Translate this page into:
Osteonevus of Nanta: A rare presentation in a young female with comprehensive dermoscopic and histopathological findings
*Corresponding author: Anil Kumar, Department of Dermatology, Venereology and Leprosy, Institute of Naval Medicine, INHS Asvini, Mumbai, Maharashtra, India. asunilk22@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Srinivasan P, Kharayat V, Kumar A, Bhatt S, Reddy A. Osteonevus of Nanta: A rare presentation in a young female with comprehensive dermoscopic and histopathological findings. J Cutan Aesthet Surg. doi: 10.25259/JCAS_151_2024
Abstract
Osteonevus of Nanta, or osseous metaplasia in a melanocytic nevus, is a rare dermatological entity characterized by the presence of bone tissue within a nevus. It has an extremely low prevalence, with few documented cases globally. Awareness of its clinical, dermoscopic, and histopathological features is crucial for accurate diagnosis. A 24-year-old female presented with a dark-colored, pea-sized swelling on her left cheek. Dermoscopy revealed a homogeneous brownish background, a central dark area, and peripheral lighter pigmentation consistent with a compound melanocytic nevus. Histopathology confirmed an intradermal nevus with lamellar bone formation, diagnostic of osteonevus of Nanta. Surgical excision of the lesion provided both diagnostic confirmation and cosmetic resolution, highlighting the role of surgery as the definitive management modality. The etiology of osteonevus of Nanta is still debated, but it is thought to result from chronic inflammation or trauma. Dermoscopy aids in pre-operative differentiation from other calcified lesions. This case adds to the limited literature on osteonevus of Nanta, emphasizing the importance of considering this rare entity in the differential diagnosis of nodular lesions with bony consistency.
Keywords
Dermal bone formation
Dermoscopy
Histopathology
Ossified nevus
Osteonevus of Nanta
INTRODUCTION
Osteonevus of Nanta, a rare variant of intradermal melanocytic nevi with osseous metaplasia, was first described by Nanta in 1911.1,2 This condition is primarily observed in the head-and-neck region with an incidence of <0.1% in documented intradermal nevi.3,4 Despite its rarity, clinicians should be aware of this condition to avoid misdiagnosis as other osseous or calcified lesions.
CASE REPORT
A 24-year-old female presented with a solitary, pea-sized, dark-colored swelling on her left cheek, present since childhood. It began as a pinhead-sized papule and slowly increased over 15 years to its current size, about 5 times its original size. The lesion is asymptomatic, with no pain, itching, discharge, or ulceration. There is no bleeding, rapid growth, or recent changes in size, shape, or color. She denies trauma, infection, or manipulation, such as threading or waxing. No history of oral contraceptive use, sunburn, or excessive sun exposure. There are no similar lesions elsewhere, no family history of similar lesions or malignancies, and no systemic symptoms such as weight loss, fever, or night sweats. She has had no prior procedures on the lesion and is seeking treatment for the 1st time.
Clinical examination
On examination, the lesion was a well-defined, raised, pigmented nodule measuring approximately 0.6 cm in diameter. The surface was smooth and the color was uniformly dark brown to black. There was the presence of both terminal and vellus hairs noted. No surrounding erythema or satellite lesions were noted. No telangiectasia or central punctum was visible. The lesion was firm in consistency and non-tender on palpation. No regional lymphadenopathy is noted [Figures 1a and b].

- (a) A 24-year-old female presented with a dark-colored, pea-sized swelling on her left cheek. (b) Post-excision of the lesion.
Dermoscopic examination
Dermoscopy revealed a homogeneous brownish background with multiple dark blue-gray dots and globules. Multiple terminal and vellus hairs emerging from the lesion were observed, consistent with a compound melanocytic nevus. The presence of white structures, suggestive of osseous formation, was noted [Figure 2].
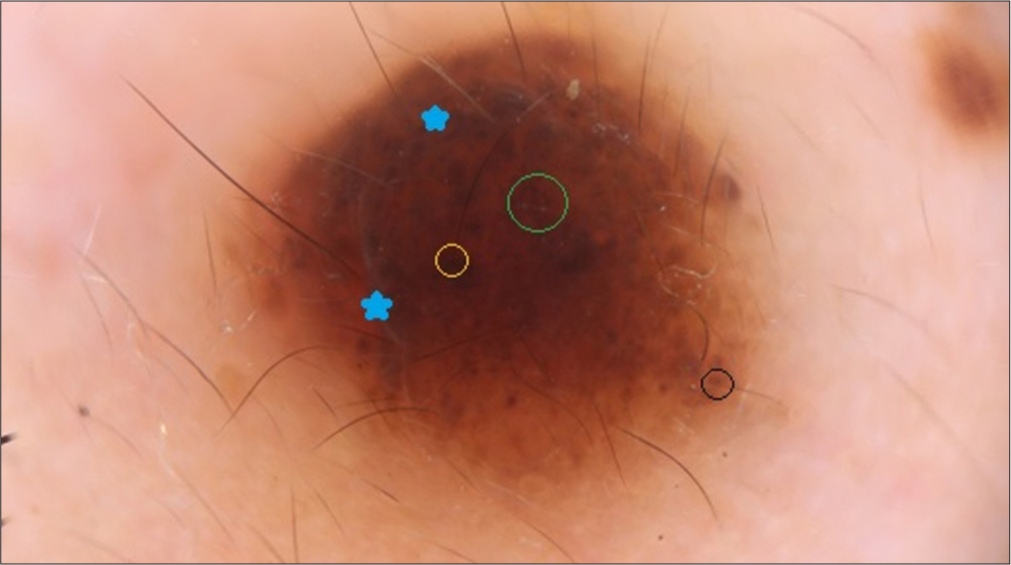
- Dermoscopic image of a compound melanocytic nevus shows white structures (blue stars), suggestive of osseous formation, indicating possible fibrosis or calcification, homogeneous brown background with dark blue-gray dots and clods (green circle), terminal (yellow circle), and vellus hairs (black circle).
The lesion was excised under local anesthesia using a fusiform incision with a 2 mm margin of surrounding healthy tissue, aiming to achieve both diagnostic clarity and cosmetic improvement.
Histopathological examination revealed a dermal-based, symmetric lesion localized to the superficial and mid-dermis, with no epidermal involvement, indicating benign growth. Nevus cells were arranged in nests and reticulated patterns, showing uniform round-to-oval nuclei, inconspicuous nucleoli, and moderate cytoplasm without nuclear atypia, pleomorphism, or mitotic figures, confirming a benign cytological profile. A maturation gradient was noted, with smaller, less pigmented nevus cells deeper in the dermis, typical of benign melanocytic nevi. Melanin accumulation in superficial nevus cells contributed to the brown-to-black pigmentation. In the deep dermis, mature lamellar bone with well-defined trabeculae was observed, consistent with osteonevus of Nanta. Importantly, there was no epidermotropism, junctional activity, or atypical features, emphasizing the lesion’s benign nature. These findings collectively support the diagnosis of a benign melanocytic nevus with osseous metaplasia [Figure 3].
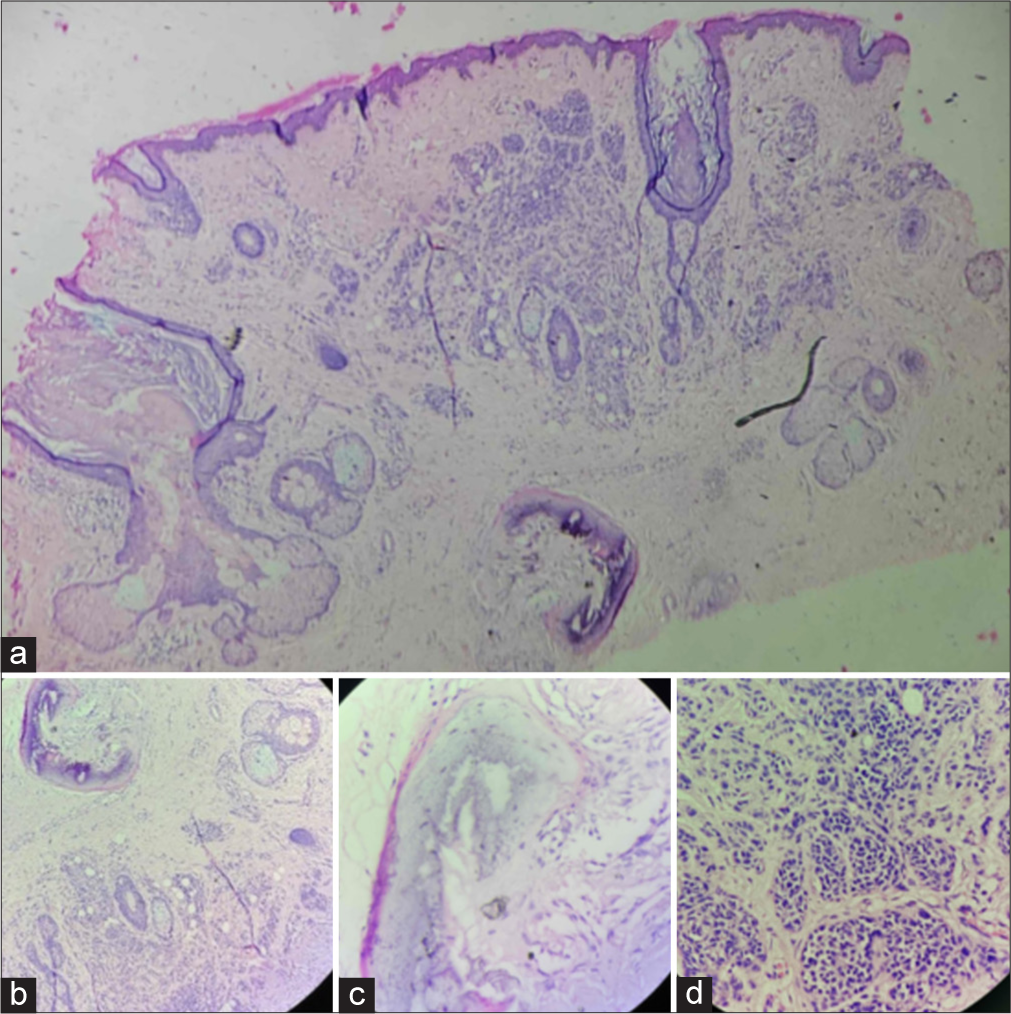
- (a-d) (a) Histopathological examination image shows ×4 magnification view of a dermal, symmetric benign melanocytic nevus with nests of nevus cells and lamellar bone formation. (b-d) Histopathological examination image shows ×10 magnification view (lower right corner) of a dermal, symmetric benign melanocytic nevus with nests of uniform nevus cells (lower left corner), maturation gradient, melanin pigmentation, and lamellar bone (lower center) in the deep dermis indicates osseous metaplasia.
DISCUSSION
Osteonevus of Nanta is a rare clinical entity characterized by bone formation within a melanocytic nevus, most commonly observed in the head-and-neck region with a female predilection.4 Its exact prevalence is not well defined, but it is considered a distinct but extremely rare variant of intradermal nevi.2,3
The pathophysiology of ossification in lesions is linked to disembrioplasia and metaplasia.2,3 Disembrioplasia suggests primitive mesenchymal cells, such as osteocytes, are present in the dermis where ectodermal and mesodermal structures coexist, promoting bone formation. Chronic inflammation or trauma, such as follicular distortion by melanocytes or trauma from hair removal, can cause follicular rupture and an inflammatory response, leading to metaplastic changes. In addition, interaction between nevus cells and surrounding mesenchymal tissue may trigger cell metaplasia, resulting in ossification.2 Studies also indicate a higher incidence of osteonevus in females, suggesting a role for estrogen in bone formation.2 Estrogen binds to receptors on osteoblasts, activating them and inhibiting bone resorption by osteoclasts, contributing to ossification. These factors collectively explain the development of osseous structures in benign lesions such as osteonevus of Nanta.
Dermoscopic evaluation is crucial for distinguishing osteonevus of Nanta from lesions such as calcinosis cutis, pilomatricomas, or cutaneous osteomas. Bone-like white structures and reticular pigment patterns aid in pre-operative identification, and in this case, the dermoscopic findings matched histopathology, revealing lamellar bone formation in the deep dermis. Other notable dermoscopic features include white crystalline clods, which correspond to underlying calcification or ossification, and telangiectatic vessels, indicating increased vascularity around the calcified areas, suggesting a reactive process. Peripheral blue-gray pigmentation may indicate melanin in the deeper dermis, typical of melanocytic nevi, while a brown-black pigmented network with a reticular pattern surrounding the central nodule points to a benign melanocytic nevus. These dermoscopic features assist in accurately diagnosing the lesion before surgical intervention.5
Histologically, osteonevus of Nanta demonstrates intradermal bone formation, typically accompanied by nevus cells arranged in a symmetric pattern.3,4 Management usually involves complete excision for diagnostic confirmation and cosmetic concerns, with an excellent prognosis and minimal risk of recurrence.5
The surgery ensured complete removal of the lesion, mitigating the risk of recurrence and future diagnostic ambiguity while also providing excellent cosmetic results, with the patient achieving a smooth, pigment-free skin surface [Figure 1b]. The incision healed uneventfully, and the patient reported high satisfaction during follow-up, highlighting the success of this definitive and patient-centered intervention.
CONCLUSION
Recognition of this rare entity is crucial for clinicians to prevent misdiagnosis and ensure proper treatment. The simplicity of the surgical procedure, along with the lesion’s superficial dermal location, facilitated its excision with minimal risk of complications. This reinforces the role of surgical intervention as the gold standard in the management of benign osseous lesions in the skin.
Authors’ Contributions
All the authors contributed equally to the manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Osteo-Nevus of Nanta (Osseous Metaplasia in an Intradermal Melanocytic Nevus): Case report of an uncommon phenomenon. Biosci Biotechnol Res Asia. 2011;8:435-8.
- [CrossRef] [Google Scholar]
- Ostéome sous-naevique (ostéo-naevus de Nanta) Bull Soc Fr Dermatol Syphiligr. 1963;70:873-7.
- [Google Scholar]
- Cutaneous osteomas: A clinical and histopathologic review. Arch Dermatol Res. 1977;260:121-35.
- [CrossRef] [PubMed] [Google Scholar]
- Osteomas of the skin revisited: A clinicopathologic review of 74 cases. Am J Dermatopathol. 2002;24:479-83.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of an osteonevus of Nanta. Int J Dermatol. 2014;53:e212-4.
- [CrossRef] [PubMed] [Google Scholar]






