Translate this page into:
Platelet-rich plasma and topical minoxidil 5% in the treatment of severe alopecia areata: Report of two cases
*Corresponding author: Lidiya Nikolova Todorova, Department of Dermatology and Venereology, Medical University of Plovdiv, Plovdiv, Bulgaria, 15A Vasil Aprilov blvd. lidiatodorova@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Todorova LN. Platelet-rich plasma and topical minoxidil 5% in the treatment of severe alopecia areata: Report of two cases. J Cutan Aesthet Surg. doi: 10.25259/JCAS_42_2024
Abstract
Alopecia areata (AA) is an autoimmune non-scarring hair loss that can affect any hair-baring body area. Corticosteroids are considered first-line treatment, but their long-term use may lead to undesirable side effects. Platelet-rich plasma (PRP) is an autologous product, which includes concentrated platelets that secrete growth factors stimulating hair follicle proliferation. Topical minoxidil has been used for mild cases of AA and other types of alopecia. We report two cases of severe multifocal AA, treated successfully with the combination of topical minoxidil 5% and intralesional PRP. PRP was injected once monthly for a total of six visits. Patients were advised to use 5% topical minoxidil twice daily. Trichoscopy was performed and evaluation of the severity of hair loss was done with Severity of Alopecia Tool (SALT). One month after the final PRP procedure, patients showed significant hair regrowth. Further controlled trials with more subjects are needed to validate the reported results.
Keywords
Alopecia
Alopecia areata
Hair loss
Minoxidil
Platelet-rich plasma
INTRODUCTION
Alopecia areata (AA) is an autoimmune non-scarring hair loss of the scalp or the body with an incidence rate of 0.1–0.2%. AA manifests as single or multiple well-defined round bald patches of different size. If multiple, the patches may coalesce forming a reticular pattern, known as multifocal AA. The condition may also affect the hair follicles of the body.1 The course of the disease is unpredictable and spontaneous remissions occur in 34–50% of patients within a year.2 Traditional treatments show limited efficacy and may lead to undesirable side effects or relapses when discontinued.3 Platelet-rich plasma (PRP) includes concentrated platelets, 4–7 times above baseline, that secrete growth factors and cytokines. They stimulate hair follicle proliferation, differentiation, and neoangiogenesis.3-6 Topical minoxidil is used to promote hair growth, but its exact mechanism of action is still not fully understood.7 We present two cases of severe multifocal AA, which were successfully treated with combination of monthly intralesional applications of PRP and 5% topical minoxidil.
Materials and methods
Standard laboratory tests
Complete blood count, electrolytes, serum creatinine, and liver function tests were done at first visit. PRP was prepared by the double-spin methodology: Blood was drawn in six 3, 2% sodium citrate 5 mL tubes, centrifuged for 5 min at 500 rpm. The bottom one-third layer of plasma (above the red blood cells layer) was transferred into two 5 mL blood collection tubes which were centrifuged at 1300 rpm for 7 min. The obtained 6–8 mL PRP was injected in the scalp through multiple intradermal injections. The procedure was performed once monthly for a total of six sessions. Patients were advised to use 5% topical minoxidil twice daily during the treatment period. Follow-up (FU) was done 1 month after the last PRP session. Trichoscopy was performed with Dino-Lite Edge Digital Microscope AM7915MZT (R7), ×70 magnification at first visit, (base line, BL), and at FU. Evaluation of the severity of hair loss was done with Severity of Alopecia Tool (SALT score).
CASE REPORT
Case 1
A 38-year-old female patient presented with the first episode of hair loss at multiple sites over the capillitium leading to severe alopecia. The duration of the hair loss was 12 months. She had not been treated previously and refused corticosteroid (CS) treatment due to corticophobia. She had no associated conditions. On clinical examination, there were multiple well-defined coalescing bald areas, forming a reticular pattern. The skin in the bald patches was of normal color, and there were visible vellus hairs and black dots. Standard laboratory tests were within the norms. At BL, we evaluated SALT 65 and trichoscopy depicted black dots, exclamation marks, and vellus hairs [Figure 1a-c]. Due to the reported corticophobia, PRP and 5% topical minoxidil was the treatment of choice. At FU, the patient had SALT 4, 5. Trichoscopy at FU showed upright regrowing hairs, pigmented terminal hairs, and increased hair shaft thickness. Three months after the last PRP application, the patient had SALT 0 [Figure 2a-c], that is, complete hair regrowth.
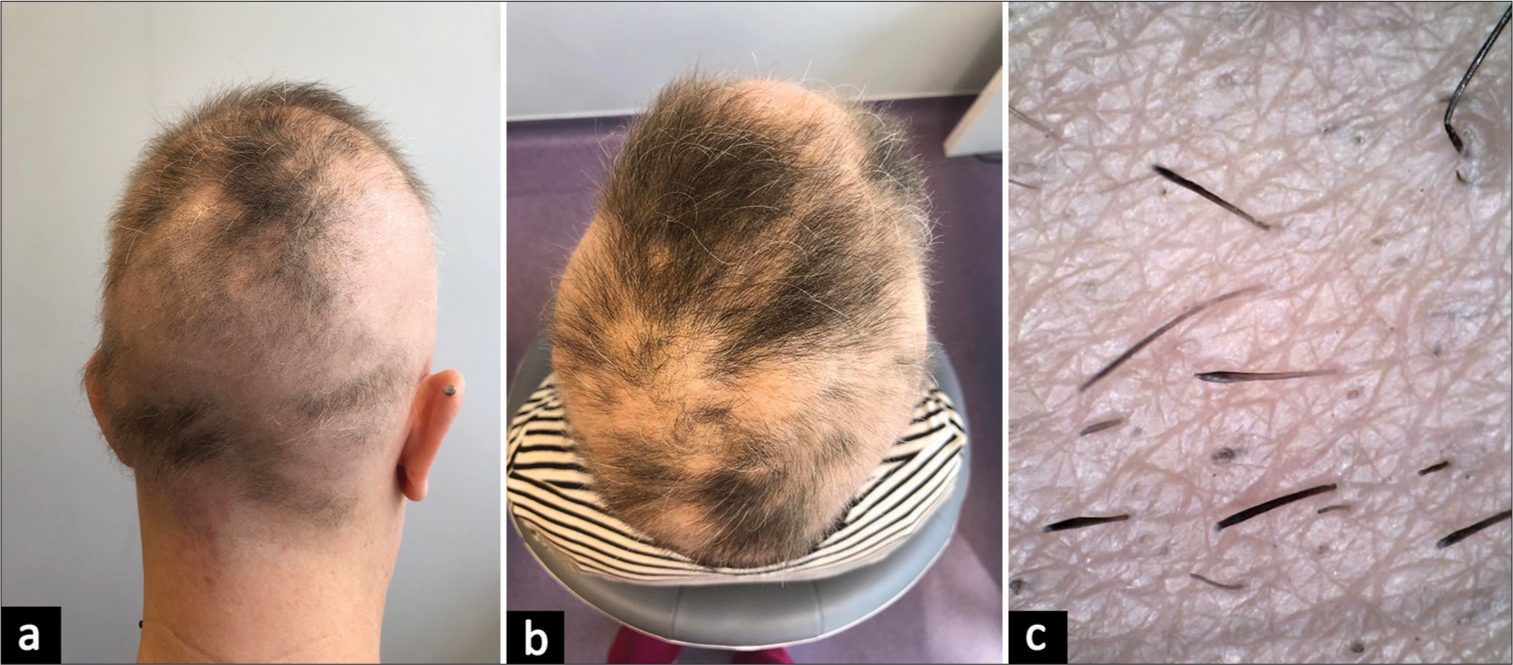
- (a and b) Case 1 at baseline, severity of alopecia tool 65. (c) Trichoscopy of case 1 at base line: Black dots, exclamation mark hairs.
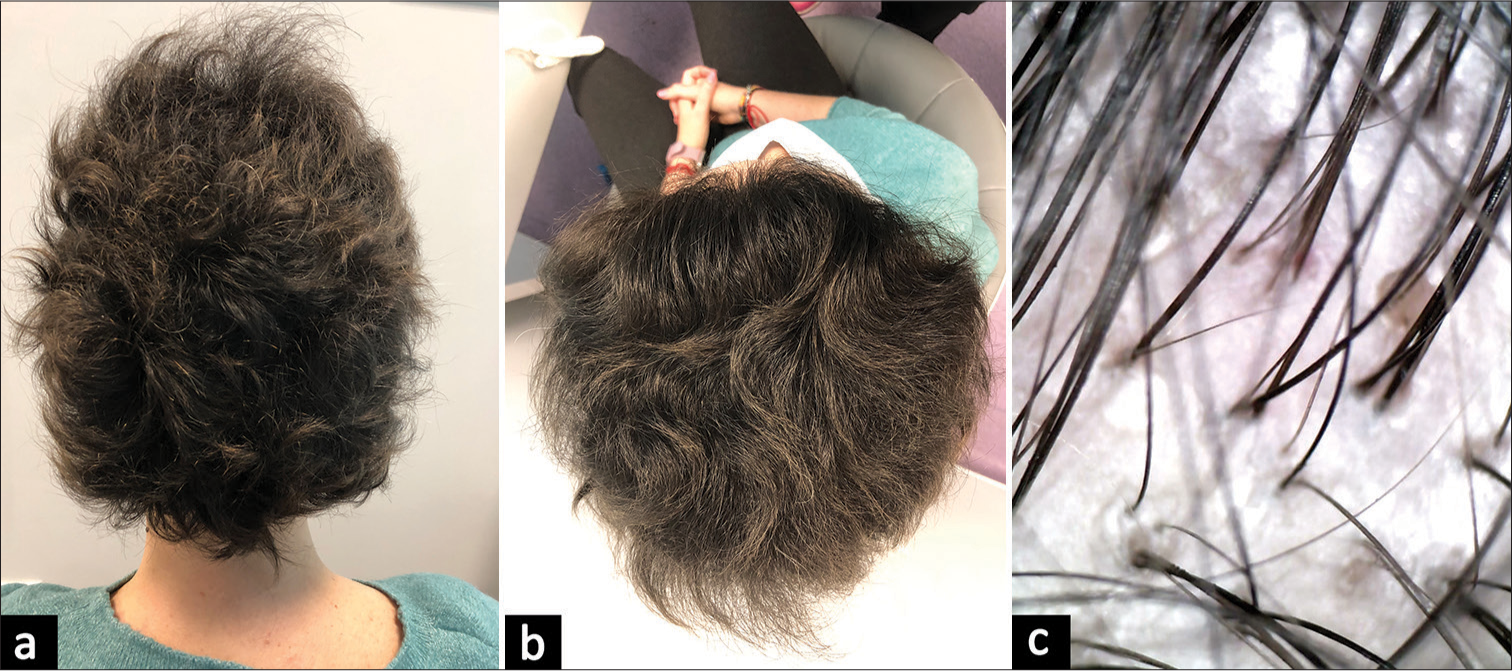
- (a and b) Case 1: 3 months after the last platelet-rich plasma application, severity of alopecia tool 0. (c) Trichoscopy of case 1 at follow-up: Upright regrowing hairs, pigmented terminal hairs, increased hair shaft thickness.
Case 2
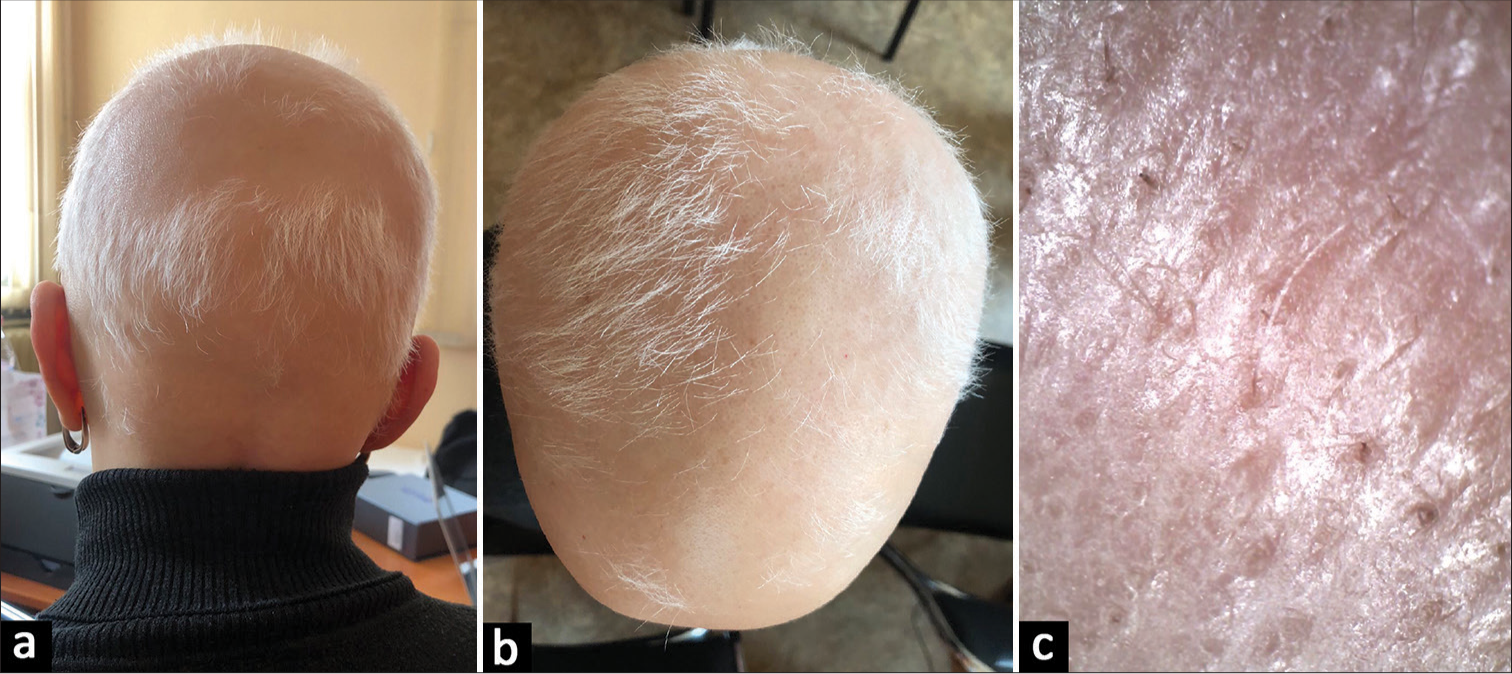
A 49-year-old female presented with recurrent scalp hair loss of reticular pattern with duration of 6 months, and no associated comorbidities. The skin in the bald patches was of ivory color and included a minimal amount of vellus hairs. Standard laboratory tests were within the norms. Trichoscopy showed yellow dots, black dots, broken hairs, and vellus hairs. At first visit, SALT was 82% [Figure 3a-c]. The patient refused CS treatment and was offered the aforementioned therapeutic approach. At FU, the patient had estimated SALT 19 and trichoscopy showed upright regrowing hairs and terminal hairs [Figure 4a-c].
- (a and b) Case 2 at baseline, severity of alopecia tool 82. (c) Trichoscopy of case 2 at base line: Yellow dots, black dots, broken hairs, and vellus hairs.

- (a and b) Case 2 at follow-up, severity of alopecia tool 19. (c) Trichoscopy of case 2 at follow-up: Upright regrowing hairs, terminal hairs.
DISCUSSION
The presented cases show that the combination of intralesional PRP and topical minoxidil leads to significant improvement in hair restoration in patients with severe multifocal AA. The non-scarring hair loss of AA is connected with the CD4+ and CD8+ T-lymphocytes, which violate the immune privilege of the anagen hair follicle.1 The diagnosis and activity of AA are based on the typical clinical manifestation and trichoscopy. Trichoscopic findings of active hair loss are black dots, broken hairs, exclamation mark hairs, and tapered hairs. Yellow dots and short vellus hairs are markers for chronic cases. Hair regrowth is associated with thicker and more pigmented vellus hairs, upright regrowing hairs, and pigtail hairs.8
Various therapeutic modalities have been used for AA, showing limited efficacy and leading to undesirable side effects. CSs in different forms and ways of administration are the most common treatment of use. Potent topical CS under occlusion is the preferred method. However, they show limited efficacy in severe AA. Triamcinolone acetonide is considered the drug of choice in mild and moderate AA as well as AA of the face. The most common side effects of the topical and intralesional CS treatment are folliculitis, telangiectasia, and atrophy.2,9 An alternative treatment approach for hair loss is the use of PRP. PRP includes concentrated platelets, 4–7 times above baseline values, that secrete growth factors and cytokines, including: Platelet-derived growth factor, vascular endothelial growth factor, transforming growth factor, fibroblast growth factor, connective tissue growth factor, epidermal growth factor, and insulin-like growth factor. They stimulate the anagen phase of the hair follicle, neovascularization, and development of adnexal structures.4-6 Full hair regrowth was observed in some studies exploring PRP effectiveness in patients with AA.6,9 Topical minoxidil has been considered of no benefit for patients with severe AA. It is usually recommended for mild AA until cosmetically acceptable regrowth is evident. The continuous use of minoxidil may lead to undesirable headache, edema, dermatitis, and hypertrichosis. They are reversible with the cessation of the treatment. Reports available compare PRP and local minoxidil, both leading fully pigmented hair regrowth in patchy AA, and reducing short vellus hair, broken hairs, and yellow dots.10
CONCLUSION
The autologous PRP and topical minoxidil are both treatment alternatives for AA. However, the combination of both therapeutic approaches for AA has not been explored yet. The presented clinical cases confirm that this combination shows effective results in patients with severe multifocal AA and could be applied as an effective treatment alternative. Further controlled trials with more subjects are needed to validate the reported results.
Authors’ contributions
The author confirms sole responsibility for the following: data collection, analysis and interpretation of results, and manuscript preparation.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Epidemiology and burden of alopecia areata: A systematic review. Clin Cosmet Investig Dermatol. 2015;8:397-403.
- [CrossRef] [PubMed] [Google Scholar]
- Alopecia areata: A long-term follow-up study of 104 patients. J Eur Acad Dermatol Venereol. 2019;33:1602-9.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of alopecia areata. J Investig Dermatol Symp Proc. 2013;16:S13-5.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous platelet-rich plasma: A potential therapeutic tool for promoting hair growth. Dermatol Surg. 2012;38:1040-6.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-rich plasma in the treatment of alopecia areata: A review. J Investig Dermatol Symp Proc. 2020;20:S45-9.
- [CrossRef] [PubMed] [Google Scholar]
- Role of platelet-rich plasma in chronic alopecia areata: Our centre experience. Indian J Plast Surg. 2015;48:57-9.
- [CrossRef] [PubMed] [Google Scholar]
- Topical minoxidil in the treatment of alopecia areata. Br Med J (Clin Res Ed). 1983;287:1015-7.
- [CrossRef] [PubMed] [Google Scholar]
- Trichoscopy of alopecia areata: An update. J Dermatol. 2018;45:692-700.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, double-blind, placebo-and active-controlled, half-head study to evaluate the effects of platelet-rich plasma on alopecia areata. Br J Dermatol. 2013;169:690-4.
- [CrossRef] [PubMed] [Google Scholar]
- Platelets rich plasma versus minoxidil 5% in treatment of alopecia areata: A trichoscopic evaluation. Dermatol Ther. 2017;30:1-6.
- [CrossRef] [PubMed] [Google Scholar]







