Translate this page into:
Potential execution of vitiligo surgery by the most conceivable technique – which, where, and why?
*Corresponding author: Sushil S. Savant Jr., Department of Dermatology, The Humanitarian Clinic: Skin, Hair and Laser Centre, Mumbai, Maharashtra, India. sushilsavant786@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Savant S S. Jr., Savant S. Potential execution of vitiligo surgery by the most conceivable technique – which, where, and why? J Cutan Aesthet Surg. 2024;17:282-91.doi: 10.25259/jcas_128_23
Abstract
While various treatment options exist for vitiligo, surgical interventions have gained significant attention due to their potential for long-lasting repigmentation. Several surgical procedures have been developed, including miniature punch grafting, thin Theirsch’s split-thickness skin grafting (STSG), suction blister technique, and ultrathin STSG. The decision-making process should also consider the potential risks and benefits associated with each technique. Factors such as graft survival, color match, post-operative complications, and long-term stability of repigmentation should be evaluated. In addition, patient factors such as comorbidities, skin type, and psychological impact should be carefully considered to ensure optimal surgical outcomes. We, hereby, aim to explore the potential execution of vitiligo surgery using the most conceivable technique, considering factors such as efficacy, safety, and patient-specific characteristics.
Keywords
Efficacy
Vitiligo
Safety
Surgery
INTRODUCTION
In stable vitiligo, surgical intervention is indicated when it is refractory to the conventional medical line of treatment/phototherapy.1,2 This can be achieved by various surgical methods such as permanent camouflaging – tattooing (T)3,4 or surgically activating the lesional and perilesional dormant melanocyte reservoir – therapeutic wounding (TW)3,5,6 or seeding (transplanting) the area either through autologous tissue graft/grafts – miniature punch grafting (MPG),3,7 thin Theirsch’s split-thickness skin grafting (STSG),3,8 suction blister technique (SBT),3,9 ultrathin split-thickness skin grafting (UTSG)3,10,11 single – hair follicular unit transplant (FUT),12 follicular unit extraction (FUE),13 eyelash transplantation,14 or cellular suspensions/culture – autologous non-cultured melanocytes – keratinocytes cell suspension (NCMKCS),3,15-18 autologous cultured melanocytes,3,15,19,20 autologous epidermal cell transfer technique (Jodhpur technique),21, etc. Most of them have claimed good to excellent results (60–95% re-pigmentation)3,22 with whichever surgical method they have adopted, depending on the type, size, site, and stability of the vitiligo lesion, and age and color complexion of the patient. Addition of psoralen (P) and ultraviolet radiation (UVA) (PUVA) or psoralen and UVA obtained by sunlight (PUVASOL), or narrow-band ultraviolet light B (NBUVB), or excimer laser/lamp phototherapy enhances the rate of pigmentation with an increased overall success rate (90–95%).3,11,20-23 All these techniques aim to achieve uniform re-pigmentation, color match, and good cosmesis. The dermatosurgeon is often in a dilemma to deciding the ideal surgical modality in an individual case as all these have their advantages, disadvantages, limitations, and complications.3,22-24
TATTOOING (T)
Advantages
It is only a camouflaging procedure. It is useful for small patches located on the lip [Figure 1], nipple, and genitalia in dark-complexioned individuals to achieve a good color match. It gives instantaneous results and is useful in emergencies (impending marriage, job interviews, and medical examinations).3,4,22

- Tattooing in lip vitiligo.
Disadvantages
It has limitations and complications such as mismatched color, change in color shade, fading of color, and reaction to tattoo pigments over time.3,4,22
THERAPEUTIC WOUNDING (TW)
Advantages
In this technique, faster re-pigmentation can be induced with various wounding techniques to cover large areas (dermabrasion/laser ablation) as well as small residual areas (phenol, trichloroacetic acid [TCA], and needling with or without 5-fluorouracil [5-FU] cream) [Figure 2].3,5,6,22,25

- Therapeutic wounding.
Disadvantages
It can be carried out only in hairy areas where 25–50% of the existing hair is black.3,5,6,22,25
MINIATURE PUNCH GRAFTING (MPG)
Advantages
It is a simple and friendly office-based technique for dermatosurgeons with a high success rate of re-pigmentation and can be carried out on most body parts [Figure 3]. It is best suited and highly recommended for acral vitiligo (fingertips and toe tips) [Figure 4], for palms and soles, and genital vitiligo [Figure 5].3,7,22,24 None of the other available techniques give satisfactory results due to local factors such as the absence of hair follicles thick epidermis, constant (frictional) trauma, and inadequate depth achieved during dermabrasion/carbon dioxide (CO2) laser ablation.3,7,22,24 Other than T, punch grafting can be done over the vulva with the fixation of grafts with cyanoacrylate glue.26
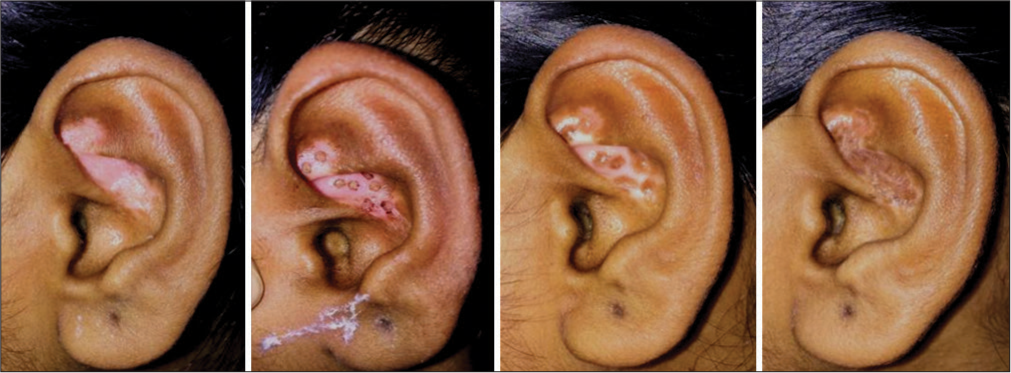
- Miniature punch grafting for vitiligo focalis in conchae or ear.

- Miniature punch grafting for acral vitiligo.

- Miniature punch grafting for genital vitiligo.
Disadvantages
Cobble-stoning, polka dot appearance, de-pigmented junctional line, superficial scarring of the donor site, etc., are some of its limitations and complications.3,7,22,24
Over time, changes have been made to procedures such as the way tissue for transplants is obtained, which has reduced the possible complications. In a case study, Hirobe and Enami showed the use of an electric micro-drill to create a graft that was 1.5–1.8 mm deep and had a diameter of 0.6–1.0 mm. This reduced the chance of cobblestoning and enhanced pigment distribution.27 According to a clinical trial conducted by Ragab et al., the greatest degree of repigmentation and fastest response were obtained with mini-punch grafting and weekly needling over 6 months. Only transverse needling and mini-punch grafts outperformed the control group in terms of outcomes. There were no documented negative effects related to steroids. Consequently, the application of transverse needling after mini-punch grafting positively impacts the ultimate therapeutic outcomes. Compared to MPG and needling done separately, this adjustment enables one to achieve a higher degree of repigmentation in less time and with the lowest cumulative dose of NB-UVB.28
THIN THIERSCH’S SPLIT THICKNESS SKIN GRAFT (STSG)
Advantages
It achieves fast results; large areas can be covered with a high rate of excellent pigmentation, color match, and cosmesis. It can cover most of the body sites except fingertips, toe tips palms, and soles.3,8,22,24
Disadvantages
Hyperpigmentation of the graft at the recipient area, perilesional halo, stuck-on tire appearance, beaded borders, etc., are some of its main limitations and complications.3,8,22,24
SUCTION BLISTER TECHNIQUE (SBT)
Advantages
It is one of the best methods to obtain excellent re-pigmentation and color match as there is direct transfer/transplant of melanocytes from the epidermal graft [Figure 6]. It is a safe, inexpensive office-based procedure.3,9,22,24

- Suction blister grafting for lip vitiligo.
Disadvantages
It is time-consuming, sometimes there may be hyperpigmentation or incomplete pigmentation, and only small areas (lips and eyelids) can be treated at 1 time.3,9,22,24
Consequently, other methods that are effective for creating suction blisters for grafting have been recently developed. These methods include a unique Korean method based on cups with valves, modified syringe procedures that include a three-way tap system, or a formula that uses an automated device called CelluTomeTM for epidermal graft harvesting.29-34 All body areas appear acceptable for blister formation, although the thigh or the forearm remains the preferable site, given that scarring following suction blister epidermal graft (SBEG) is an extremely rare complication.35 Furthermore, research findings have indicated that SBEG is effective in treating regions such as the lips’ angles, which are commonly considered to be extremely difficult to cure.9 Iwanowski et al. and Hann et al. found that phototherapy can be used as a complementary treatment following successful grafting.35,36
ULTRATHIN SPLIT-THICKNESS SKIN GRAFTING (UTSG)
Advantages
It is one of the best methods to obtain a high success rate of excellent re-pigmentation, color match, and cosmesis as there is direct transfer/transplant of melanocytes from the ultrathin graft which dries off or is peeled off or slightly thicker graft (>0.005 inch/0.1 mm) gets taken up as STSG [Figure 7]. Vitiliginous areas of any size, shape, and at any place can be treated except fingertips, toe tips, palms, and soles.3,10,11,22,23

- Ultra-thin skin grafting for segmental vitiligo.
Disadvantages
Time consuming procedure, requires expensive equipment, and surgical expertise, and can cover vitiliginous areas in a 1:1 ratio only.3,10,11,22,23
SINGLE – HAIR FOLLICULAR UNIT TRANSPLANT (FUT), FOLLICULAR UNIT EXTRACTION (FUE), AND EYELASH TRANSPLANTATION
Advantages
These are extremely good methods to treat vitiliginous patches on the scalp, leukotrichia of eyelashes or eyebrows, mustache, and beard areas with good re-pigmentation.12-14
Disadvantages
It is tedious, time-consuming, requires a longer learning curve, there is scarring at the donor site and it is difficult to treat medium to large-size lesions and glabrous areas with them. Donor hair can be taken from any hairy area, for example, scalp beard, or any other body parts.12-14
AUTOLOGOUS NON-CULTURED MELANOCYTES – KERATINOCYTES CELL SUSPENSION (NCMKCS) TRADITIONAL METHOD AND MODIFIED METHOD WITH READYMADE KIT
Advantages
This is a very good method to achieve excellent re-pigmentation, color match, and cosmesis as there is direct transfer/transplant of melanocytes to the recipient’s vitiliginous lesion. Ten-fold (average 5 folds) large vitiliginous area can be treated at 1 time with small size donor graft [Figure 8]. Vitiliginous areas of any size, shape, and at any place can be treated except fingertips, toe tips, palms, and soles.3,15-18,22,24,37

- Preparation of Autologous non-cultured melanocytes-keratinocytes cell suspension.
Disadvantages
It requires a long time for the spread of pigment, special efforts such as making the suspension viscous are required to retain the suspension (liquid form) over the grafted recipient sites, is time-consuming, and requires special laboratory equipment and chemicals (culture media, solutions) and one has to learn the laboratory techniques. Now, in India, there are specially made ready-made kits available to carry out this procedure, which has the added advantage that they are cost-effective, do not require storage of expensive laboratory chemicals, better-modified media is supplied, and trypsin inhibition is not required; however, the procedure is same.3,15-18,22,24,37
AUTOLOGOUS CULTURED MELANOCYTES
Advantages
In this technique, large areas can be treated at 1 time with a small skin sample resulting in excellent repigmentation with good color match, cosmesis, and uniform texture as melanocytes are directly transferred/transplanted. Vitiliginous areas of any size, shape, and at any place can be treated except fingertips, toe tips, palms, and soles.3,15,19,20,22
Disadvantages
It requires a longer time interval, an expensive procedure, and requires state of art laboratory setup, there are concerns regarding the mutagenicity of certain ingredients of the culture media, it is a two-stage procedure that is not yet commercially available in India.3,15,19,20,22
AUTOLOGOUS EPIDERMAL CELL TRANSFER TECHNIQUE (JODHPUR TECHNIQUE)
Advantages
It is a simple, safe, and inexpensive office-based procedure that can be carried out with minimal complications and gives excellent re-pigmentation and good color match. It is found to be useful in treating perilesional halo.
Disadvantages
It has its limitations such as the slow spread of pigment, needing to be combined with phototherapy, achromic/hypochromic skip areas being left behind, it is difficult to treat large lesions and lesions over lips, fingertips, toe tips, palms, and soles.21,22,38
Despite the limitations, complications, and disadvantages of various techniques, there are certain advantages of each of these techniques mentioned. Njoo et al.39 in one meta-analysis reported that 87% of the patients achieved more than 75% repigmentation with SBT, which was similar to split thickness grafting (87%), but better than mini grafting (68%) and grafting of non-cultured epidermal suspensions (31%). In UTSG, the success rate of re-pigmentation reported varied from 95% to 99%.3,10,11,22,23,40 Total re-pigmentation was reported with TW in 46 (88.5%) out of 52 hairy sites.5 In a study with NCMKCs, segmental and focal vitiligo showed the best results in all the cases followed by generalized vitiligo.17,37 In another study on epidermal grafting, it was reported that segmental and focal vitiligo responded better (91% achieving >75% re-pigmentation) than generalized vitiligo (53%, P< 0.001). However, there was no significant difference in repigmentation rates at different body sites.41 Most of the techniques have reported better results in focal and segmental vitiligo (75–95%) than in generalized vitiligo. Younger (20–30 years) and darker-complexioned patients have better results. Comparatively, acral areas, malleoli, knees, and elbows are less responsive to surgery. Smaller patches respond better. Post-vitiligo surgery PUVA, PUVASOL, NBUVB, and excimer laser/lamp phototherapy accelerate repigmentation and increase the success rate (90–95%).3,11,21-23,40
FACTORS DECIDING TYPE OF VITILIGO SURGERY
Patient selection
This is the most important criterion that a patient’s vitiligo should be stable before planning for any vitiligo surgery. Stable vitiligo is a term coined for such cases, wherein the disease is inactive along with no eruption of fresh lesions, no progression of pre-existing lesions, and no sign of Kobner’s phenomenon for the past 1 year.26 Kobner’s phenomenon may occur in the form of recurrence of vitiligo at the donor or recipient site in the form of the appearance of new lesions in unstable patients or if the disease has become reactive after stability. Hence, proper selection of patients is important to either minimize or avoid these complications.2,3,22,24 It is advisable to do a test grafting using 3–5 mini-punch grafts and observe for its positive response to confirm the stability before treating patients with large lesions with any of the opted/selected surgical modalities. Cyanoacrylate glue can be used to fix the graft in all difficult (periorbital, genital, concha, umbilicus, areola, and underarms) places for surgery that can avoid difficult dressing.42-46
In patients with unrealistic expectations, it is better to avoid surgery. Proper patient counseling and information regarding expected results, complications, and cost of the procedure should be discussed with the patient and further documented to avoid medico-legal complications.
The axillary area can be used as an incubator to reduce the cost of the procedure.47
Cosmetic priority
For exposed cosmetically important areas such as the scalp, face including eyebrows and eyelashes, part of the neck, fingers, hands, and forearm, one has to choose the modality that gives the best cosmetic results depending on the size of the area involved [Table 1]. For areas that are not exposed, most of the modalities are useful and the choice should be given to the patient.
| Site | Treatment of choice | ||
|---|---|---|---|
| 1. | Lips and eyelids | SBT, STSG, and UTSG | |
| 2. | Hairy areas with 25–50% black hairs | TW. | |
| 3. | Scalp, beard, mustache, eyebrows, and eyelashes | Eyelash Transplant, BHT, Single hair FUT,and FUE | |
| 4. | Tips of fingers, toes, palms, and soles | MPG | |
| 5. | Face and neck | Autologous NCMKCS, STSG, and UTSG | |
| 6. | Angle of mouth | MPG-Tattooing in dark patients and UTSG | |
| 7. | Trunks and limbs | Autologous NCMKCS, MPG, Jodhpur technique, STSG, and UTSG | |
| 8. | Genitals | ||
| Vulva | Tattooing | ||
| Penis and scrotum | Tattooing, UTSG, and MPG | ||
SBT: Suction blister technique, STSG: Split thickness skin grafting, UTSG: Ultrathin split-thickness skin grafting, TW: Therapeutic wounding, FUT: Follicular unit transplant, FUE: Follicular unit extraction, MPG: Miniature punch grafting, NCMKCS: Non-cultured melanocytes – keratinocytes cell suspension, BHT: Body hair transplantation
Time bound priority
Some patients require fast results in certain emergencies such as impending marriage, job interviews, or medical examinations, leaving very little time at the disposal of the dermatosurgeon. Such patients can be treated by either T or STSG which give fast results as discussed earlier.
Location of the lesion
Most of the techniques can be carried out to re-pigment vitiliginous lesions located over various parts of the body. However, some technique/techniques are found to be useful for specific body parts [Table 1].3,5,6,8,9-18,22-26
Size of the lesion
This is one of the important factors, which decides the modality to be followed:
Small-sized patches (1–4 cm): SBT, MPG, STSG, UTSG, and hair follicular grafts (FUT, FUE, or body hair transplantation [BHT]) will give good results. T works equally well in dark individuals preferably if the patch is located on the lip nipple or genitals.
Medium-to-large sized patch: Noncultured epidermal cell suspension (NCECS), UTSG, STSG, Jodhpur technique, and serial MPG done over multiple sittings are the modalities of choice.
Size of punch
The smaller the size of the punch, the better the result. Small sizes of punch (1.0 and 1.5 mm) can be accepted well in all difficult sites of surgery.48
Depth of the punch
The depth of the donor should be less than the depth of the punch removed from the recipient site to prevent cobblestoning.48
Pattern of the shape of the vitiligo lesion
Round or oval – UTSG, NCECS, STSG, MPG, and Jodhpur technique; depending on the size, location of the lesion, and other factors.
Geographical amoeboid with narrow tentacles – MPG, Jodhpur technique, TW (needling), and miniature punch grafts can be inserted between the existing pigmented island
Small remnants – TW (needling [with or without 5-FU cream], TCA, and phenol)
The semi-circular – peri-lesional halo commonly seen after STSG can be successfully re-pigmented by re-grafting with UTSG, STSG, autologous cultured melanocytes, and Jodhpur technique
Small achromic fissures – skip areas or peri graft halo areas around MPG. In all such cases, re-pigmentation can be stimulated by PUVA, PUVASOL, NBUVB, excimer laser/lamp phototherapy, or topical steroid/tacrolimus creams.
Degree of existing hypo/depigmentation in the vitiliginous area
All the residual islands of hypopigmentation should be dermabraded or laser ablated before carrying out any suitable desired procedure as leaving these islands of hypopigmentation in between will result in poor cosmetic outcomes as the resultant color will not match. In MPG also it is advisable to remove these islands and not to graft on them as when these grafts get taken up, there is no spread of pigment in these hypopigmented areas, whereas in achromic areas with MPG, there is a good spread of pigment with complete repigmentation.
Existing color of hair in vitiligo area
If 25–50% of hair is black, then TW will induce good repigmentation in small, medium, or even large-sized vitiliginous areas
For lesions on the scalp with white hair or if there is leukotrichia of eyebrows or eyelashes then FUT, FUE, or BHT or eyelash transplant will achieve good cosmesis
It is observed that vitiligo surgery done by most of the techniques will induce re-pigmentation in 30–60% of existing white hair in the lesion during re-pigmentation of the achromic areas and continue to respond over the next 6 months–2 years.
Set up
Office setup: Most of the procedures can be carried out in an office set up under local anesthesia (LA) or tumescent LA for lesions of any size either in single or multiple serial sessions. Even if patches are large and require short general anesthesia (IV ketamine), they can be managed in an office setup with an operation theater facility
Hospital setup: This is required if regular general anesthesia is required as when lesions are large (extremity) or when it is large and located over sensitive areas (face and genital area) and when immobilization is required (major joints).
Technical support
Tissue culture laboratories are needed for melanocyte culture grafting
Costly devices, such as laboratory equipment (centrifuge, incubator, and chemicals – for traditional method) NCMKCS
CO2 laser and power dermatome (Zimmer) for UTSG
Ultraviolet light units (PUVA/NBUVB) or excimer laser/lamp (308 nm) facility for accelerating re-pigmentation after vitiligo surgery
Same as trypsin inhibitor, Dulbecco’s modified eagle medium (DMEM) medium can also be optional to use in the process of melanocyte transplant.41
Surgical expertise
This is another significant and probably the single most important criterion in selecting the procedure. Some techniques such as MPG or SBT are simple and easy to learn, whereas certain surgical expertise is required to obtain uniformly thin split-thickness grafts for the STSG technique. Similarly, the UTSG technique not only one to obtain ultrathin (0.005/0.1 mm) skin graft but also must acquire the skill to ablate the vitiliginous recipient site using CO2 laser with proper freehand technique to cause dermo-epidermal split (bubbling effect). For retaining grafts over genital areas, one may need expertise to take fine stay sutures to secure the grafts. As discussed so far, similar cosmetic results can be achieved using various modalities and dermatosurgeons may prefer to choose the modality that they are best trained in. A few dermatosurgeons have acquired good skills in multiple techniques. Their long-term experience and expertise will help them in deciding the right surgical method. Some methods may be tedious, time-consuming, and delicate with long learning curves such as FUT, FUE, BTH, and eyelash transplantation, and will require experience, expertise, and vigil. Hence, one must select a method in which one is most comfortable.
CONCLUSION
Summarizing, one can say that various surgical techniques are useful to treat stable vitiligo; however, proper selection of the technique will play a major role in achieving good therapeutic results. Each technique has its advantages and disadvantages. Some may be simple to carry out, while some may cause more side effects. Sometimes, one may have to modify and adapt a few technical variations. Sometimes, more than one technique may have to be carried out in a given patient, such as SBT for lips, MPG for tips, or UTSG or SBT on lips with T at the angles of the mouth. All these permutations and combinations will thus enable the dermatosurgeon to achieve better cosmetic results.
Authors’ contributions
Sushil Savant and Satish Savant contributed to data collection, analysis and interpretation, and drafting of the article. Sushil Savant contributed to critical revision of the article and final approval of the version to be published.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Surgical treatment of vitiligo. Int J Environ Res Public Health. 2022;19:4812.
- [CrossRef] [Google Scholar]
- Standard guidelines of care for vitiligo surgery. Indian J Dermatol Venereol Leprol. 2008;74:S37-45.
- [Google Scholar]
- Surgical therapy of vitiligo: Current status. Indian J Dermatol Venereol Leprol. 2005;71:307-10.
- [CrossRef] [Google Scholar]
- Therapeutic spot and regional dermabrasion in stable vitiligo. Indian J Dermatol Venereol Leprol. 1996;62:139-45.
- [Google Scholar]
- Chemical peeling with phenol: For the treatment of stable vitiligo and alopecia areata. Indian J Dermatol Venereol Leprol. 1999;65:93-8.
- [Google Scholar]
- Autologous miniature punch skin grafting in stable vitiligo. Indian J Dermatol Venereol Leprol. 1992;58:310-5.
- [Google Scholar]
- A novel technique for getting mini thin Thiersch's skin grafts for tiny vitiligo lesions. CosmoDerma. 2022;2:106.
- [CrossRef] [Google Scholar]
- Suction blister epidermal grafting for vitiligo involving angles of lip: Experience of 112 patients. J Cutan Aesthet Surg. 2018;11:13-9.
- [CrossRef] [Google Scholar]
- Vitiligo and the melanocyte reservoir. Indian J Dermatol. 2009;54:313-8.
- [CrossRef] [Google Scholar]
- A comprehensive surgical in vivo study of autologous melanocyte transplant/transfer through ultrathin skin grafting over CO2 ablated lesions supplemented with excimer lamp (308 nm) therapy in stable vitiligo. Indian J Dermatol Venereol Leprol. 2024;90:150-7.
- [CrossRef] [Google Scholar]
- Single-hair follicular unit transplant for stable vitiligo. J Cutan Aesthet Surg. 2011;4:41-3.
- [CrossRef] [Google Scholar]
- Follicular unit extraction as a therapeutic option for vitiligo. J Cutan Aesthet Surg. 2013;6:229-31.
- [CrossRef] [Google Scholar]
- Eyelash transplantation for the treatment of vitiligo associated eyelash leucotrichia. J Cutan Aesthet Surg. 2016;9:97-100.
- [CrossRef] [Google Scholar]
- Long-term follow-up of leucoderma patients treated with transplants of autologous cultured melanocytes, ultrathin epidermal sheets and basal cell layer suspension. Br J Dermatol. 2002;147:893-904.
- [CrossRef] [Google Scholar]
- Autologous noncultured melanocyte-keratinocyte transplantation in stable vitiligo: A randomized comparative study of recipient site preparation by two techniques. Indian J Dermatol Venereol Leprol. 2019;85:32-8.
- [CrossRef] [Google Scholar]
- Autologous non-cultured melanocytekeratinocyte transplantation in the treatment of vitiligo: Patient selection and perspectives. Clin Cosmet Investig Dermatol. 2018;11:521-40.
- [CrossRef] [Google Scholar]
- A study of non-cultured extracted hair follicle outer root sheath cell suspension for transplantation in vitiligo. Int J Trichol. 2016;8:67-72.
- [CrossRef] [Google Scholar]
- Cultured epidermal melanocyte transplantation in vitiligo: A review article. Iran J Public Health. 2019;48:388-99.
- [CrossRef] [Google Scholar]
- Efficacy and safety of autologous cultured melanocytes delivered on poly (DL-lactic acid) film: A prospective, open-label, randomized, multicenter study. Dermatol Surg. 2012;38:1981-90.
- [CrossRef] [Google Scholar]
- Keratinocyte-Melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:622-4.
- [CrossRef] [Google Scholar]
- Vitiligo surgery: Which? where? why? textbook of dermatosurgery and cosmetology principles and practice Vol 48. (3rd ed). Mumbai, India: Bhalani Publishing House; 2018. p. :623-7.
- [Google Scholar]
- Ultrathin split-thickness skin grafting followed by narrowband UVB therapy for stable vitiligo: An effective and cosmetically satisfying treatment option. Indian J Dermatol Venereol Leprol. 2012;78:159-64.
- [CrossRef] [Google Scholar]
- Tissue grafts in vitiligo surgery-past, present and future. Indian J Dermatol. 2009;54:150-8.
- [CrossRef] [Google Scholar]
- Comparative study of micro-needling combined with topical 5-flurourocil versus Microneedeling alone in treatment of localized stable vitiligo. I. J Dermatol. 2021;66:574.
- [CrossRef] [Google Scholar]
- Microskin grafting for stable vitiligo of the penis and vulva: Near total uniform pigmentation. J Cutan Med Surg. 2015;19:477-83.
- [CrossRef] [Google Scholar]
- Excellent color-matched repigmentation of human vitiligo can be obtained by mini-punch grafting using a machine in combination with ultraviolet therapy. Dermatol Sin. 2018;36:203-6.
- [CrossRef] [Google Scholar]
- Transverse needling after autologous mini-punch grafts improves repigmentation in stable non-segmental vitiligo. Clin Cosmet Investig Dermatol. 2021;14:827-35.
- [CrossRef] [Google Scholar]
- Suction blister epidermal graft (SBEG)-An easy way to apply this method. J Dtsch Dermatol Ges. 2019;17:468-71.
- [CrossRef] [Google Scholar]
- Syringes versus Chinese cups in harvesting suction-induced blister graft: A randomized split-body study. Int J Dermatol. 2018;57:1249-52.
- [CrossRef] [Google Scholar]
- Modified technique of suction blistering for epidermal grafting in vitiligo. Int J Dermatol. 1999;38:306-9.
- [CrossRef] [Google Scholar]
- The CelluTome epidermal graft-harvesting system: A patient-reported outcome measure and cost evaluation study. Int Wound J. 2017;14:555-60.
- [CrossRef] [Google Scholar]
- A prospective, multicentre study on the use of epidermal grafts to optimise outpatient wound management. Int Wound J. 2017;14:241-9.
- [CrossRef] [Google Scholar]
- Epidermal skin grafting in vitiligo: A pilot study. Int Wound J. 2016;13:47-51.
- [CrossRef] [Google Scholar]
- Efficacy of suction blister epidermal grafting with concomitant phototherapy in vitiligo treatment. Postepy Dermatol Allergol. 2018;35:592-8.
- [CrossRef] [Google Scholar]
- Treatment of stable vitiligo with autologous epidermal grafting and PUVA. J Am Acad Dermatol. 1995;32:943-8.
- [CrossRef] [Google Scholar]
- Long term follow up study of segmental and focal vitiligo treated by autologous non-cultured melanocyte-keratinocyte cell transplantation. Arch Dermatol. 2004;140:1211-5.
- [CrossRef] [Google Scholar]
- Jodhpur technique In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549891 [Last accessed on 2024 May 05]
- [Google Scholar]
- A systematic review of autologous transplantation methods in vitiligo. Arch Dermatol. 1998;134:1543-5.
- [CrossRef] [Google Scholar]
- Ultra-Thin skin grafting (UTSG) (melanocyte transplant/transfer) In: Textbook of dermatosurgery and cosmetology principles and practice Vol 45. (3rd ed). Mumbai: Bhalani Publishing House; 2018. p. :585-95.
- [Google Scholar]
- Grafting in vitiligo: How to get better results and how to avoid complications. J Cutan Aesthet Surg. 2013;6:83-9.
- [CrossRef] [Google Scholar]
- The use of cyanoacrylate glue for skin grafts stabilisation: A retrospective multicenter study. Int Wound J. 2023;20:79-84.
- [CrossRef] [Google Scholar]
- Cyanoacrylate: A handy tissue glue in maxillofacial surgery: Our experience in Alexandria, Egypt. J Maxillofac Oral Surg. 2013;12:243-7.
- [CrossRef] [Google Scholar]
- Surgical wound repair with innovative hemostatic glue: Clinical case report. Appl Sci. 2023;13:8979.
- [CrossRef] [Google Scholar]
- The advantages in using cyanoacrylate glue over skin staples as a method of skin graft fixation in the pediatric burns population. Ann Chir Plast Esthet. 2018;63:323-9.
- [CrossRef] [Google Scholar]
- Cyanoacrylate surgical glue as an alternative to suture threads for mesh fixation in hernia repair. J Surg Res. 2010;163:e53-8.
- [CrossRef] [Google Scholar]
- Axillary incubator for cell-based therapies in vitiligo. J Am Acad Dermatol. 2021;85:e279-80.
- [CrossRef] [Google Scholar]
- Chapter 4: Punch grafting In: Dermatologic surgery made easy. New Delhi, India: Jaypee Digital Explore Health Sciences; 2006.
- [CrossRef] [Google Scholar]






