Translate this page into:
Periareolar Augmentation Mastopexy: Finding the Aesthetic Level of Breast Lifting
Address for correspondence: Dr. Il Hwan Byun, Department of Plastic and Reconstructive Surgery, ID Hospital, 142 Dosandae-ro, Gangnam-gu, Seoul, South Korea. E-mail: byunmd@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Ptosis and volume atrophy of the breasts are common symptoms for various ages of women and may induce a considerable amount of stress in daily life. Periareolar augmentation mastopexy is an effective procedure for such conditions, and planning the new nipple position is very important.
Aim:
To provide a simple, straightforward planning and walkthrough of this operation in a journey to find the ideal level of breast lifting for natural upper fullness.
Materials and methods:
From January 2019 to December 2021, a total of 193 patients with volume deflation and ptosis of the breast received periareolar augmentation mastopexy in our institute. We retrospectively reviewed data on demographics, surgical procedures, outcomes, and complications.
Results:
All operations were done with periareolar incisions, and the mean follow-up period was 29.48 ± 9.11 months. The Likert scale of outcome satisfaction scored 9.02 ± 0.61. Complications were minimal, and no symmastia or bottoming out occurred.
Conclusion:
We present our basic strategies of periareolar augmentation mastopexy with a slight modification of the design. We believe that lifting the nipple to 3–4 cm above the inframammary fold (IMF) (making the top of the areola about 5–6 cm above the IMF) yields satisfactory aesthetic results.
Keywords
Breast augmentation
cosmetic breast surgery
periareolar mastopexy
INTRODUCTION
Ptosis and volume atrophy of the breasts are common symptoms for various ages of women and may induce a considerable amount of stress in daily life. The breast is doubtlessly a very important part of the upper body as the symbol of female sexuality as well as maternity.[12] Such changes in the breast often come after multiple pregnancies, breastfeeding, or significant weight loss.[34] Breast surgery alleviates many conditions such as small size, asymmetry, hypoplasia, ptosis, and chest wall anomalies.[567] It is the most common cosmetic surgery in the United States and is growing popular around the world.[8] For a woman with both volume decrease and ptosis of the breasts, not only augmentation but also mastopexy is required.
Cooper’s ligaments play an essential role in maintaining the breast shape, by connecting the mammary gland to the skin and pectoralis major fascia.[9] The structures may loosen as a woman ages, gives births, breastfeeds, or loses weight.[410] The Regnault classification is often used to evaluate breast ptosis, where the grade depends on the position of the nipple in relation to the inframammary fold (IMF).[11] Regardless of the severity and grade, many women with decreased volume and skin sagging seek for rejuvenation of the breast to relieve stress and boost self-esteem. However, breast augmentation and mastopexy are sometimes conflicting, bringing many challenges and discussions for surgeons.[1213141516] The combination of two procedures makes the prediction of results more difficult compared with a single operation.
Gonzalez-Ulloa[17] first described augmentation mastopexy in 1960, and operating breast ptosis in combination with an implant has been widely applied worldwide. The goals of augmentation mastopexy often include elevation of the nipple-areolar complex, elevation of the mound, conversion of a ptotic breast to a conical one, volume increase, and improvement of symmetry.[12] The surgeon must remove enough skin with the mastopexy to create a tight appropriate envelope, yet reserve enough laxity for implant placement and volume increase. The more the breast tissue that hangs under the IMF, the more inadequately the implant will fill out the breast without adequate skin elevation.[18] There are various methods of augmentation mastopexy, such as periareolar, circumvertical, and inverted T. We utilized periareolar technique the most, because most patients are concerned for minimal scars.
As with other cosmetic procedures, surgical design and simulation are very important for desired results. For periareolar augmentation mastopexy, the new position of the nipple is the crucial part of the planning. There are several methods of finding the new nipple position, but we tried to keep it simple and consider the relation to IMF the most important. Many previous studies proposed designs of the new nipple to be located at the same level or just cephalad to the IMF.[1819] Although it may differ by time and ethnicity, we believe that a higher nipple position brings an aesthetic contour and enhances the effects of breast lifting. The reason for modifying our design from traditional position was because in many previous cases where we adjusted the new nipple position near the IMF, as time goes by and skin loosens, the new nipple often was slightly lower than the maximal projection of the breast. Also, although it may differ by individuals, some patients often asked if their nipple could not be lifted more. Here, we provide a simple, straightforward planning and walkthrough of periareolar augmentation mastopexy, in a journey to find the ideal level of breast lifting for natural upper fullness.
MATERIALS AND METHODS
From January 2019 to December 2021, a total of 193 patients with volume deflation and ptosis of the breast received periareolar augmentation mastopexy in our institute. We retrospectively reviewed data on demographics, surgical procedures, outcomes, and complications. Patients who received circumvertical or inverted T mastopexy were not included in this study. Outcomes were measured by a Likert scale from 0 to 10 (0 = poor result; 10 = very satisfied result). The study was performed in accordance with the Declaration of Helsinki.
Thorough history taking was done including comorbidities, allergies, surgical history, drinking, and smoking history before the surgery. Drinking and smoking cessation were strongly recommended for 1 month before and after the operation. The width, height, and projection of the breast were measured. Preoperative photographs from six were obtained. After a thorough consultation, the implant company and sizes were selected for desired results. We routinely performed ultrasound examination to screen any suspicious lesions.
For surgical planning, the new nipple location was considered the most important factor. First, we marked the meridian of each breast regardless of the nipple position. Then, the IMF was marked for each breast, and a horizontal line was drawn across the chest. We then marked a point about 5–6 cm above that line in the midline. A small horizontal line was marked on each breast at the level of the previously mentioned point, meeting the previously marked meridian of each breast. This became the apex of the periareolar incision design. Considering the new areolar diameter to be less than 4 cm, the center of the nipple would be located about 3–4 cm higher than the IMF. The upper margin of the areola was pinched and lifted up for simulation of the new position. In cases of tall patients above 170 cm (5.58 ft) with a long upper body and patients with a low breast profile, the new nipple position may be even higher than 4 cm above the IMF. But we made sure that the nipple would not be visible when wearing a bra. The medial and lateral points of the incision were designed by gently shifting the breast to the left and right, trying not to be too wide. The shape of the design was not perfectly circular, but rather oval with the lower portion wider than the upper portion, as shown in Figure 1. As mentioned in previous literature, asymmetric excision of the skin was used to adjust breast asymmetry.[20]
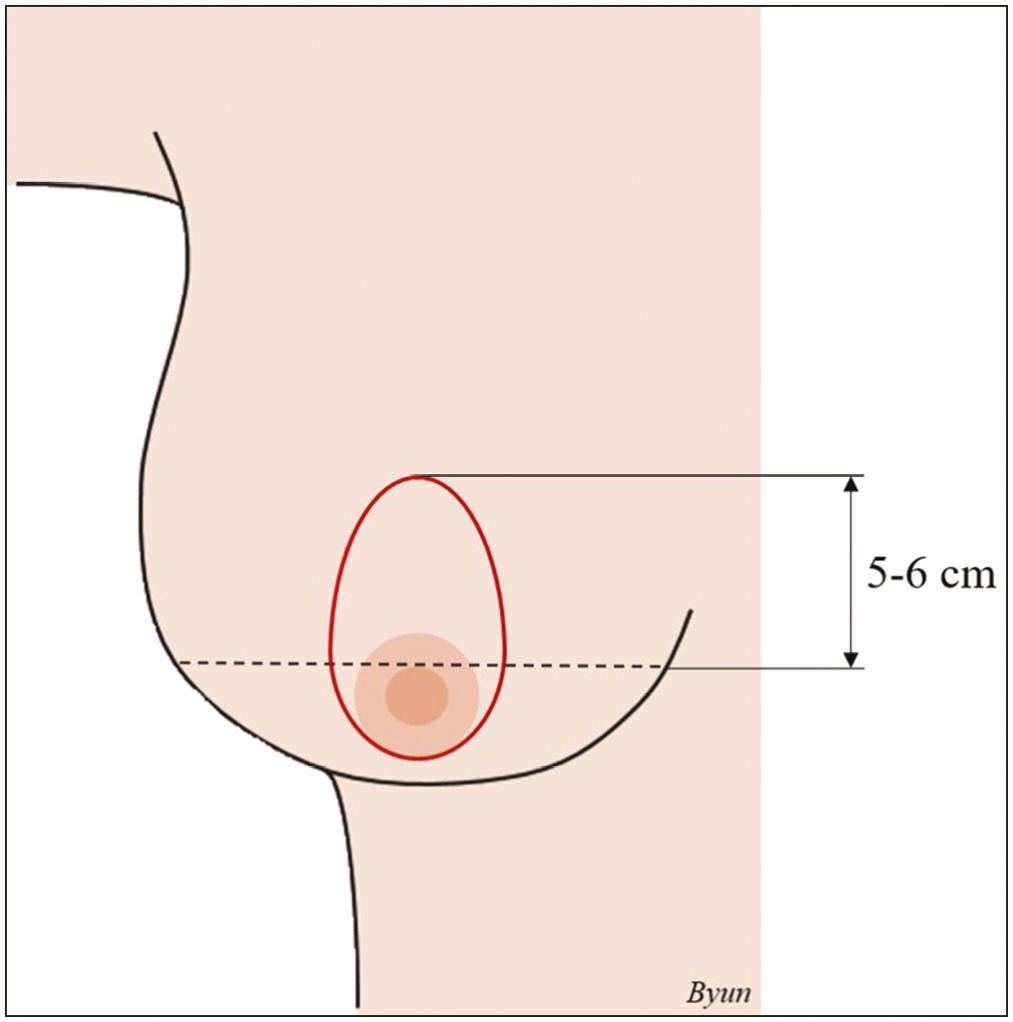
- Surgical design of periareolar augmentation mastopexy. The upper margin of the relocated areola is 5–6 cm above the inframammary fold
All operations were performed under general anesthesia. After the areola was evenly stretched with two hands, a new 38-mm areola was marked with an areola marker. Local anesthetic of 1% lidocaine mixed with 1: 100,000 epinephrine solution was injected along the incision lines. Precise incisions of the new areola and outer mastopexy design were done, and the skin between the two incisions was de-epithelized. Within the area of the raw surface, a 3-cm incision near the caudal part was created, and subfascial pocket dissection was done under direct vision. Sometimes, dual-plane dissection was utilized in very thin patients without much breast tissue. Precise dissection was done to minimize remnant dead space, and temporary intraoperative sizers were used to check the margins. Pocket irrigation with antibiotics mixed saline was done before the insertion of the implant. After the insertion of the implant with “no touch” technique, the glandular tissues were sutured with absorbable 3-0 sutures. Then, the dermis near the margin of the outer circle was slightly dissected, and a purse-string suture was performed with 3-0 polypropylene suture to close the new areola. The diameter of the new areola was usually measured within 4 cm, considering the widening in the future. Finally, the areolar skin closure was done with absorbable 4-0 and nylon 5-0 sutures. No drain was inserted in any cases.
Postoperatively, patients were given a surgical brassiere and oral antibiotics. At follow-up visits, clinical examination, photography, ultrasound, and Likert scale satisfaction survey were done to assess the results. Descriptive statistics are presented as the mean with standard deviation or as numbers and percentages.
RESULTS
All of the 193 patients included in this study were females with the mean age of 43.19 ± 6.54 and a mean body mass index of 23.33 ± 3.71. All operations were done with periareolar incisions. The mean implant volume was 261.43 ± 65.75 cc, and the mean follow-up period was 29.48 ± 9.11 months. All of our surgeries were performed with round smooth implants. Some were microtextured implants, but they are categorized as smooth implants according to International Organization for Standardization standards. The Likert scale of outcome satisfaction scored 9.02 ± 0.61. Other demographic data and surgical details are listed in Table 1.
| Number of patients | 193 (386 breasts) |
|---|---|
| Age (years) | 43.19 ± 6.54 |
| Body mass index | 23.33 ± 3.71 |
| Comorbidities | |
| Hypertension | 6 (3.10%) |
| Diabetes | 1 (0.05%) |
| Smoking | 14 (7.25%) |
| Implant volume (cc) | 261.43 ± 65.75 |
| Use of drain | 0 (0%) |
| Likert scale (0–10)a | 9.02 ± 0.61 |
| Follow-up period (months) | 29.48 ± 9.11 |
a0 = poor result; 10 = very satisfied result
There were few complications following our operations. They included hematoma, capsular contracture (defined as Baker scale grades III and IV), minor wound problem, and hypertrophic scar. There was one (0.52%) hematoma case. The hematoma was surgically drained in the operation room, and the patient recovered without any sequela. There were two (1.04%) cases of capsular contracture (grade III), and successful surgical revision was done with total capsulectomy. Seven patients (3.63%) presented with minor wound problems, and minimal debridement and nylon sutures were done in the outpatient clinic. Three patients (1.55%) developed hypertrophic scars, and triamcinolone injection was done for two patients, and scar revision was done for one patient. No symmastia occurred, and complication data are listed in Table 2. Examples of pre- and postoperative photos are shown in Figures 2 and 3.
| Number of patients | 193 |
|---|---|
| Hematoma | 1 (0.52%) |
| Seroma | 0 (0%) |
| Infection | 0 (0%) |
| Capsular contracture (grade III–IV) | 2 (1.04%) |
| Implant rupture | 0 (0%) |
| Minor wound problem | 7 (3.63%) |
| Hypertrophic scar | 3 (1.55%) |
| Symmastia | 0 (0%) |
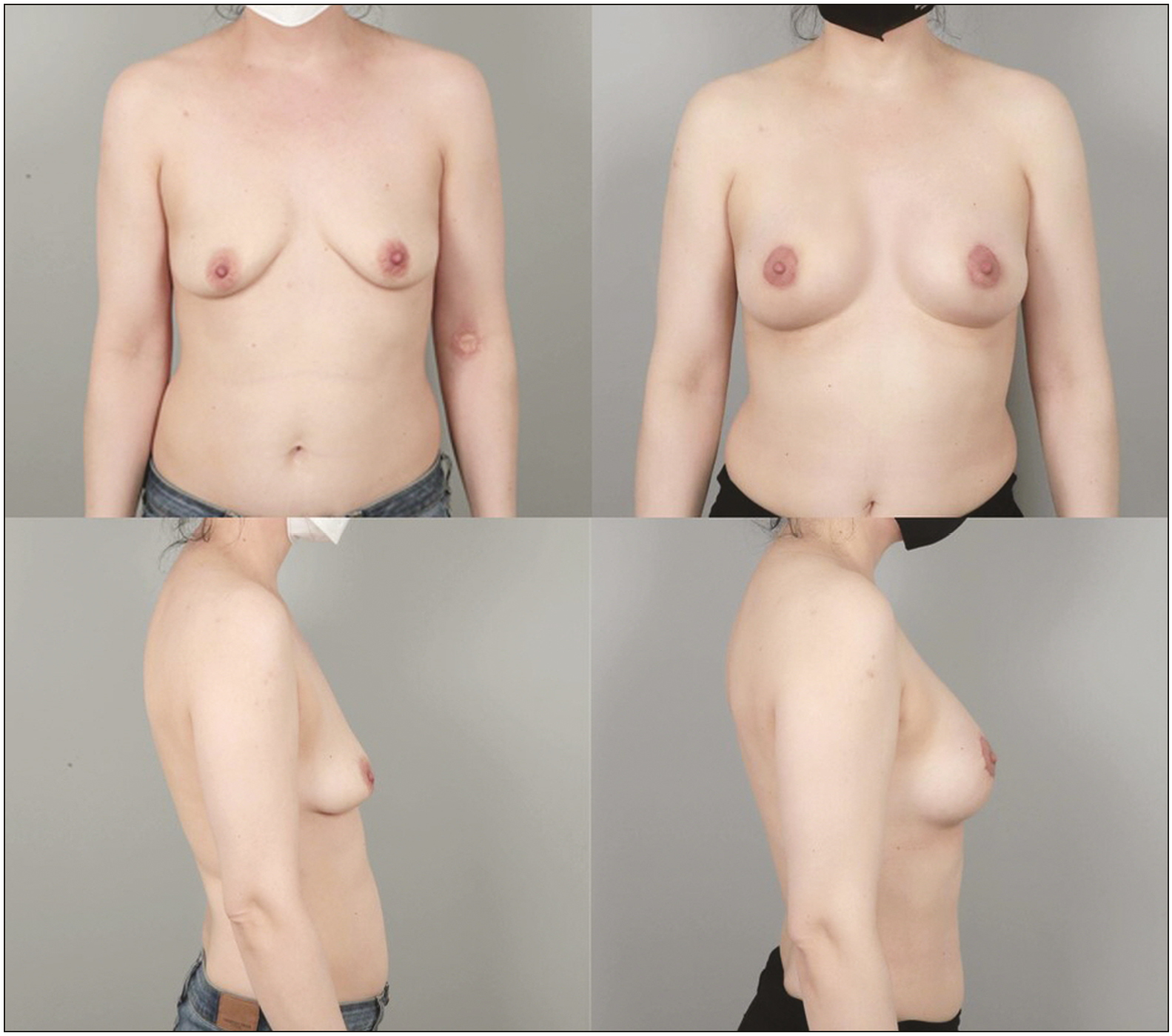
- Preoperative front and lateral views (left above and below) and postoperative front and lateral views (right above and below) of a 39-year-old female who received periareolar augmentation mastopexy with 215 cc implants
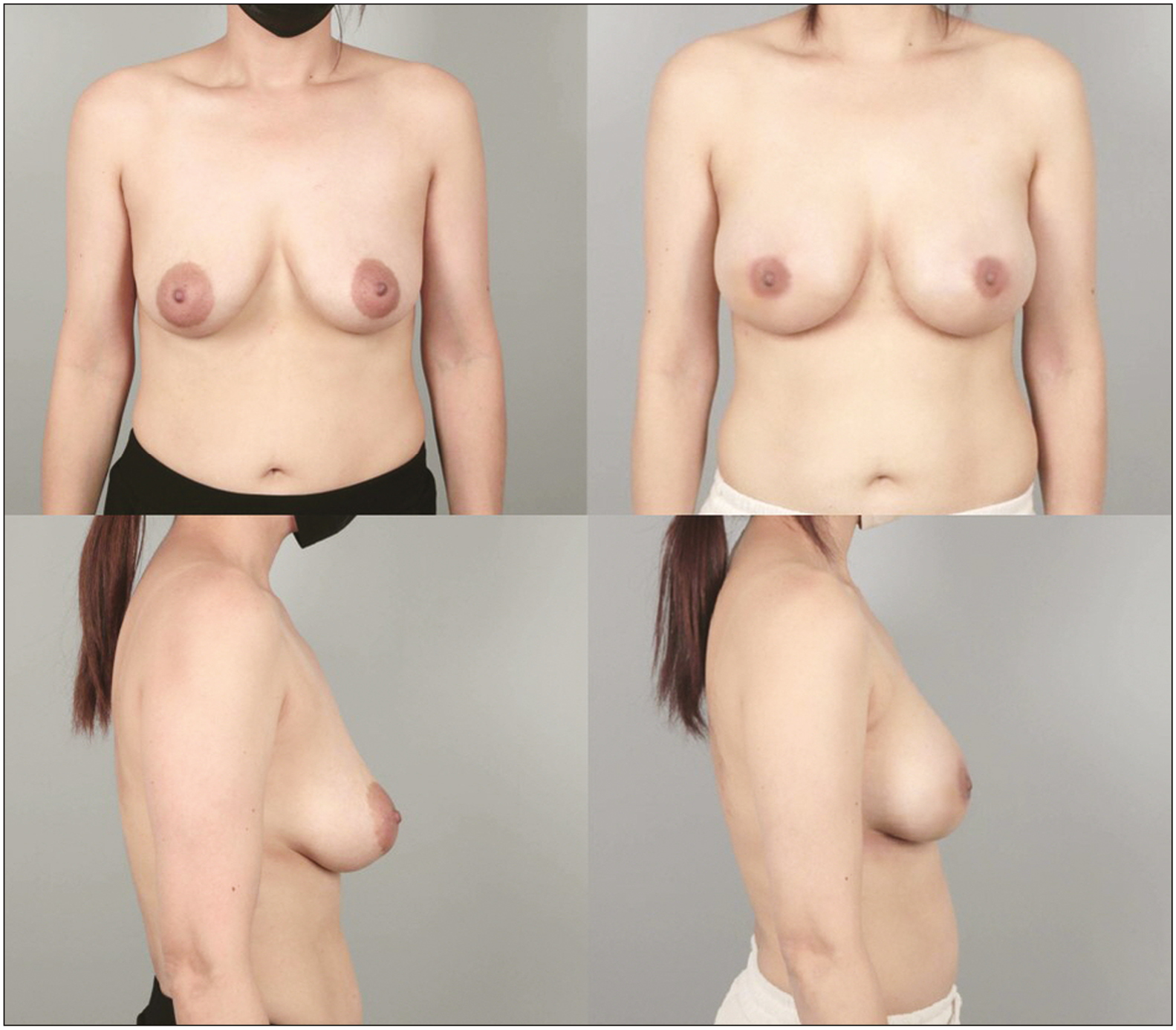
- Preoperative front and lateral views (left above and below) and postoperative front and lateral views (right above and below) of a 46-year-old female who received periareolar augmentation mastopexy with 295 cc implants
DISCUSSION
Both volume decrease of the upper pole and ptosis of the breast are common and dynamic processes in many women. Many factors contribute to this change such as pregnancy, lactation, and weight loss.[4] Usually, Cooper ligaments become loose, and the skin gets lax and stretched. Postpartum atrophy and massive weight loss bring volume loss and failure to support the firmness of the breast. The gradually stretched mammary gland results in the lengthening of the glandular tissue and skin, especially on the upper pole of the breast. Thick gland shifts downward when standing.[9] Such changes in breast shape often induce stress, and some people have exaggerated self-image and frustration.[2122] Emotional stress may push women to seek cosmetic surgery even in the absence of functional limitations.[2324] As stated in our Likert scale results, augmentation mastopexy brought great satisfaction to such patients and boosted self-esteem. There are several types of mastopexy including periareolar, vertical, and inverted T as described in previous literature.[25] Although vertical mastopexy is widely used in many countries, we utilized periareolar incision the most to avoid the obvious vertical scar, which may not be well accepted in many cultures.[9] Even in grade 3 ptosis patients, simultaneous use of an implant makes the periareolar technique possible to yield good results. Yet, the large difference between the two circumferences may make periareolar scar irregular and unaesthetic. Thus, we recommend this to patients with grade 1 or 2, and patients with grade 3 who do not want vertical or inverted T scars. Patients with large areolas and elastic skin are known to be ideal for this technique because the resected skin will not flatten the overall breast shape.[3]
Preoperative planning and design are very important for augmentation mastopexy because the two procedures contradict each other, possibly increasing the risk of complications.[14] One of the most important decisions was finding the aesthetic level of the new nipple position. In many previous studies, the new nipple was usually depicted at the same level or very close to the IMF or was determined by the distance from the sternal notch.[318,19] Because every patient’s original nipple position is different when she was young, we thought the harmony of the arrangement between the nipple and the IMF is more important than the sternal notch. We also believed that an aesthetic level of the nipple is a few centimeters above the IMF, a bit more cephalad to the maximal projection of the breast. Of course, it is crucial to pinch the upper areola and simulate the new position, and we usually designed the upper margin of the areola to be 6 cm above the IMF. When we first started this design a few years ago, we did worry about possible pseudoptosis appearance or bottoming out of the implant. But rather contrary, we did not experience any bottoming-out cases, and patients were more pleased with the result. We believe that using implants of not too big sizes led to such results.
The recommended sizes of the implant were usually smaller than those used in primary augmentation cases. Many augmentation mastopexy candidates often had more glandular tissue than primary augmentation patients, and naturally filling the upper pole was a more important goal than obtaining a large volume. Also, we believe that inserting an adequate-sized implant than the maximum volume possible lessens the periareolar tension and leaves better scars.
Appropriate surgical planning and patient selection lead to stable satisfactory results with minimal complications. As noted in Table 2, our complication rate was low compared with previous literature. Previous study reports that the complication rate of periareolar surgery can be up to 40%.[2627282930313233] Possible complications include hypertrophic scars, scar widening, areolar distortion, breast flattening, and wound problems.[2728,3435] We believe that choosing an appropriate-sized implant and making a vertically long oval periareolar incision lessened the tension to minimize complications.
Although our follow-up period of 29.48 ± 9.11 months is not a short time, longer period of evaluation will strengthen the results. We often utilized subfascial plane for implant insertion to maximize breast elevation and to prevent double bubble deformity or flattening of the breast. A pinch test was always performed, and a dual plane was applied if the tissue was too thin. Even with mostly subfascial dissection, our overall contracture rate was lower than many previous data.[3637] We tried to shorten the operation time as possible and followed most of the 14-point plan proposed by Adams et al.[38] to minimize complications.
CONCLUSION
As with facelift and other antiaging surgeries, periareolar augmentation mastopexy is an effective operation that can benefit many women with great satisfaction and small complications. We believe that lifting the nipple to 3–4 cm above the IMF (making the top of the areola about 5–6 cm above the IMF) yields satisfactory aesthetic results. One may say this is just a few centimeters difference, but as the famous architect Ludwig Mies van der Rohe said, “God is in the details.”
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- Simultaneous augmentation mammoplasty and vacuum-assisted breast biopsy for enhanced cosmesis and efficacy. Aesthetic Plast Surg. 2020;44:2041-7.
- [Google Scholar]
- Double triangle suture technique for inverted nipple correction while preserving the lactiferous ducts. Aesthetic Plast Surg. 2022;15:371-4.
- [Google Scholar]
- Simultaneous augmentation and periareolar mastopexy: Selecting the correct implant. Aesthetic Plast Surg. 2010;34:33-9; discussion 40.
- [Google Scholar]
- Breast augmentation combining fat injection and breast implants in patients with atrophied breasts. Ann Plast Surg. 2017;78:623-8.
- [Google Scholar]
- Endoscopic transaxillary versus inframammary approaches for breast augmentation using shaped implants: A matched case-control study. Aesthetic Plast Surg. 2019;43:563-8.
- [Google Scholar]
- Basic strategies of augmentation mammoplasty in patients with tendencies of pectus excavatum and carinatum. Aesthetic Plast Surg. 2022;47:54-60.
- [Google Scholar]
- Current trends in breast augmentation: An international analysis. Aesthet Surg J. 2018;38:133-48.
- [Google Scholar]
- Simultaneous mastopexy via areola excision to correct mild and moderate breast ptosis. Aesthetic Plast Surg. 2021;45:948-55.
- [Google Scholar]
- Augmentation mastopexy with a dermal encapsulated round or anatomic autoprosthesis. Aesthetic Plast Surg. 2018;42:88-97.
- [Google Scholar]
- Vertical mastopexy with expansion augmentation. Aesthetic Plast Surg. 2003;27:13-9.
- [Google Scholar]
- Unsatisfactory results of periareolar mastopexy with or without augmentation and reduction mammoplasty: Enlarged areola with flattened nipple. Aesthetic Plast Surg. 2001;25:286-9.
- [Google Scholar]
- Mastopexy preferences: A survey of board-certified plastic surgeons. Plast Reconstr Surg. 2006;118:1631-8.
- [Google Scholar]
- One-stage augmentation combined with mastopexy: Aesthetic results and patient satisfaction. Aesthetic Plast Surg. 2004;28:259-67.
- [Google Scholar]
- Correction of hypotrophy of the breast by means of exogenous material. Plast Reconstr Surg Transplant Bull. 1960;25:15-26.
- [Google Scholar]
- Simultaneous breast augmentation with periareolar mastopexy. Semin Plast Surg. 2004;18:189-201.
- [Google Scholar]
- Quality of life of patients who have undergone the minimally invasive repair of pectus carinatum. Eur J Cardiothorac Surg. 2013;43:122-6.
- [Google Scholar]
- Self- and social perception of physical appearance in chest wall deformity. Body Image. 2012;9:246-52.
- [Google Scholar]
- An evidence-based approach to management of pectus excavatum and carinatum. Ann Plast Surg. 2019;82:352-8.
- [Google Scholar]
- Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: A control group comparison of psychological characteristics prior to surgical correction. Eur J Cardiothorac Surg. 2011;40:1138-45.
- [Google Scholar]
- “Zigzag” wavy-line periareolar incision. Plast Reconstr Surg. 2002;110:1778-83; discussion 1784.
- [Google Scholar]
- Reduction mammaplasty and correction of ptosis: Dermal bra technique. Plast Reconstr Surg. 2003;111:1122-30.
- [Google Scholar]
- Periareolar mammaplasty: Double skin technique with application of polyglactine or mixed mesh. Plast Reconstr Surg. 1996;97:959-68.
- [Google Scholar]
- A new periareolar mammaplasty: The “round block” technique. Aesthetic Plast Surg. 1990;14:93-100.
- [Google Scholar]
- Circumareolar dermo-glandular plication: A new concept for correction of breast ptosis. Aesthetic Plast Surg. 2001;25:404-20.
- [Google Scholar]
- The “donut” mastopexy: Indications and complications. Plast Reconstr Surg. 1980;65:34-8.
- [Google Scholar]
- Concentric mastopexy revisited. Plast Reconstr Surg. 2001;107:1294-9; discussion 1300.
- [Google Scholar]
- A new mastopexy operation for mild or moderate breast ptosis. Plast Reconstr Surg. 1976;57:687-91.
- [Google Scholar]
- Nine-year core study data for sientra’s FDA-approved round and shaped implants with high-strength cohesive silicone gel. Aesthet Surg J. 2016;36:404-16.
- [Google Scholar]
- Natrelle round silicone breast implants: Core study results at 10 years. Plast Reconstr Surg. 2014;133:1354-61.
- [Google Scholar]
- Macrotextured breast implants with defined s.jpg to minimize bacterial contamination around the device: Experience in 42,000 implants. Plast Reconstr Surg. 2017;140:427-31.
- [Google Scholar]






