, making the nevus appear lighter.[672021]
The other benefit of combination therapy is that with two lasers working on different targets synergistically, we can adopt a lower fluence for each laser type. This reduces the chance of complications such as PIH.
Research has demonstrated that the Nd:YAG laser and CO2 laser combination also work well.[14] However, we believe that our Er:YAG and Nd:YAG combination is more ideal. This is because CO2 is an ablative laser and can cause erythema that takes about 3 months postoperatively to resolve.[14] CO2 laser can also cause bleeding and scarring. Comparatively, the use of the nonablative Er:YAG has a downtime of only 5-7 days that includes erythema on the first 2 days followed by generalized peeling over the next 3-5 days. Therefore, our combination therapy is ideal because it provides a solution that has a balance of effectiveness and yet minimal downtime and complications.
It is imperative for research to be conducted to elucidate the exact mechanism by which combination therapy works. It is also important to conduct larger prospective trials to elucidate the exact settings for the lasers. It may also be worthwhile to study a comparison between CO2 laser or Er:YAG laser as a combination laser and Nd:YAG laser. It is also important to follow up for even longer durations to monitor recurrence.[1011]
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Circumscribed dermal melanoses. Classification and histologic features. Dermatol Clin. 1988;6:315-26.
- [Google Scholar]
- Nevus of ota. In: Fitzpatrick TB, Kukita A, Morikawa F, Seiji M, Sober AJ, Toda K, eds. Biology and Diseases of Dermal Pigmentation Vol 1. (1st ed). Tokyo: University of Tokyo Press; 1981. p. :67-76.
- [Google Scholar]
- Electron microscopy. Ultrastructural observations of the extracellular sheath of dermal melanocytes in the nevus of Ota. Am J Dermatopathol. 1982;4:245-51.
- [Google Scholar]
- Treatment of nevus of Ota by Q-switched ruby laser. J Am Acad Dermatol. 1994;30:743-51.
- [Google Scholar]
- Treatment of nevus of Ota by the Q-switched alexandrite laser. Dermatol Surg. 1995;21:592-6.
- [Google Scholar]
- An in vivo trial comparing the clinical efficacy and complications of Q-switched 755 nm alexandrite and Q-switched 1064 nm Nd:YAG lasers in the treatment of nevus of Ota. Dermatol Surg. 2000;26:919-22.
- [Google Scholar]
- Q-switched ruby laser therapy of acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1999;25:938-41.
- [Google Scholar]
- Q-switched Nd:YAG laser treatment for acquired bilateral nevus of ota-like maculae: A long-term follow-up. Lasers Surg Med. 2000;26:376-9.
- [Google Scholar]
- Treatment of Hori's nevus with the Q-switched Nd:YAG laser. Dermatol Surg. 2000;26:477-80.
- [Google Scholar]
- Dermabrasion is an effective treatment for acquired bilateral nevus of Ota-like macules. Dermatol Surg. 1996;22:559-62.
- [Google Scholar]
- Treatment of acquired bilateral nevus of Ota-like macules (Hori›s nevus) using a combination of scanned carbon dioxide laser followed by Q-switched ruby laser. J Am Acad Dermatol. 2003;48:584-91.
- [Google Scholar]
- Treatment of acquired bilateral nevus of ota-like macules (Hori›s nevus) with a combination of the 532 nm Q-Switched Nd:YAG laser followed by the 1,064 nm Q-switched Nd:YAG is more effective: prospective study. Dermatol Surg. 2006;32:34-40.
- [Google Scholar]
- Combination therapy for nevus of Ota with the Q-switched ruby laser, CO2 laser, and dermabrader. J Kor Soc Laser Med. 1998;2:46.
- [Google Scholar]
- Combination treatment of melasma with pulsed CO2 laser followed by Q-switched alexandrite laser: A pilot study. Dermatol Surg. 1999;25:494-7.
- [Google Scholar]
- Treatment of facial skin using combinations of CO2, Q-switched alexandrite, flashlamp-pumped pulsed dye, and Er:YAG lasers in the same treatment session. Dermatol Surg. 2000;26:114-20.
- [Google Scholar]
- CO2 laser resurfacing of tattoos prior to Q-switched laser treatment. Lasers Surg Med (Suppl 12):23.
- [Google Scholar]
- Response of naevus of Ota to Q-switched ruby laser treatment according to lesion colour. Br J Dermatol. 2000;142:77-83.
- [Google Scholar]
- Light and electron microscopic investigation of the process of healing of the naevus of Ota by Q-switched alexandrite laser irradiation. Virchows Arch. 1997;431:63-71.
- [Google Scholar]






