Translate this page into:
Practice Points from Prof. Lawrence M. Field—Father of Modern Dermatosurgery: Bi-level anesthesia and blunt dissection
Address for correspondence: Dr. Nilesh N. Goyal, Lilavati Hospital, Bandra West, Mumbai 400050, Maharashtra, India. E-mail: getyoung@juvenis.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Keywords
Prof. Lawrence Field
bi-level anesthesia
blunt dissection
Dear Derma colleagues,
Today we are expanding our horizons of dermatosurgical skills, searching for newer surgical techniques, and going into deeper territories. Our surgical techniques can be refined by reviewing what our masters have done many decades ago. Prof. Lawrence Marshall Field, who has rightly been conferred upon as the Father of Modern Dermatosurgery, has written about many techniques in dermatosurgery which we follow today. With his passing on 2 October 2020, we have lost a phenomenal teacher who lived and traveled to teach dermatosurgery across the world over the last three decades. He was a true inspiration for the coming generations to teach and learn from each other the principles of dermatosurgery. He firmly believed that “to teach is to touch a life forever.” Today there are dermatologists in more than 70 countries who have learnt from him and are mourning his passing.
CONCEPT OF BI-LEVEL ANESTHESIA
His concept of bi-level anesthesia gave many a dermatosurgeon the confidence to enter the subcutaneous plane boldly and perform skin surgery comprehensively [Figure 1]. This involves anaesthetizing the subcutaneous space followed by surface anesthesia resulting in complete anesthesia of the surgical area. This is then combined with blunt deep dissection. It is by far the safest surgical technique for any and all cutaneous surgery including skin cancer surgery, liposuction, and hair transplant.[1] The technique has also been used in modern day procedures like deep chemical peeling, dermabrasion, laser resurfacing, excisions of large moles, and scar revisions.
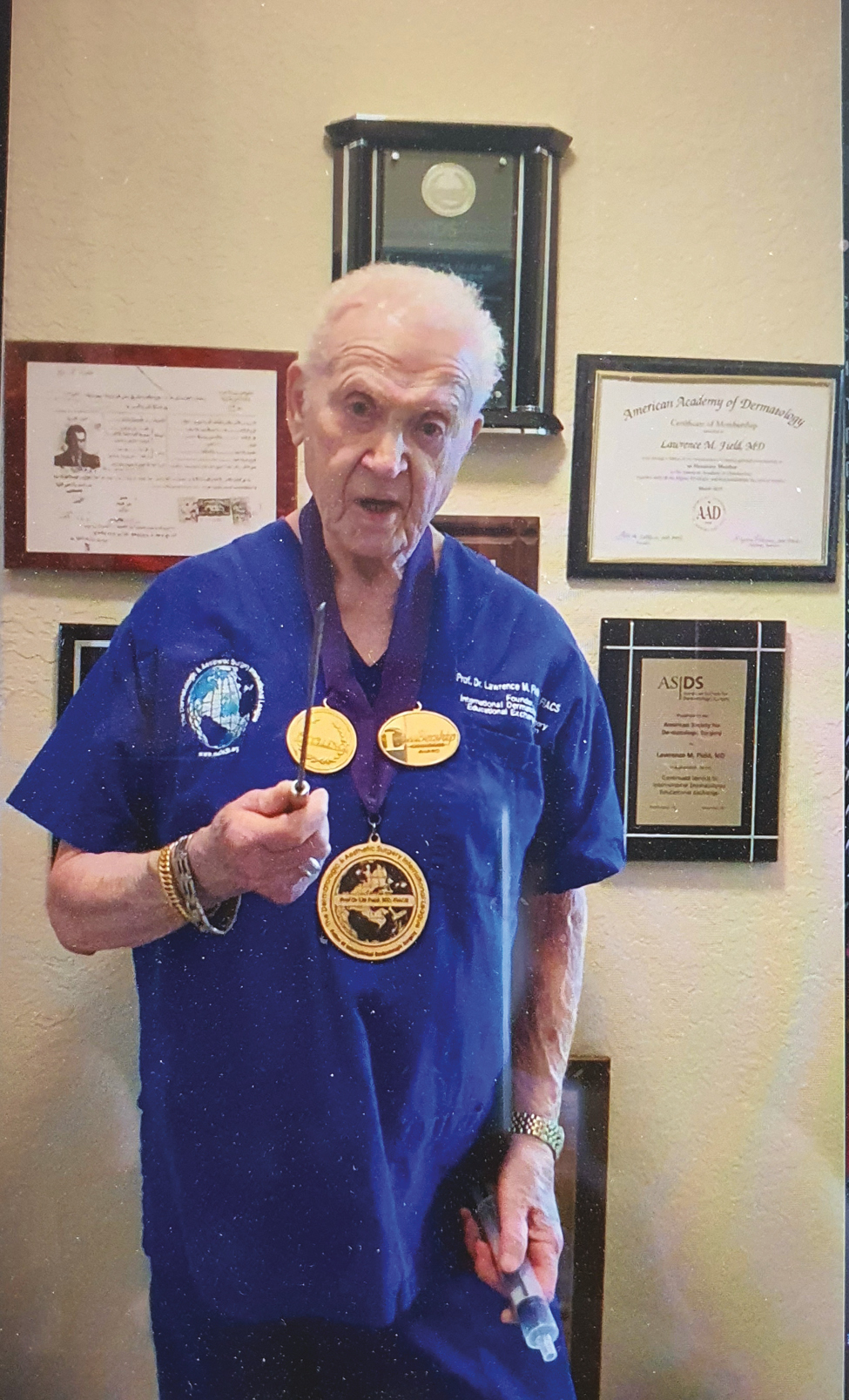
- Prof. Lawrence Field (1929–2020) explaining the concept of bi-level tumescent anesthesia and blunt dissection
TECHNIQUE
It involves injecting a solution of tumescent anesthesia prepared prior to surgery into the subcutaneous plane via a puncture wound. The entry point is anesthetized with a mix of Lidocaine 2% with Adrenaline 1:200,000. This entry can be made using a round punch 2–3 mm or a 11 No. surgical blade. The Tumescent anesthesia solution is based upon Klein's formula (normal saline 1000 cc + Lidocaine 2% 10–75 mL + Adrenaline 1:1000 0.5–1 mL + sodium bicarbonate 8.4 meq/L 10 mL).[2] This solution is slowly injected using a blunt multiport infiltrator (1–2 mm). The solution is placed under the entire surgical area. The fluid is injected while withdrawing the infiltrator (retrograde infiltration). Hydrodissection occurs under the skin lesion with separation from the deeper vital structures. Often the entire surgical area can be anaesthetized from a single port of entry. A good estimate of the depth of the skin lesion can be got during infiltration by palpating the spread of fluid. A uniform rise in the skin lesion would rule out a deeper tissue involvement. Once the area is anaesthetized, the dermoepidermal junction is further anaesthetized with Lidocaine 2% without adrenaline given intradermally along the line of incision. This is usually less discomforting now that the tumescent anesthesia should have begun its action.[3] A complete anesthesia of the entire lesion including the incision line helps in relaxing the patient and allows uninterrupted progress of surgery.
A clean incision using a 15 No. surgical blade on Bard Parker handle no. 3 can allow entry into the deeper plane. The surgeon has to incise up to lower dermis. A blunt dissecting scissors can be used for separating the skin lesion from the underlying structures. Very less resistance is encountered if tumescent anesthesia is employed correctly. Blunt dissection using blunt scissors or a blunt-ended needle holder or a blunt-tipped cannula prevents any surgical damage to underlying structures with minimal disruption of fat compartment which in turn promotes faster healing and minimal scarring.
ADVANTAGES OF BI-LEVEL ANESTHESIA
A very big advantage of the Bi-level technique is that it causes a tamponade of the subdermal blood vessels which makes the surgical field blood less and hence surgeon friendly. The need for electrocautery to seal oozing vessels is significantly reduced.[3] In the author's opinion, this reduces the amount of eschar within the surgical wound encouraging better healing. Hemostatic techniques required for the larger deeper vessels are far less time consuming. Subdermal infiltration separates the cutaneous nerves from the skin overlying avoiding their accidental severance during the incision. In addition, surface anesthesia gives complete numbing of pain and keeps patient comfortable. Tumescent anesthesia in the subcutaneous layer gives long-lasting anesthesia due to the high affinity of adipocytes for lidocaine and its slow release into the systemic circulation thereby slowing its metabolic degradation. This prolonged anesthesia helps the surgeon to perform smoothly and rapidly as the patient is completely relaxed and at the same time is awake and cooperative. A personal communication from Dr. Klein is that tumescent lidocaine solution probably has an antimicrobial effect as none of his 8000 plus patients who underwent tumescent anesthesia for liposuction encountered any infections post operatively.[2]
It is very difficult to think about any possible disadvantage of this vital technique which makes dermatosurgery very safe and easy such that a novice could undertake it.
The author has benefitted very much from adopting this approach for excising lesions on scalp and neck[34] [Figures 2–4]. It has proven invaluable while performing an ablative CO2 laser procedure for multiple angiokeratomas involving a large area of scrotum and for dermabrasion of cheeks for acne scars. It has definitely made hair transplant surgery very comfortable for the patients as the level of anesthesia is optimum for them to be relaxed and pain free. The taut subcutaneous space helps in keeping the hair erect making extraction easy with fewer transections.[56]
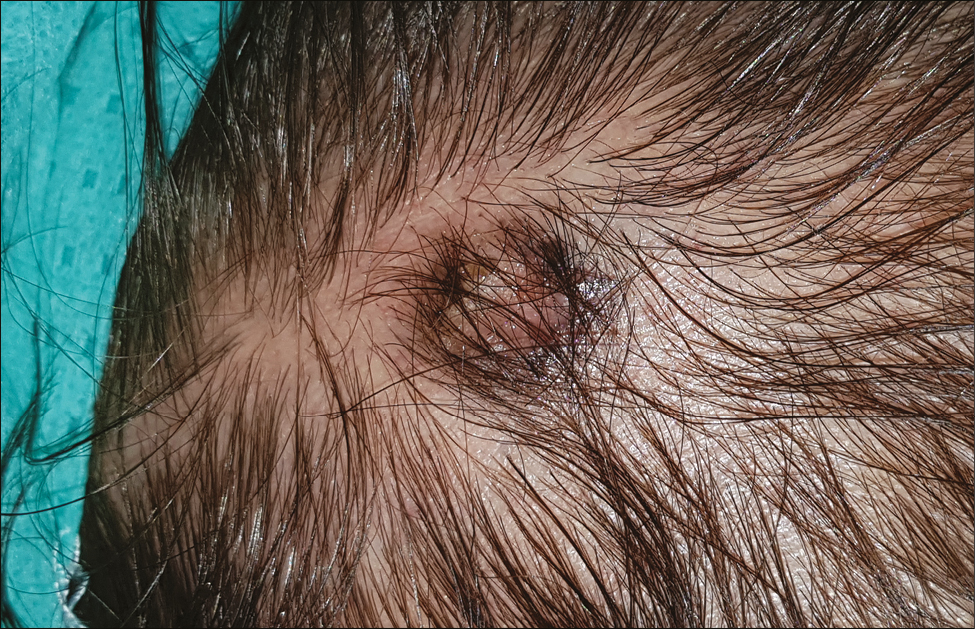
- Basal cell carcinoma on temporal scalp pre infiltration
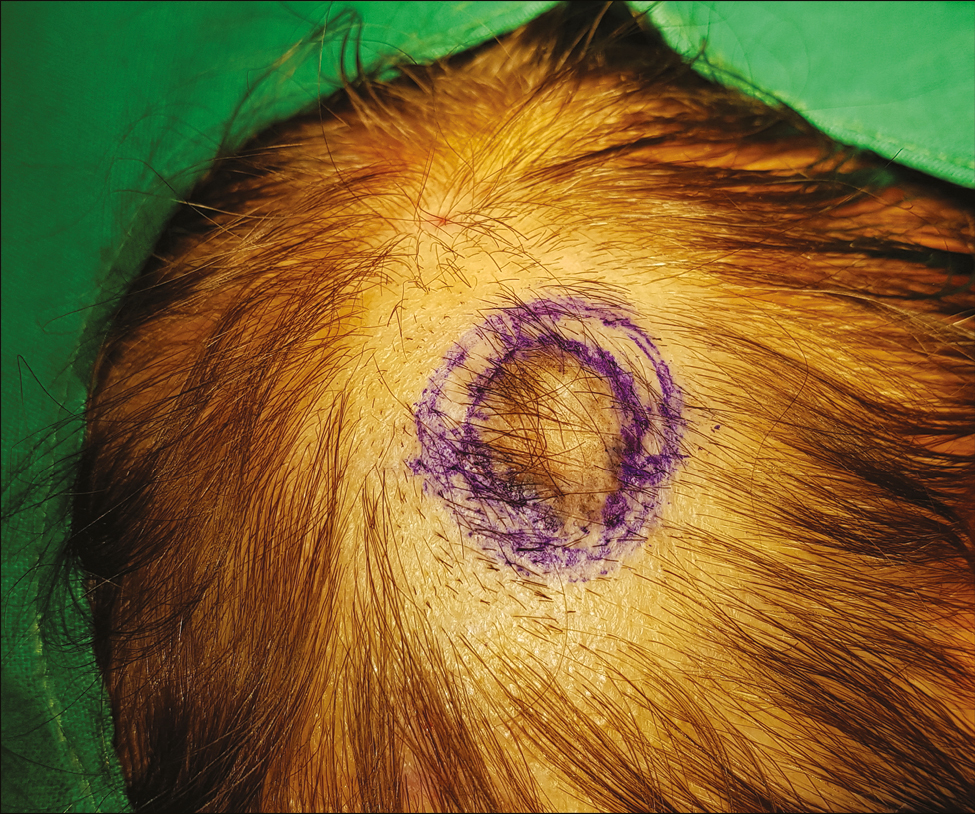
- Bi-level tumescent anesthesia showing pale skin around the lesion with lifting of the lesion

- Blunt-tipped 2 mm infiltration cannula with multiple ports
Points to learn and adopt
Bi-level anesthesia helps in separating the operating skin from the deeper vital structures keeping the surgeon safe. It ensures complete anesthesia of the skin and surrounding tissues.
Blunt dissection with blunt-tipped scissors or cannula in deeper planes causes less damage to fat compartment resulting in better and faster healing.
Tamponade effect of tumescent anesthesia results in blood less surgical field.
Long-lasting anesthesia with tumescent technique avoids overuse of pain killers and anxiolytics.
Most dermatological and cosmetic procedures can be done with ease by using the Bi-level technique of anesthesia.
Prof. Lawrence M. Field called this technique of “surgical tumescent anesthesia” as an extension of the concept of “tumescent anesthesia” which was an invention by Dr Jefferey A. Klein. He promoted this at dermatosurgical meetings throughout the world in the last two decades. We owe him sincere gratitude for his unrelenting efforts over four decades to spread dermatosurgery across the global dermatology fraternity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Bilevel anesthesia and blunt dissection: Rapid and safe surgery. Dermatol Surg. 2001;27:989-91.
- [Google Scholar]
- Use of the tumescent technique for scalp surgery, dermabrasion, and soft tissue reconstruction. J Dermatol Surg Oncol. 1992;18:130-5.
- [Google Scholar]
- Harvesting split-thickness grafts with tumescent anesthesia. Dermatol Surg. 1997;23:62.
- [Google Scholar]
- Bilevel tumescent anesthetic infiltration for hair transplantation. Dermatol Surg. 1997;23:289-90.
- [Google Scholar]






