Translate this page into:
Occipital Donor Area Grading and Profile in Indian Population
Address for correspondence: Dr. Muthuvel Kumaresan, Cutis Skin Clinic and Hair Transplant Center, 43/20 Third Cross, Om Ganesh Nagar, Vadavalli, Coimbatore 641041, India. E-mail: dr_kumaresh@yahoo.co.in
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Safe donor area (SDA) in hair transplant surgery had been categorized by various studies. We designed a study to profile the occipital donor area in our population and devise a grading scale the donor area.
Aim:
To profile and grade the pattern of receding hair over the occipital donor area among men in the age group of 50–55 years with androgenetic alopecia (AGA).
Materials and Methods:
A total of 681 men with AGA (grade 3 and above Norwood scale, diffuse unpatterned AGA, and retrograde AGA) in the age group between 50 and 55 were included in the study group. Their occipital donor area was analyzed and photographed with the head in the sagittal plane. A team of two dermatologists graded the hair loss and the pattern of the receding hair over the occipital donor area and devised a grading scale and profiled the donor area.
Results:
Grades 1, 2, and 3 occipital donor area constituting 76.05% of the subjects analyzed, fulfilled the standard SDA criteria and 22.31% of the subjects did not fit well into the standard SDA widely followed. Diffuse thinning and reverse thinning of the occipital donor area was observed among the subjects.
Conclusion:
There is no clear cut defined SDA. There are lot of individual variations in SDA. SDA selection should be always conservative and over harvesting of the occipital donor region should be avoided.
Keywords
Grading
hair transplant
safe donor area
INTRODUCTION
Safe donor area in hair transplantation (HT) had been categorized by various studies. We designed a study to profile the occipital donor area in our population and grade the donor area.
Aim
The aim of this article is to profile and grade the pattern of receding hair over the occipital donor area among men in the age group of 50–55 years with androgenetic alopecia (AGA).
MATERIALS AND METHODS
A total of 681 men with AGA (grade 3 and above Norwood scale, diffuse unpatterned AGA, and retrograde AGA) in the age group between 50 and 55 were included in the study group. Their occipital donor area was analyzed and photographed with the head in the sagittal plane. A team of two dermatologists graded the hair loss and the pattern of the receding hair over the occipital donor area and devised a grading scale based on the location of the lowest point of the occipital fringe from the imaginary horizontal line connecting the superior surface of the helix of the ear (grades 1–5 with or without diffuse hair loss and reverse thinning).
Grade 5—the lowest point of the occipital fringe is below the horizontal line connecting the superior surface of the helical rim.
Grade 4—the lowest point of the occipital fringe is at the level of the horizontal line.
Grade 3—lowest point of the occipital fringe is at the distance of up to 3 cm from the horizontal line.
Grade 2—the lowest point of the occipital fringe is at a distance of 3–5 cm. Is it up to 5 cm? Else next category from the horizontal line.
Grade 1—the lowest point of the occipital fringe is at the distance of more than 5 cm from the horizontal line. How does this grading system correlate with safe donor area (SDA) definitions?
Subjects with a density of <30 follicular units/cm identified by trichoscopy over three random regions of occipital, parietal, and temporal area corresponding to Unger’s safe donor area were categorized as diffuse thinning (DT). Subjects with retrograde AGA were diagnosed clinically, and those with >20% variation in hair shaft diameter by trichoscopy were categorized as reverse thinning (RT). The presence of DT and RT as a standalone finding or in any of the above-mentioned grades was also noted and documented.
RESULTS
Grade 1 pattern was found in 29.07% (198) [Figure 1], grade 2 pattern was found in 26.57% (181) [Figure 2], grade 3 pattern was found in 22.02% (150) [Figure 3], grade 4 pattern was found in 18.20% (124) [Figure 4], and grade 5 pattern was found in 4.11% (28) [Figure 5 and Table 1]. RT alone was found in 0.6% (4) [Figure 6], and DT alone was found in 1.17% (8) [Figure 7] subjects. DT over the occipital donor area in all the grades was found in 7.63% (52), RT in all the grades was found in 22.02% (150), and both RT and DT in the same subject was found in 2.05% (14) [Figure 8].
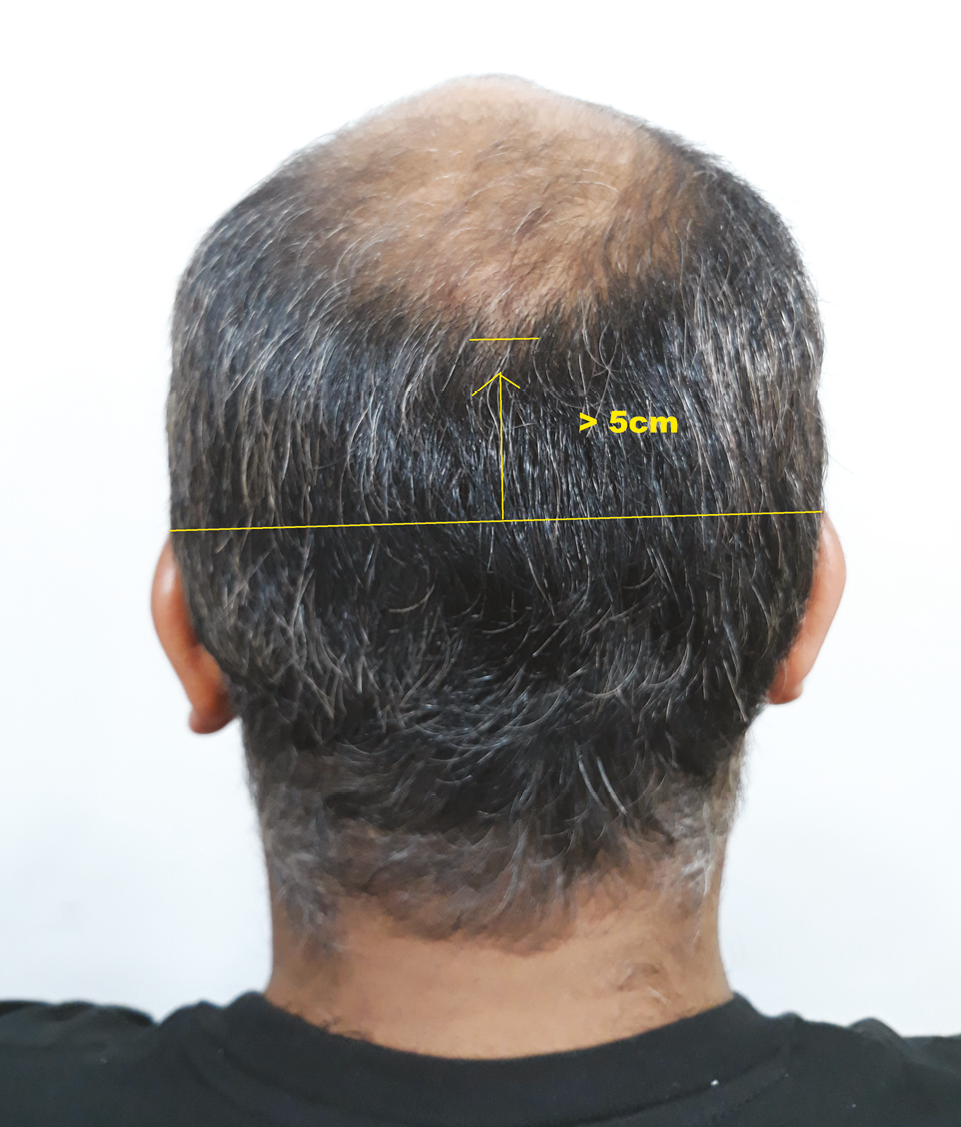
- Donor area grade 1
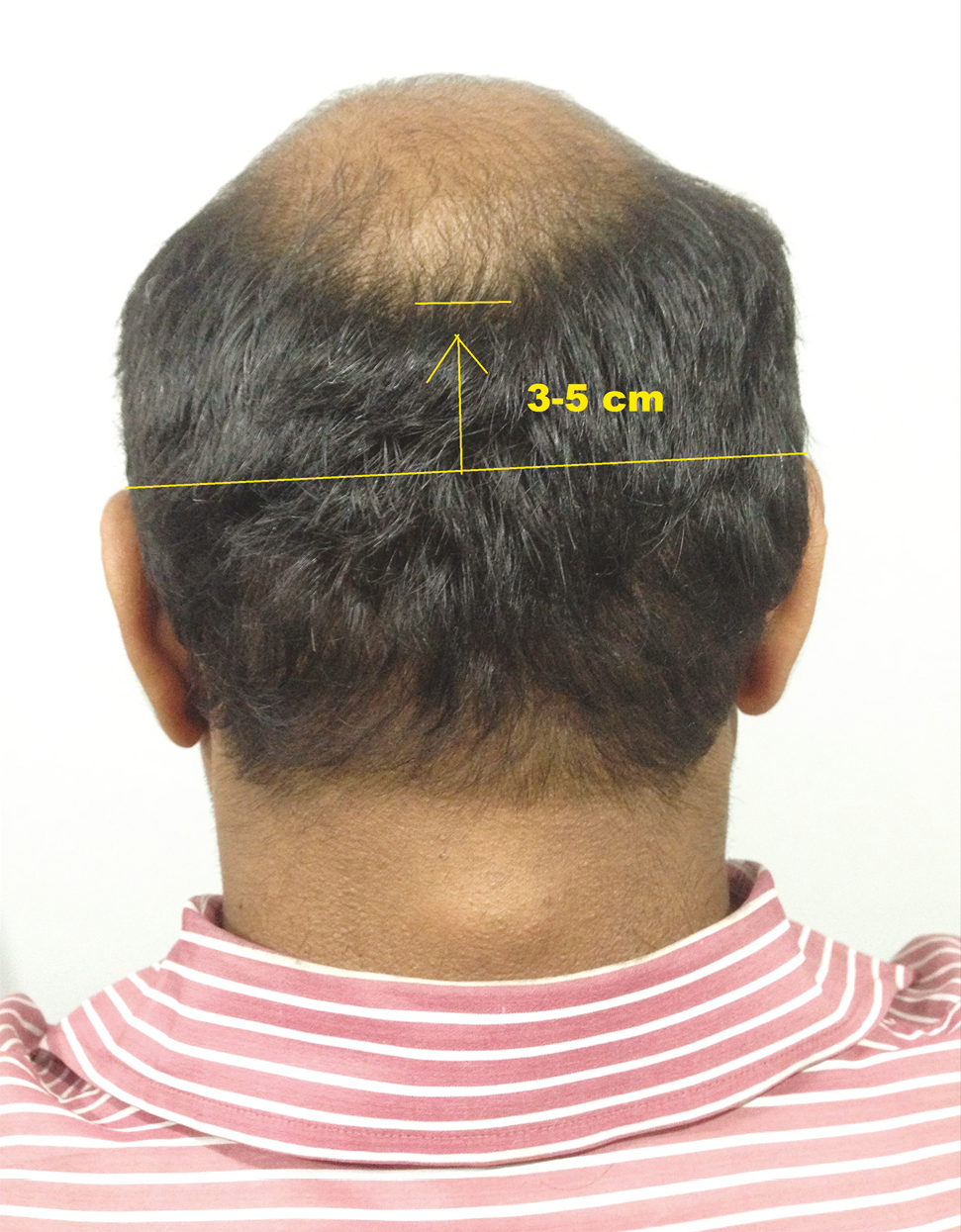
- Donor area grade 2

- Donor area grade 3

- Donor area grade 4

- Donor area grade 5
| Donor area grade | % | Number of subjects (n = 681) |
|---|---|---|
| 1 | 29.07 | 198 |
| 2 | 26.57 | 181 |
| 3 | 22.02 | 150 |
| 4 | 18.20 | 124 |
| 5 | 4.11 | 28 |

- Reverse thinning

- Diffuse thinning

- DT and RT in the same subject
DISCUSSION
Hair follicles located over the occipital region were considered to be androgen-resistant and thought to be permanent and hence these follicles are utilized as the donor in hair transplant surgery for AGA.[1] SDA was first suggested by Unger et al.[2] in 1994 and this continues to be the global standard. The other SDA definitions are from Alt et al.[345] Among these, SDA definition by Unger and Cole [Figure 9] has pictorial comparison of SDA. What they gave is being widely followed. In clinical practice, retrograde AGA/reverse pattern hair loss, diffuse AGA, and possibility of miniaturization in occipital scalp were also observed routinely. These factors were not clearly addressed in the standard SDA definition. Recently, with the advent of mega sessions of follicular unit excision (FUE), the grafts being harvested over larger parts of occipital scalp, questions have been raised as to what is SDA and whether it is wise to harvest from all areas of occipital scalp. In this study, we intended to profile the donor area in our population.
![SDA definitions by Unger et al.[8]](/content/173/2023/16/2/img/JCAS-16-101-g009.png)
- SDA definitions by Unger et al.[8]
Although various grading scales for AGA have been published and widely followed, there are no grading scales for the donor area described in the literature. We tried to formulate a grading scale to define the donor area objectively by keeping the horizontal line connecting the superior rim of the helix of the ear as a landmark. Based on the distance of the lowest point of the receding occipital fringe from this line, donor area was categorized into five grades. How is grade classified? What level of miniaturization was taken to differentiate one from the other? Means grade 4–5? Where would you place your line depending on what level of miniaturization? Its usually a transition in most of the patients not a cutoff line. So what level is taken to consider next grade? The grading scale described in this study can be a simple, objective, and a useful grading scale for defining the donor area in all the age groups.
There are limited studies to assess the SDA in Indian population.[6] We tried to profile the donor area in our population in men with AGA falling in the age group between 50 and 55 years, since epidemiologically 50% men at this age group would have AGA.[7] The donor area was categorized into five types according to our grading scale; among these five types, grades 1, 2, and 3 constitute occipital donor area constituting 78% of the subjects and fulfilled the SDA criteria by Unger and Cole. Grades 4 and 5 have occipital area constituting that 22% of the subjects did not fit well into the SDA definition by Unger and Cole. Unger had described that 80% of men under the age group of 80 years would fulfill the SDA definition.[28] In our study population, only 76% under the age group of 55 years fulfilled the definition of Unger’s SDA. These data highlight the importance of defining the SDA among various races, and extrapolating the SDA from Western data might not suit the Indian population. What suggestions are given to assess the donor area vis-à-vis hair transplant? What level to take and what not to?
In our study group, DT was observed in 7.63% of the subjects, and diffuse unpatterned hair loss over the occipital donor region was not accounted for in any of the earlier SDA definition by Unger et al. In one of the subjects, DT over the occipital region led to visibility of strip surgery scar performed in the past [Figure 10]. These findings highlight the possibilities of DT in the donor area with advancing age, which shows the practical relevance of this classification.

- DT over the donor area with the visibility of the previous strip surgery scar
In our study group, RT was observed in 22.02% of the subjects and in some subjects this retrograde thinning extended up to the occipital protuberance extending into the standard SDA in some subjects [Figure 11]. We observed the RT in many patterns among the subjects, paralleling the pattern of occipital fringe, as a straight line from the inferior hair line, on either side and on the central portion alone. Possibility of RT with advancing age needs to be considered while harvesting the hair follicles, particularly in FUE.

- RT extending up to occipital protuberance
Among the study population, 0.6% (4) had RT alone without the receding of occipital fringe and 1.17% (8) had DT alone. DT and RT were observed in all the grades (1–5) in our study group [Table 2]. These findings highlight the possibilities of thinning of hair follicles in the so-called permanent zone of hair.
| Donor area grade | Number of subjects with DT | Number of subjects with RT |
|---|---|---|
| 1 | 8 | 8 |
| 2 | 12 | 20 |
| 3 | 10 | 54 |
| 4 | 16 | 60 |
| 5 | 6 | 8 |
Findings from our study demonstrate that miniaturization does affect the hair follicles located over the SDA. The pattern of miniaturization is unpredictable and highly variable. The possibilities of thinning of hair over the donor area with advancing age, DT, and RT affecting the donor area should be discussed with the patients prior to the hair transplant surgery, as this may bring down the long-term survival of the grafted follicles and may lead to poor results.
CONCLUSION
There is no clear-cut defined SDA. SDA might vary among different races; a proper history, careful assessment of future hair loss progression, family history, pattern of hair loss in the family, and the possibilities of DT and RT over the occipital region should be analyzed and discussed with the patient prior to the hair transplant surgery. SDA selection should always be conservative and over harvesting of the occipital donor region should be avoided.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Effects of hormones on hair. In: Mysore V, ed. Hair transplantation (1st ed.). New Delhi, India: Jaypee; 2016. p. :21-3.
- [Google Scholar]
- Delineating the “safe” donor area for hair transplanting. Am J Cosmet Surg. 1994;11:239-43.
- [Google Scholar]
- An overview of the donor area: Basic principles. In: Unger WP, Shapiro R, Unger R, Unger M, eds. Hair transplantation (5th ed.). New York: Informa Health Care; 2011. p. :247-62.
- [Google Scholar]
- Follicular transplantation. Patient evaluation and surgical planning. Dermatol Surg. 1997;23:771-84; discussion 801-5.
- [Google Scholar]
- Predicting the permanent safe donor area for hair transplantation in Koreans with male pattern baldness according to the position of the parietal whorl. Arch Plast Surg. 2014;41:277-84.
- [Google Scholar]
- Assessment of safe donor zone of scalp and beard for follicular unit extraction in Indian men: A study of 580 cases. J Cutan Aesthet Surg. 2019;12:31-5.
- [Google Scholar]
- Androgenetic alopecia: An update. Indian J Dermatol Venereol Leprol. 2013;79:613-25.
- [Google Scholar]






