Translate this page into:
Proliferating Trichilemmal Tumor of Scalp: Benign or Malignant, A Dilemma
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Proliferating trichilemmal tumor (PTT) is a well-circumscribed dermal or subcutaneous neoplasm with squamoid cytologic features and trichilemmal-type of keratinization.[1] This neoplasm was first recognized by Wilson-Jones[2] in 1966 as an entity that had the histologic capacity to simulate squamous cell carcinoma. Different terminologies have been used to describe this tumor, namely epidermoid cyst, pilar tumor of the scalp, proliferating trichilemmal cyst, proliferating epidermoid cyst, giant hair matrix tumor, hydatidi form keratinous cyst, trichochlamydocarcinoma, and invasive hair matrix tumor.[3] PTT has been classified into three groups: benign, locally aggressive, and malignant.[4] Herein, we report a case of well-differentiated low-grade malignant PTT due to its rarity.
A 25-year-old lady presented to the dermatology outpatient department with an itchy, red swelling over fronto-temporal part of the scalp for 1 year. There was history of similar swelling over the same site 2 years back which she got excised from outside. This time the swelling recurred and started as a pea-sized lesion and over the next 5-6 months, it suddenly increased to attain the present size. The patient did not give history of preceding trauma. The examination revealed a single, hard, erythematous swelling of 3×4 cm size over the left fronto-temporal scalp with overlying alopecia [Figure 1]. It was not fixed to the underlying bone. There was no regional lymphadenopathy. Systemic examination was normal. We got the lesion excised with a 2 cm margin of normal skin in view of recurrence. Microscopic examination of the excised lesion revealed proliferating nests of squamoid cells throughout the dermis, separated by fibrous stroma. There were areas of keratinization and necrosis [Figure 2]. The tumor cells were infiltrating skeletal muscle [Figure 3]. Abrupt keratinization was not seen. Features of anaplasia (increase in the nucleo-cytoplasmic ratio, nuclear hyperchromasia or nuclear polymorphism and mitotic figures) were not seen on examination of multiple sections of the excised specimen. The resected surgical margins of the mass were free of tumor. Based on the histopathological findings, the diagnosis of low-grade, well-differentiated malignant PTT was made. Chest roentgenogram did not reveal any evidence of pulmonary metastasis. Contrast-enhanced CT scans of the brain also did not reveal intracranial invasion. Ultrasound of abdomen as well as kidney, ureter, and bladder were normal. The patient is under follow-up for the past 1 year of surgical excision and there is no recurrence so far [Figure 4].

- A single hard, erythematous nodular swelling 3 × 4 cm present over right fronto-temporal aspect of scalp.
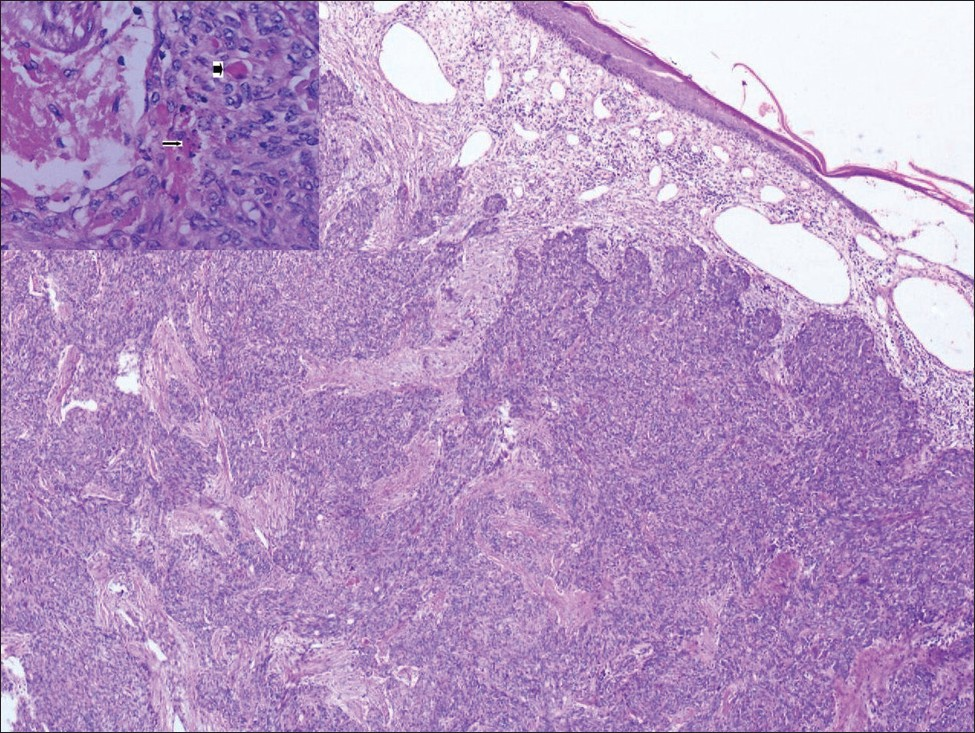
- Low power view of tumor in dermis consisting of proliferating nests of squamoid cells separated by fibrous stands (H&E ×100). Inset {High power view of tumor showing foci of keratinization and areas of necrosis (H&E ×400)}.
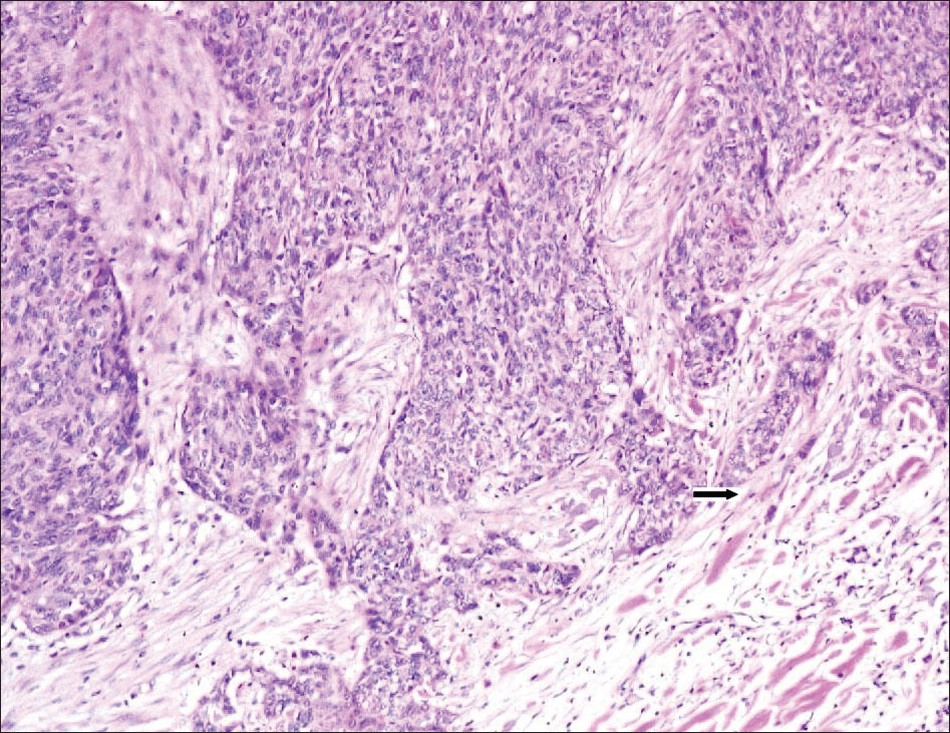
- Deeper margins of the tumor showing small nests of tumor cells infiltrating the skeletal muscle (H&E ×400).

- Post-surgical excision clinical photograph.
PTT is more commonly seen in women. Lanugo hair follicles of the bald scalp and follicles of other areas devoid of non-terminal hair are unlikely to produce these tumors. Therefore, pilar tumors are not seen in the bald scalp, being more common in areas with excess hair growth.[5] PPT is usually benign and rarely may undergo malignant transformation in a step-wise manner starting with an adenomatous stage of the trichilemmal cyst to an epitheliomatous stage of the PTT evolving into the carcinomatous stage of the MPTT.[6] In the present case, functionally, the tumor was malignant for it showed features of rapid growth, invasion; and morphologically it depicted foci of necrosis. However, anaplasia was not seen. Malignant and benign tumors can be differentiated on the basis of morphological criteria, i.e. rate of growth, invasion and metastasis, and functional criteria, i.e. anaplasia and cellular atypia. Anaplasia, if found, is hallmark of malignancy, but cellular atypia and anaplasia may be surprisingly absent in some cases.[7] Metastasis from malignant PTT has only rarely been reported. Seff and Berkowitz reported two cases which metastasized several times to neck nodes, the patient subsequently dying of disseminated disease.[8] Another report had also described a rare malignant variant of the PTT, with an aggressive clinical course and a propensity for nodal and distant metastases.[5] According to these basic principles of pathology, the present case was functionally malignant morphologically benign though. A clinicopathological study of 76 cases divided PPT into three groups on the degree of stromal invasion and the level of cellular atypia: benign, low- and high-grade malignant. Group I included those patients who showed no infiltration of surrounding stroma and minimal nuclear atypia; they showed trichilemmal keratinization, stromal invasion with a mononuclear infiltrate of plasma cells and lymphocytes, and dystrophic calcification and were considered as benign tumors. Group II tumors were composed of multiple lobulated and bosselated expansive masses of squamous epithelium separated by loose edematous stroma and filled centrally with homogeneous acellular eosinophilic material representing amorphous debris and pilar keratin. In addition, the squamoid tumor cells manifested large, hyperchromatic nuclei with irregular nuclear membranes surrounded by abundant eosinophilic cytoplasm. Foci of single cell necrosis and abrupt keratinization were identified. Cords of atypical squamous epithelium extended into the surrounding dermis, with a desmoplastic stromal response. There was a lack of marked cytologic atypia in group 2 PPTs. A minimal to moderate infiltrate of mononuclear inflammatory cells was identified as well. Group III tumors were invasive; they were cytologically anaplastic and were therefore considered malignant.[4] The present case was classified as group II, considering the invasive property, foci of necrosis and lack of cellular atypia. The classification, however, does not take account of the clinical behavior, which may surprisingly be independent of the histopathology of any neoplasm.[7] Besides, malignant transformation of a PPT can be manifested by sudden, rapid growth.[9] Thus, it is imperative to take cognizance of not only the morphological but the functional features of a tumor as well and manage the tumor accordingly. In the present case, it was thought to be either an early malignant of a locally aggressive form of PPT in view of its recurrent nature, invasion of skeletal muscle, and foci of necrosis on microscopy. Therefore, it was excised completely with a 2 cm margin. Mohs micrographic surgery, which ensures precise lesion margin control, may be undertaken to reduce the recurrence and metastasis rate after tumor resection.[1011]
REFERENCES
- Cutaneous adnexal tumors: A guide to pathologic diagnosis. Chicago, IL: ASCP Press; 1991. p. :113-68.
- Proliferating trichelemmal cyst: A simulant of squamous cell carcinoma. Cancer. 1981;48:1207-14.
- [Google Scholar]
- Proliferating pilar tumors: A clinicopathologic study of 76 cases with a proposal for definition of benign and malignant variants. Am J Clin Pathol. 2004;122:566-74.
- [Google Scholar]
- Development of a malignant proliferating trichilemmal cyst in a patient with multiple trichilemmal cysts. Dermatologica. 1983;166:203-8.
- [Google Scholar]
- Malignant proliferating trichilemmal tumour presenting early in life: An uncommon feature. J Cutan Aesthet Surg. 2011;4:51-5.
- [Google Scholar]
- Neoplasia. In: Kumar V, Abbas AK, Fausto N, Aster J, eds. Robbins and Cotran Pathologic Basis of Disease (8th ed). New Delhi: Elsevier; 2010. p. :173-223.
- [Google Scholar]
- Carcinomatous degeneration of sebaceous cysts. Surg Gynecol Obstet. 1916;33:469-73.
- [Google Scholar]
- Proliferating trichilemmal tumors: Clinicopathologic evaluation is a guide to biologic behavior. J Cutan Pathol. 2003;30:492-8.
- [Google Scholar]
- Mohs’ micrographic surgery of a proliferating trichilemmal tumor in a young black man. Dermatol Surg. 2005;31:359-63.
- [Google Scholar]
- Proliferating trichilemmal tumors: A review of the literature. Dermatol Surg. 2007;33:1102-8.
- [Google Scholar]





