Translate this page into:
Platelet-Rich Plasma with Microneedling in Androgenetic Alopecia: Study of Efficacy of the Treatment and the Number of Sessions Required
Address for correspondence: Dr Vani Yepuri, Venkat Center for Skin and Plastic Surgery, No. 3437, 7th Main Road, 1st G Cross Road, Subbanna Garden, Vijayanagar, Bengaluru 560040, Karnataka, India. E-mail: yepuri.vani@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Platelet-rich plasma (PRP) is a simple and safe procedure, which has been used for soft tissue and wound healing. PRP has been used in dermatology for skin rejuvenation and alopecia.
Objective:
The objective of our study was to study efficacy of PRP with microneedling in patients with androgenetic alopecia (AGA) and to assess number of sessions required for a patient.
Materials and Methods:
Sixty patients diagnosed with AGA were studied between August 2016 and October 2018 who did not respond to minoxidil and finasteride. PRP was prepared by centrifugation of patients’ blood. PRP with microneedling was done for all patients under aseptic conditions. Four to six sessions were done at an interval of 4 weeks. Subjective and objective scores were assessed based on a visual analog global score. Assessment was done at the first session, every next sitting, and 4 weeks after the last sitting. Follow-up was done at 3rd and 6th month after the last sitting.
Results:
According to subjective scores, two patients (3.33%) had excellent results, 24 (40%) very good, 22 (36.6%) good, 6 (10%) fair results, and 6 (10%) did not have any response. Objective assessment scores showed that two patients (3.33%) had excellent results, 26 (43.3%) very good, 21 (35%) good, 7 (11.6%) had fair results, and 4 (6.7%) did not have any response. Fifty patients underwent four sessions out of which 40 (i.e. 66%) patients had very good results. Only 10 patients required more than four sessions to achieve good results. Patients were happy with four sessions. There were no side effects noted either during or after the treatment.
Conclusion:
This study shows PRP with microneedling as an efficacious treatment for AGA and augments the effects of conventional treatment. This study sets example for assessing the number of PRP sessions. A minimum of four sessions is required to achieve very good results.
Keywords
Androgenic alopecia
microneedling
platelet-rich plasma
Platelet-rich plasma enhances hair growth in AGA
and consistent treatment with PRP yields better results

INTRODUCTION
Platelet-rich plasma (PRP) is an emerging modality of treatment without any adverse effects. PRP is an autologous concentration of platelets in a fraction of plasma. Platelets are the source for growth factors (GFs), and this is the rationale for its use in alopecia as well as other dermatological conditions. Androgenetic alopecia (AGA) is a hereditary, androgen-dependent disorder of hair which is very common among men as well as women. Besides being an aesthetic concern, for both patient and physician, AGA is a common cause of psychosocial stress among both sexes. The treatment modalities are limited to topical minoxidil and oral/topical finasteride. Though these are FDA-approved, concern about long-term efficacy and safety profiles lowers patients’ compliance and this in turn paved way for this newer modality of treatment without any adverse effects. Our aim was to show the efficacy of PRP along with microneedling in such patients, simultaneously assessing the number of sessions required.
MATERIALS AND METHODS
This was a retrospective analysis and included 60 patients suffering with AGA. The study was done from August 2016 to October 2018. Inclusion criteria were patients those who did not respond to topical minoxidil and oral finasteride and those who were unresponsive or unwilling to use finasteride. Minoxidil takes at least 3 months to show its results as far as reducing hair fall or causing thickening of hairs. So we took 4 months to give significant time before concluding up as non-responders.
Our exclusion criteria were patients who have history of malignancies, platelets disorders, uncontrolled diabetes mellitus, anemia or bleeding disorders, immunocompromised patients, keloidal tendency, women who were pregnant or breastfeeding, and patients with unrealistic expectations. Patients were asked to continue topical minoxidil throughout the sessions. No other oral drugs were prescribed.
Scalp was examined to exclude any inflammation, erythema, or scarring prior to the procedure. At each session, informed consent from the patient and photographs were taken to evaluate overall improvement in hair growth, hair volume, and fullness from the front, vertex, lateral, and back views. An aliquot of 8 mL of venous blood was collected in tubes containing ACD and gel separator under aseptic condition. The collected blood sample was subjected to centrifugation at 3500 RPM for 10 min. The red blood cells (RBCs) were separated and settled at the bottom below the gel. A clear plasma containing platelets was collected above the gel. An aliquot of 5 mL of PRP was formed. Extraction of only PRP from the tube through a syringe was difficult and invariably some amount of platelet-poor plasma (PPP) also gets extracted. However, studies have shown that even PPP also includes GFs. Hence instead of discarding, we also took some amount of PPP along with PRP.[1] The PRP was loaded in 1 mL insulin syringes, and calcium chloride (nine parts of PRP and one part calcium chloride) was added just prior to the treatment.
Meanwhile, scalp was anesthetized either by applying topical EMLA for 30 min or by giving local anesthetic injections in a circular fashion on the scalp only in apprehensive patients. Some patients who refused both forms of anesthesia could manage even with just vibration anesthesia.
Area of the scalp to be treated was cleansed with betadine solution. Microneedling was done with a dermaroller studded with 1.5 mm length needles. The dermaroller was moved on scalp horizontally, vertically, and crisscross directions. Pinpoint bleeding was the end point following which PRP was applied topically. Patients were asked to go back home/work same day and were advised not to wash scalp that day. Topical minoxidil was advised to be applied from next day till next session. Sessions were repeated at 4-week interval and a total of four to six sessions were done.
Based on the visual analog global scale, objective and subjective scorings were done as shown in Table 1. Objective assessment was done by comparing global photographs taken at the beginning of the treatment, every session, and 4 weeks after the last session. Patients’ satisfaction scores were taken based on hair loss reduction and overall visual improvement in hair thickness/quality on a scale ranging from 0% to 100%. Follow-up was done at 3rd month and 6th month after the last session. Statistical analysis and p-value were measured by using the z-test.
| % of Improvement | Scoring |
|---|---|
| <19 | Poor |
| 20–39 | Fair |
| 40–59 | Good |
| 60–79 | Very good |
| >80 | Excellent |
RESULTS
Out of 60, 12 were female and 48 were male patients. Their age varied from 19 to 45 years with a median age of 30.5 years.
According to subjective scores (PSS), two patients (3.33%) had excellent results, 24 (40%) had very good, 22 (36.6%) had good, 6 (10%) had fair results, and 6 (10%) did not have any response. Objective assessment scores (OAS) showed that two patients (3.33%) had excellent results, 26 (43.3%) had very good, 21 (35%) had good, 7 (11.6%) had fair results, and 4 (6.7%) did not have any response [Table 2]. Figures 1–3 show the images of three patients with very good and excellent results after four sessions.
| Grading and percentage of improvement | Patients’ satisfaction score (PSS) | Objective assessment score (OAS) |
|---|---|---|
| Poor (≤ 19%) | 6 (10) | 4 (6.7) |
| Fair (20–39%) | 6 (10) | 7 (11.6) |
| Good (40–59%) | 22 (36.6) | 21 (35) |
| Very good (60–79%) | 24 (40) | 26 (43.3) |
| Excellent (≥80%) | 2 (3.33) | 2 (3.33) |
| Total (n=60) | 60 (100) | 60 (100) |
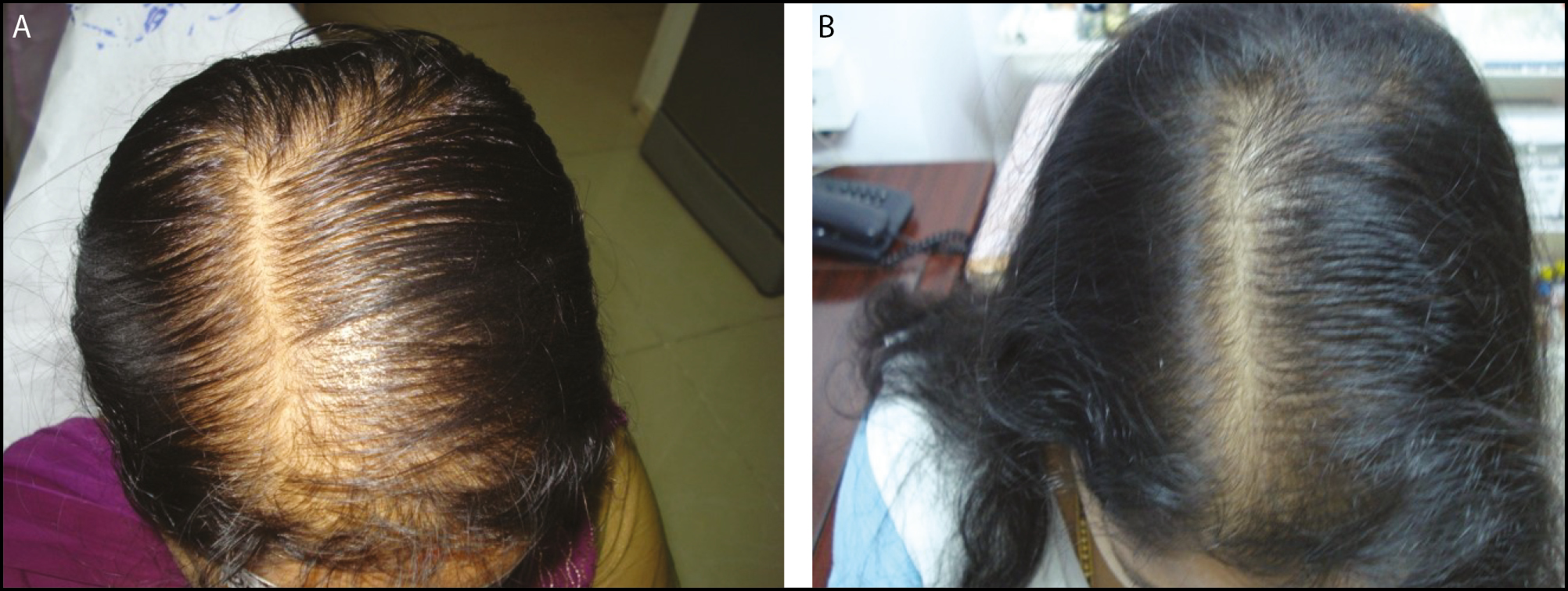
- A: A 40-year-old female before treatment. B: After four sessions—excellent results
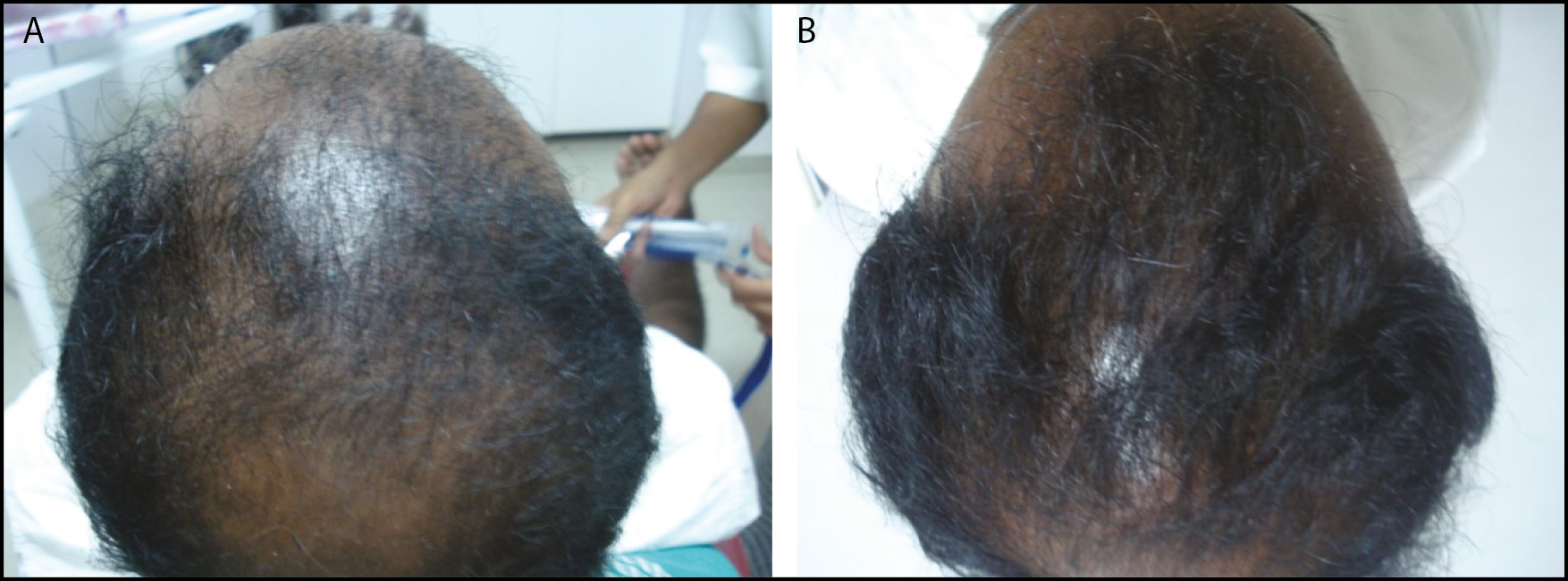
- A: A 35-year-old male before treatment. B: After four sessions—very good results

- A: A 30-year-old male before treatment. B: After four sessions—excellent results
After the first session, nearly 58 patients had less than 40% improvement. After the last session, 49 (81.6%) patients had more than 40% improvement [Table 2]. Patients noticed improvement in terms of reduced hair fall and improvement in hair thickness.
An attempt was made to assess the minimum number of sessions required for satisfactory results. Out of 60, almost 50 (83.3%) patients underwent four sessions. Comparison between the first session and last (fourth) session showed the following results [Table 3].
| Grading and percentage of improvement | No. of patients (%) after first session | No. of patients (%) after fourth session | P-value |
|---|---|---|---|
| Poor (≤ 19%) | 21 (42%) | 3 (6%) | 1 |
| Fair (20–39%) | 28 (56%) | 7 (14%) | 0.6 |
| Good (40–59%) | 1 (2%) | 15 (30%) | 0.05 |
| Very good (60–79%) | 0 (0%) | 23 (46%) | 0.02 |
| Excellent (≥ 80%) | 0 (0%) | 2 (4%) | 0.05 |
| Total (n=50) | 50 (100%) | 50 (100%) |
Out of those 50 patients who took four sessions, three did not have any improvement, seven patients had fair results, 40 patients (i.e. 66.7%) had good to excellent results with significant P-value as shown in Table 3.
Ten patients (16.67%) needed more than four sessions to get more than 40% improvement (P-value=0.007). Out of these 10, one patient did not have any improvement despite more sessions. Based on these results and number of sessions analysis, it shows that majority were satisfied with the results achieved from four sessions. Hence, we opine that a minimum of four sessions is required to achieve good results [Table 4].
| No. of sessions | No. of patients who underwent | No. of satisfied patients | % of patients satisfied (out of total 60 patients) |
|---|---|---|---|
| Four sessions | 50 | 40 | 66.7% |
| More than four | 10 | 9 | 15% |
Ten patients (6%) complained of a mild headache after the procedure for 1 day, which subsided with paracetamol 500 mg. None of the patients had any other side effects. Follow-up at 3rd month and 6th month showed persistent results in all except 3 male patients who resumed hair fall after 3 months.
DISCUSSION
In the present era, there is a hype of PRP in dermatological and aesthetic indications causing enthusiasm both for the physicians and patients.
PRP has been emerging rapidly both for skin rejuvenation and for hair loss. Literature has many publications, and in the last 5 years, there are increasing numbers of articles favoring PRP treatment for alopecia. The European Dermatology Forum proposed evidence-based (s3) guidelines for the treatment of AGA both in men and in women.[2] According to this guideline, PRP was given level of evidence 3.
PRP is defined as an autologous concentration of platelets in plasma fraction of blood prepared from the patient’s venous blood. The blood thus drawn is subjected to differential centrifugation to separate platelets from RBCs. The desired platelet concentration is four to five times above the baseline platelet count which is 200,000 cells/µL.[3]
AGA is genetic, hormonal-influenced, non-scarring patterned hair loss which affects both the genders and is a common cause of psychosocial distress for both the genders. Only two FDA-approved medications are available for AGA, i.e. minoxidil and finasteride. However, few drawbacks of minoxidil, such as daily twice application, dryness or irritation, initial shedding of the telogen hairs, and adverse effects of finasteride though very rare, reduce patient compliance for both the drugs. Apart from these two drugs, the other option is surgical hair transplantation (HT). But HT is an expensive treatment and affordability is an issue. Hence, an alternate modality of treatment is the need of hour to benefit patients in an effective way by overcoming these drawbacks. PRP is one such modality which is safe and office-based procedure with ability to improve hair growth in AGA at affordable costs.
Hair growth cycle is regulated by different GFs. Platelet-derived growth factor (PDGF), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), transforming growth factor beta (TGF b1 and b2), insulin 1-like growth factor (IGF-1), and fibroblast growth factor (FGF)[4] are the major growth factors involved in the hair follicle formation. The growth factors are stored in the alpha granules of platelets which are released on activation by a process called degranulation. PRP releases growth factors from the platelet concentrate and also stimulates molecular signaling pathways.[35] PRP increases phosphorylation of extracellular signal-regulated kinases (ERK) and PI 3-kinase/Akt signaling pathways which promote hair growth and prevent apoptosis.[46] The procedure is safe and till date there are no side effects reported. There is rare possibility of transmission of infection if done under strict aseptic precautions. Pain during the therapy is a limitation. Ninety percent of the patients could tolerate the pain during procedure and in the remaining it was alleviated with topical EMLA, vibration anesthesia, or ring block.
In our study, PRP was prepared using single spin technique using PRP tubes prefilled with anti-coagulant and cell separator. Centrifugation at 3500 RPM for 10 min was done. Following this, RBCs were collected at the bottom of the tube with plasma above containing platelet concentrate. Many studies use single spin technique for separating platelets.
As stated earlier, PRP is rich in several GFs. However, it has been shown that even PPP contains platelets and GFs, though in lesser concentration compared with PRP. Hence, we decided not to reject the PPP and collected PRP along with PPP for application.[1]
Activator used was calcium chloride in the ratio of 1:9 to PRP. Though there is a controversy regarding use of activator, most of the studies have used activator before injecting PRP. PRP can be either injected directly (subdermal or intradermal) or can be applied topically after microneedling. When PRP comes in contact with the skin/dermal collagen after microneedling it gets activated automatically; hence no need of activator.[7] Activator can be used when direct PRP injections are given. The GFs are released within 10 min of activation by CaCl2.[8] Hence, PRP treatment to affected area should be started immediately after addition of activator.
In our study, the hair growth results were evaluated based on global photographs which was at par with the European Dermatology forum. According to the European guidelines, global photographic assessment was recommended as the most effective evaluation method of hair growth and was proposed to be used even for long-term follow-up.[2]
In our study, a dermaroller of 1.5 mm needles was used to microneedle on scalp in vertical, horizontal, and crisscross directions. Pinpoint bleeding was taken as end point following which the PRP was applied. Microneedling has several benefits. The pinpoint bleeding/pores created due to microneedling ensures uniform absorption of PRP in the affected areas, thus enhancing its efficacy. In contrast, the micro-injury caused by microneedling itself recruits growth factors such as epidermal growth factor and platelet growth factor through platelet activation and wound healing mechanism and increases expression of Wnt proteins especially Wnt3a and Wnt10b which in turn stimulate dermal papillae cells and increase blood supply.[910]
Our study has demonstrated PRP as an effective, adjuvant therapy in AGA when combined with microneedling. Studies with such combination are very less. Jha et al.[11] reported in 2019 that PRP with microneedling had better outcome in AGA when compared with PRP alone or with minoxidil. This study was done on 93 patients. In another study, Jha et al.,[12] in 2018, noted significant hair growth after three sessions of PRP with microneedling and their results were assessed dermascopically also. The patient satisfaction score was 75% in 18 patients in their study.
Shah et al.[13] also performed a comparative study in 2017 of PRP with microneedling plus minoxidil in one group and topical minoxidil alone in another group. The group who received PRP with microneedling group has significant improvement (P < 0.005) when compared with the control group. Greco and Brandt[14] demonstrated PRP with microneedling in AGA patients. They observed a significant increase in hair diameter and its density, respectively, with this minimally invasive technique. Microneedling using a dermaroller creates multiple microchannels and has been shown to increase transdermal penetration of drugs, facilitating higher concentration in dermis.[15]
There are many studies showing microneedling treatment alone in AGA patients. Dhurat et al.[9] in 2013 conducted a randomized evaluator-blinded controlled study on 100 patients. The study showed significant improvement of hair count (P = 0.0039) in patients who underwent dermaroller along with minoxidil when compared with those with minoxidil treatment only. Another study by Dhurat et al.,[16] in 2015, shows that microneedling was done in four patients not responding much to medical treatment. These patients showed 50–75% improvement in hair growth after microneedling. This study shows that microneedling can augment the conventional treatment in AGA. We therefore feel a separate controlled study of PRP with and without it is warranted to address this confounding factor.
Number of sessions
We repeated sessions at 1-month interval. Four sessions were required to get very good results. Gkini et al. studied the effect of PRP injections in 20 patients with AGA. They performed three sessions at an interval of 3 weeks and one booster session after 6 months. Their results were based on noninvasive evaluation methods, such as hair pull test, hair density, dermoscopic photomicrographs, and patients’ satisfaction scale. The study showed a significant increased rate in hair density at 3 months (170.70 ± 37.81, P < 0.001) and 6 months (156.25 ± 37.75, P < 0.001), respectively, with reduction in hair loss compared to baseline.[16] This is a well-designed study, with statistical analysis, with relative objective evaluation methods, but no controls. Singhal et al. investigated the clinical efficacy of PRP in the treatment of AGA on 10 patients who were given autologous PRP over a period of 3 months at an interval of 2–3 weeks and results were assessed. Three months after the treatment, the patients presented clinical improvement in the hair counts, hair thickness, hair root strength, and overall alopecia, whereas there was no improvement in the control group.[17] Most of the studies as shown in Table 5 performed three sessions at monthly intervals to be efficacious in AGA. Our study correlates with these studies.
| Study | No. of sessions | Results |
|---|---|---|
| Gkini et al.[17] | Four sessions | Yes |
| Singhal et al.[18] | Four sessions 3 weeks apart | Yes |
| Shah et al.[13] | Six sessions 1 month apart | Yes |
| Alves et al.[19] | Three sessions 1 month apart | Yes |
| Gentile et al.[20] | Three sessions 1 month apart | Yes |
| Cervelli et al.[21] | Three sessions 1 month apart | Yes |
| Takikawa et al.[22] | Five sessions 2 weeks apart | Yes |
| Ayatollahi et al.[23] | Five sessions 2 weeks apart | No |
| Jha et al.[12] | Three sessions 3 weeks interval | Yes |
Pain is one of the limiting factors in PRP therapy. In spite of local anesthesia, patients complain of mild pain during the procedure. Post-procedure pain is minimal and patients are comfortable. Better methods of achieving anesthetic effects before injecting PRP have to be studied and investigated further to make the procedure more pleasant both for the physician and the patient.
CONCLUSION
We can conclude from our study that PRP with microneedling is an effective way of treating AGA. Our study also shows that PRP augments the effects of conventional therapy like minoxidil and finasteride; however, the assessment of results was limited to global photographs and not by hair count. There are very few publications on PRP with microneedling in AGA. Simultaneously, we can also show that a minimum of four sessions is required to achieve the desired effect. However, taking into consideration individual patient factors, some may require more than 4 sessions.
Guidelines and protocols on the various steps involved in the preparation of PRP like centrifugation, temperature, platelet concentration measure, and evaluation methods are important in obtaining consistent results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Assessment of the efficacy and safety of platelet poor plasma gel as autologous dermal filler for facial rejuvenation. 2019. J Cosmet Dermatol. 18:1271-9. https://doi.org/10.1111/jocd.12876
- [Google Scholar]
- Evidence-based (S3) guideline for the treatment of androgenetic alopecia in women and in men—short version. J Eur Acad Dermatol Venereol. 2018;32:11-22.
- [Google Scholar]
- Principles and methods of preparation of platelet-rich plasma: A review and author’s perspective. J Cutan Aesthet Surg. 2014;7:189-97.
- [Google Scholar]
- Autologous platelet-rich plasma: A potential therapeutic tool for promoting hair growth. Dermatol Surg. 2012;38:1040-6.
- [Google Scholar]
- Platelet-rich plasma: The choice of activation method affects the release of bioactive molecules. Biomed Res Int. 2016;2016:6591717.
- [Google Scholar]
- Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001;10:225-8.
- [Google Scholar]
- A randomized evaluator blinded study of effect of microneedling in androgenetic alopecia: A pilot study. Int J Trichology. 2013;5:6-11.
- [Google Scholar]
- Microneedling for the treatment of hair loss? J Eur Acad Dermatol Venereol. 2018;32:564-9.
- [Google Scholar]
- Platelet-rich plasma and microneedling improves hair growth in patients of androgenetic alopecia when used as an adjuvant to minoxidil. J Cosmet Dermatol. 2019;18:1330-5.
- [Google Scholar]
- Original article: Platelet-rich plasma with microneedling in androgenetic alopecia along with dermoscopic pre- and post-treatment evaluation. J Cosmet Dermatol. 2018;17:313-8. 10.1111/jocd.12394. Epub August 3, 2017
- [Google Scholar]
- A comparative study of microneedling with platelet-rich plasma plus topical minoxidil (5%) and topical minoxidil (5%) alone in androgenetic alopecia. Int J Trichology. 2017;9:14-8.
- [Google Scholar]
- The effects of autologous platelet rich plasma and various growth factors on non-transplanted miniaturized hair. Hair Transplant Forum Int. 2009;19:49-50.
- [Google Scholar]
- Microneedles: A valuable physical enhancer to increase transdermal drug delivery. J Clin Pharmacol. 2011;51:964-77.
- [Google Scholar]
- Response to microneedling treatment in men with androgenetic alopecia who failed to respond to conventional therapy. Indian J Dermatol. 2015;60:260-3.
- [Google Scholar]
- Study of platelet-rich plasma injections in the treatment of androgenetic alopecia through an one-year period. J Cutan Aesthet Surg. 2014;7:213-9.
- [Google Scholar]
- Efficacy of platelet-rich plasma in treatment of androgenic alopecia. Asian J Transfus Sci. 2015;9:159-62.
- [Google Scholar]
- Randomized placebo-controlled, double-blind, half-head study to assess the efficacy of platelet-rich plasma on the treatment of androgenetic alopecia. Dermatol Surg. 2016;42:491-7.
- [Google Scholar]
- The effect of platelet-rich plasma in hair regrowth: A randomized placebo-controlled trial. Stem Cells Transl Med. 2015;4:1317-23.
- [Google Scholar]
- The effect of autologous activated platelet rich plasma (AA-PRP) injection on pattern hair loss: Clinical and histomorphometric evaluation. Biomed Res Int. 2014;2014:760709.
- [Google Scholar]
- Enhanced effect of platelet-rich plasma containing a new carrier on hair growth. Dermatol Surg. 2011;37:1721-9.
- [Google Scholar]
- Platelet-rich plasma by single spin process in male pattern androgenetic alopecia: Is it an effective treatment? Indian Dermatol Online J. 2017;8:460-4.
- [Google Scholar]





