Translate this page into:
Pleomorphic Adenoma of the Upper Lip
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Pleomorphic adenoma or mixed tumour is a benign salivary gland tumour, presenting usually in the parotid or submandibular glands. This tumour contains elements of both epithelial and mesenchymal origin.[1] They are the most common tumours (50%) of the major and minor salivary glands. The palate is considered as the most common intraoral site (42.8–68.8%), followed by the upper lip (10.1%) and cheek (5.5%). Other rare sites include the throat (2.5%), retromolar region (0.7%), floor of the mouth and the alveolar mucosa.[2] It mainly affects women in their fourth to sixth decade of life. The patients usually present with a painless and slow-growing mass.[3] Histologically, it is characterized by a large variety of tissues consisting of epithelial cells arranged in a cord-like cell pattern, together with areas of squamous differentiation or with plasmacytoid appearance myoepithelial cells which are responsible for the production of abundant extracellular matrix with chondroid, collagenous, mucoid and osseous stroma.[4] We present a case of pleomorphic adenoma in the upper lip, which is a rarely reported location. A brief review of the relevant literature is also presented.
A 65-year-old female presented with a painless, slowly progressing swelling over the upper lip for the last 2 years [Figure 1]. There was no preceding history of trauma and her past medical history was unremarkable. The general health of the patient was preserved. On examination, the mass was circumscribed, sessile and firm in consistency measuring 2 × 1.5 cm in diameter. The overlying mucosa was smooth with a pinkish purple colour. The skin over the tumour was not fixed. There was no pain or bleeding on palpation. There was no regional lymphadenopathy and her general physical and systemic examinations were normal. Fine needle aspiration cytology (FNAC) revealed a biphasic pattern comprising epithelial component and fibromyxoid stroma, suggesting a diagnosis of pleomorphic adenoma. The tumour was completely removed with a lip splitting incision. During the surgical procedure, the lesion was excised without difficulty with a clinically normal margin because the mass was fully encapsulated without any subcutaneous or muscle attachments. Sutures were given with good approximation and cosmetic results. A subsequent follow-up after 1 year showed no signs of recurrence. Grossly, a grey-white tissue piece of firm consistency was received, measuring 3.5 × 2 × 1 cm. The cut surface of the lesion was solid and grey-white to tan in colour with occasional cystic areas. On histology, a well-circumscribed growth was seen comprising epithelial and stromal components. The epithelial component formed glandular structures lined by round-to-oval cells having small nuclei, pink cytoplasm and a myoepithelial basal cell layer while the stroma had a fibromyxoid appearance [Figures 2 and 3]. There was no evidence of mitosis and necrosis. The cytokeratin (CK; DAKO) immunohistochemical marker showed positive staining by the epithelial cells. S-100 (DAKO) and smooth muscle actin (SMA; DAKO) immunohistochemical markers revealed myoepithelial cell positivity. A diagnosis of pleomorphic adenoma was made with these findings.

- Clinical photograph of a firm, fixed swelling of the upper lip measuring 2 × 1.5 cm
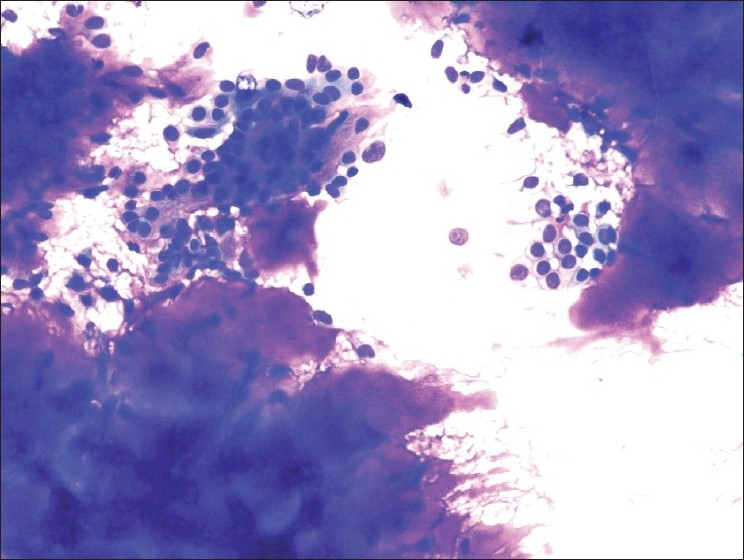
- FNA smears reveal sheets of epithelial cells and abundant fibromyxoid stroma (MGG; ×200)
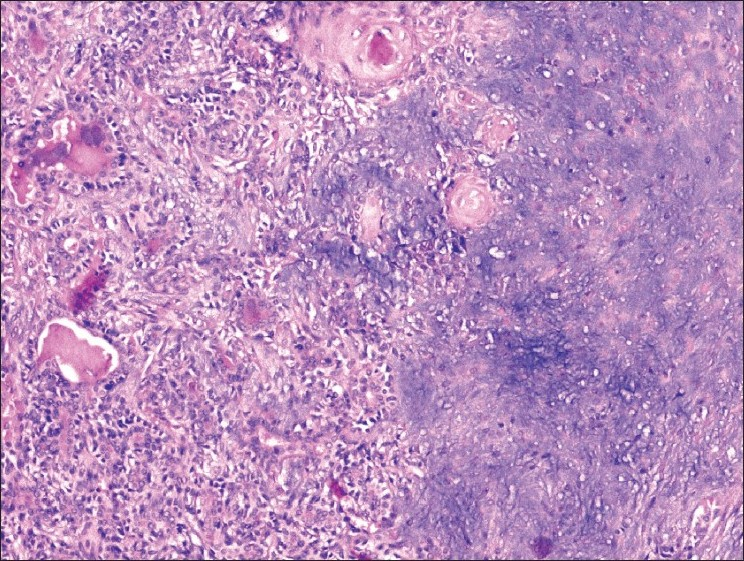
- Microsections reveal ducts and acini with a preserved myoepithelial cell layer in chondromyxoid stroma (H and E; ×100)
Salivary gland tumours are rare and constitute 2–6.5% of all head and neck tumours.[3] Tumours arising in the minor salivary gland account for 22% of all salivary gland neoplasms. Majority of them are malignant with only 18% being benign, of which pleomorphic adenoma is the commonest.[5] Pleomorphic adenoma is the most common tumour of the salivary glands. These tumours make up 70% of the parotid tumours, 50% of the submandibular gland tumours and 45% of the minor salivary gland tumours.[3]. They mostly arise in the parotid or submandibular salivary glands and the minor salivary glands that are distributed throughout the oral cavity. The most frequent site of pleomorphic adenoma of the minor salivary glands is the hard and soft palate, followed by the upper lip.[1] The definite aetiology is not known. However, cytogenetic and molecular studies have shown an epithelial origin for the tumour with chromosomal abnormality in 8q12 and 12q25.[3] Pleomorphic adenoma arising from minor salivary glands of the lips tends to occur at an earlier age than it does at other sites.[6] Bernier found that the peak incidence of pleomorphic adenoma of the lips was in third to fourth decade of life, with an average age of 33.2 years, but in our study, patient's age was 65 years.[7]
Pleomorphic adenoma of the upper lip exceeds that of the lower lip by the ratio of 6:1. There is a propensity for benign tumours to occur on the upper lip, whereas malignant lesions predominate on the lower lip. The reason for this difference has been thought to be due to the differences in embryonic development between the upper and lower lips.[6] Eveson and Cawson documented 75% of upper lip tumours as benign.[8]
Jaber has reported from a study on 75 patients with intraoral minor salivary gland tumours that 15 of the 29 benign tumours were palatal in location with only four on the upper lip and one on the lower lip.[9]
Minor salivary gland tumours present as soft to firm masses arising inside the mouth. Less common symptoms are ulceration, tenderness and difficulty in talking. Histopathologically, pleomorphic adenoma is an epithelial tumour of complex morphology, possessing epithelial and myoepithelial elements arranged in a variety of patterns and embedded in the mucopolysaccharide stroma. The formation of capsules occurs as a result of fibrosis of the surrounding salivary parenchyma, which is compressed by the tumour and is referred to as ‘false capsule’.[5]
The differential diagnosis of intraoral solid and asymptomatic nodules includes minor salivary gland tumours and benign and malignant mesenchymal tumours such as neurofibroma, lipoma and rhabdomyosarcoma. The minor salivary gland tumours, myoepithelioma and basal cell adenoma, are the primary consideration in the differential diagnoses. Myoepithelial cells are dominant, and ductal structures are very rare in myoepithelioma. Basal cell adenoma is generally palatal in location and has no capsule.[3] The surgical treatment for pleomorphic adenoma is a complete wide surgical excision with a good safety margin. An inadequate resection or rupture of the capsule or tumour spillage during excision can lead to local recurrence.
Pleomorphic adenoma of the lip is a rare neoplasm and therefore its diagnosis requires a high index of suspicion. A complete wide surgical excision is the treatment of choice. Recurrence after many years of surgical excision as well as malignant transformation should be a concern and therefore long-term follow-up is necessary.
REFERENCES
- Pleomorphic adenoma of the hard palate. Indian J Dermatol Venereol Leprol. 2003;69:74-5.
- [Google Scholar]
- Juvenile pleomorphic adenoma of the cheek: A case report and review of literature. Diagn Pathol. 2009;4:32.
- [Google Scholar]
- Pleomorphic adenoma of minor salivary gland in the parapharyngeal space. World J Surg Oncol. 2003;1:2.
- [Google Scholar]
- Pleomorphic adenoma of the upper lip: A case report. Nepal Med Coll J l. 2010;6:51-3.
- [Google Scholar]
- Tumors of the minor (oropharyngeal) salivary glands: A demographic study of 336 cases. J Oral Pathol. 1985;14:500-9.
- [Google Scholar]
- Intraoral minor salivary gland tumors: A review of 75 cases in Libyan population. Int J Oral Maxillofac Surg. 2006;35:150-4.
- [Google Scholar]





