Translate this page into:
Prospective Study of Flap Surgery-Related Complications in Cutaneous Tumors: A Tertiary Care Institutional Experience of 6 Years
Address for correspondence: Dr. Shilpa Kanathur, Department of Dermatology, Bangalore Medical College and Research Institute, No 53, Bengaluru, Karnataka, India. E-mail: shilpakvinod1980@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
Flap surgeries are the standard choice for reconstruction of defects post excision of cutaneous tumours. Complications following these surgeries predominantly result as a consequence of bleeding, tension, ischemia, infection.
Study Design:
A Prospective study of patients treated for tumor excision and flap reconstruction between the period of 2014 and 2020 were followed up and complications encountered were analysed.
Results:
A total of 70 patients with cutaneous malignancies underwent flap surgeries. Complications encountered were bleeding, hematoma, infection, necrosis, pincushioning, keloid, hypertrophic scars.
Conclusion:
Successful outcome depends on pre operative evaluation, appropriate technique selection based on site of tumor, intraoperative care, post operative care and timely management of complications if any.
Keywords
Bleeding
flaps
infection
scars
INTRODUCTION
Incidence of skin cancers has progressively increased over years in significant proportion.[1] In India, the incidence of skin malignancies is low constituting about 1–2% of all the diagnosed cancers.[2] Local flaps are the first treatment of choice for reconstruction of defects following excision of these malignancies. Apart from malignancies many nevoid, benign and hamartomas also sometime require flap reconstruction. They provide good functional and cosmetic results with respect to color, texture match and more importantly good success rate and uptake with proper skillful surgical execution. However, as with any surgical intervention, complications from these procedures are expected to occur due to their location, tissue dissection, mobility during the surgery, co-morbidities. It also requires a time lap for the tissue graft to stabilize and restore functionality.
A complication is defined as an adverse event that is not considered to be a common or usual occurrence, which may require some modification in the technique used. These complications may have poor aesthetic and functional outcome. Complications may arise during the surgery or in the early or late postoperative phases.
The present study documentation was performed during the follow up period of all the flap surgeries performed in our institute. We intend to report the type and frequency of complications occurring during or after procedure and have also reviewed the literature regarding the cause and prevention of such complications.
MATERIALS AND METHODS
All the patients with biopsy proven cutaneous tumors who underwent flap surgeries between the period of 2014 and 2020 were followed up for a period of one year. The follow up were scheduled post operatively at 48 hours, 5–7 days, 2 weeks, one month, six month and at the end of one year. During follow up, patients were assessed for any early and late complications. Appropriate measures were taken to manage these complications for better functional and aesthetic outcome.
RESULTS
A total of 70 patients with cutaneous tumors underwent flap surgeries during the study period. Out of which 58 were on head and neck area, 4 on extremities, and 8 cases on trunk. Out of 70 total cases, 45 cases were confirmed with Basal cell carcinoma (BCC), 8 cases with Bowens disease and Squamous cell carcinoma (SCC) each, 3 cases with porocarcinoma 2 cases with dermatofibroma and nevus sebaceous each, one case with tuberous xanthoma, mucinous cyst was each.
The local cutaneous flap techniques performed were single rotation in 30 patients, rhomboid in 9 patients, unipedical advancement flap in 10 patients, double rotation in 4 cases, triple rotation one case, A to T flap in 5 cases, VY advancement flap in 4 cases, H-flap in 5 cases and cresentric excision in 2 patients.
The various complications that were observed in our study are classified into intra operative, post operative and late complications. The most common intraoperative complication was increased bleeding during surgery in three patients who were hypertensive and anxious. In post operative period of one week, the complications encountered include hematoma in one patient, tip necrosis in 2 patients, full thickness necrosis in 2 patients, temporary facial nerve paresis, Ectropion due to eyelid retraction in a BCC case very close to eye was observed in one patient.
Late complications include hypertrophic scar in two patient, pincushioning deformity in two patients and recurrence in completely excised BCC was seen in on patient. All patients with complications were managed appropriately to provide optimum results.
Complications
The various complications noted, their management and outcome are enlisted in the [Table 1].
| Time of complication | Type of complication | Number | Management | Outcome |
|---|---|---|---|---|
| Intraoperative | Bleeding | 3 | Preoperative anxiolytics, blood pressure control, compression, ligation of bleeding vessel, and electrocautery | Good |
| Postoperative immediate complications |
Infection | 0 | Aseptic precautions Antibiotics Drainage of pus if any |
Good |
| Hematoma | 1 | Drainage of collected blood | Resulted in necrosis | |
| Odema | 2 | Anti-inflammatory drugs | Good | |
| Necrosis |
4 | Debridement followed by PRP and PRF dressing | Scarring | |
| Anatomical effects | 1 | Excision and free skin grafting (ectropion) | Functional diability | |
| Late complications |
Hypertrophic scar |
2 | Intralesional steroid | Flattening of scar |
| Pin cushioning |
2 | Intralesional steroid | Improved cosmetic outcome | |
| Recurrence |
1 | Early detection and excision | Good |
DISCUSSION
Complications are a known sequelae of a surgery which needs to be well anticipated and avoided. The complications most often result from ischemia, tension-related, and infectious causes. It can occur intraoperatively, immediate or late post operatively.
Intra operative complications
Bleeding
Perioperative excessive bleeding is an expected and most common complication of any surgery.[3]Flap surgery which involves large areas of tissue dissection can pose a risk of increased bleeding. The amount of bleeding depends on patient’s general condition, use of blood thinners, the site of surgery, plane of dissection, and the dermatological condition for which flap is being planned. Hypertensive patients are at increased risk of bleeding and also use of epinephrine is controversial in these patients due to risk of hypertensive crisis during surgery. Anxious patients tend to bleed more during surgery. Scalp and face being highly vascular increases the risk. In scalp if plane of dissection is more superficial, then the risk of bleeding is high and highly vascular lesions tend to bleed more during excision.
Blood pressure should be brought under control before taking up for surgery. Anxiolytics should be started in anxious patients prior to the surgery. Tranexemic acid can be used pre and intraoperatively to reduce bleeding.[4] Regular monitoring of vital should be done during the procedure. In areas like scalp plane of dissection should be at the level of galea aponueritica to reduce intraoperative bleeding. Tumescent anaesthesia should be used in areas with excessive bleeding. Capillary bleeding can be managed with gentle pressure. Venous or arterial bleeds require ligation or electrocautery. Dermatosurgeon should be equipped with electrosurgical cautery for adequate haemostasis.
In our study we had three hypertensive patients with increased bleeding that was managed with compression and electrocautery. Out of three two were on scalp and one on face. All cases were done under tumescent anaesthesia. All elderly patients on anti coagulants were asked to continue anti coagulants. However temporary interruption of anticoagulation may be required in certain circumstances based on the patient’s and procedure’s individualized risks and benefits.[5]
Oedema
Oedema is an expected complication during flap surgery because of excess tissue dissection which resolves without any sequelae. However it can become problematic in area like eyelids obstructing the vision. Mild oedema can be managed with anti-inflammatory drugs. In our study we had two cases of severe oedema of eyelid [Figure 1] which subsided within 3 to 5 days.

- Edema of eyelid obstructing the vision
Infection
Failure to take aseptic precautions and diabetes increases the risk of infection. In our study 8 patients were known diabetics on medications. Patients were taken up for surgery only after diabetic status was under control. By following strict aseptic precautions we did not encounter any infection in flap cases.
Necrosis
Causes of flap necrosis are varied. Inadequate vascularity and venous congestion are the main contributing factors. Venous Doppler studies have shown that smoking and tobacco chewing drastically reduces blood supply to flaps. It is advisable to stop smoking and tobacco chewing 2 weeks before and after flap surgery.[6]
Other causes include error in judgement and planning by surgeons. Too small flap for the defect, creating a flap that extends beyond capillary-filling pressure, not following the recommended length width ratio, degree of rotation are some of the technical errors from surgeon side leading to flap necrosis.
Other technical errors include increased tension along suture lines, inadequate haemostasis, hematoma and direct damage to sub epidermal plexus. Adequate haemostasis should be achieved before closing the flap. Dusky red or bluish discoloration of flap with swelling underneath is the early sign of hematoma. Small hematomas under large flap may get tolerated well however large hematoma damages the flap by releasing toxic free radicals. Such hematomas should be drained by removing few sutures. We encountered hematoma in one case of rotational flap who presented very late to us which resulted in flap necrosis.
Too small flap for the defect will lead to increased tension especially in distal part of the flap compromising vascularity. Pedicle of the flap should be wide enough to ensure adequate blood supply. While raising the flap care should be taken not to damage subdermal plexus. Flap thickness should be neither too thin not too thick. Raising too thin flap can damage subdermal plexus. Flaps should be raised in facelift plane to ensure blood supply from subdermal plexus.[7]
While designing the flap, various factors have to be kept in mind. Lesions with high malignant potential and at risk of recurrence need to be resected with wide margin. In such cases, skin has to be mobilised from the adjacent area. The adjacent area has to be assessed regarding laxity of skin, anatomical landmark, adjacent vital structures and resting skin tension lines (RSTL). Tension free closure is a fundamental requirement. Elderly patients with lax skin are the ideal candidates for flaps. Younger patients with large lesion and tight surrounding skin should be considered for alternate methods like grafts or tissue expanding techniques. For areas around the joints, with great mobility and decreased laxity keystone flaps can be considered.[8]
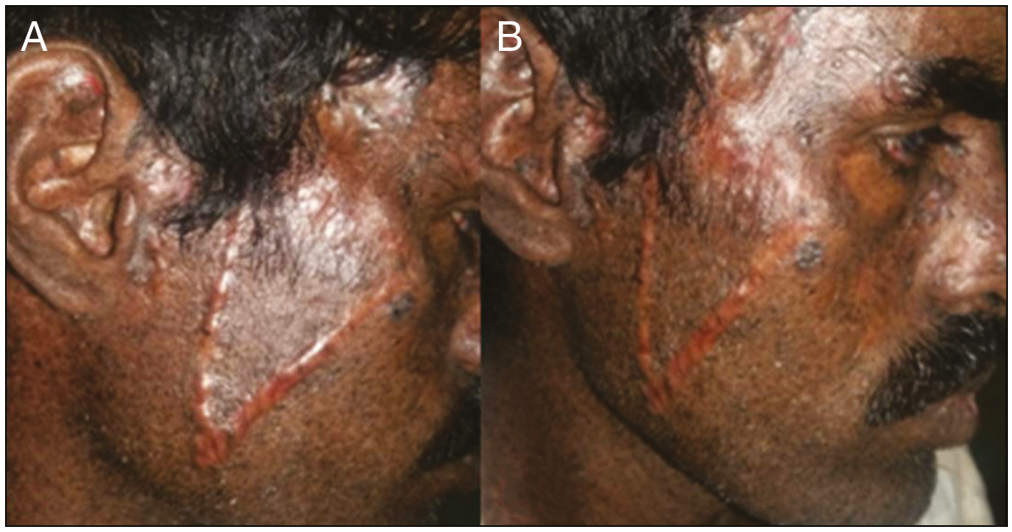
Infections, mobile areas around joints, areas with reduced vascularity, delayed wound healing due to diabetes are the other predisposing factors for flap necrosis. In our experience, we had four cases of flap necrosis. One was superficial tip necrosis due to increased tension on forehead which healed well [Figure 2A and B], second in a diabetic patient which healed with secondary intension with minimal scarring [Figure 3A and B], another due to haematoma and last due to non yielding surrounding skin and mobile area of the joint in a young boy which healed with unacceptable hypertrophic scar [Figure 4A and B].
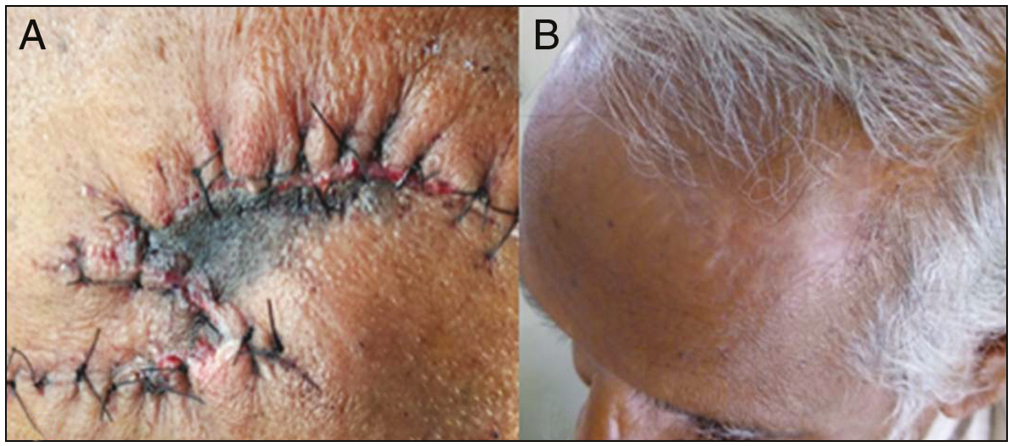
- (A) Tip necrosis in double rotational flap due to acute angle of rotation. (B) Very well healed scar following superficial tip skin necrosis
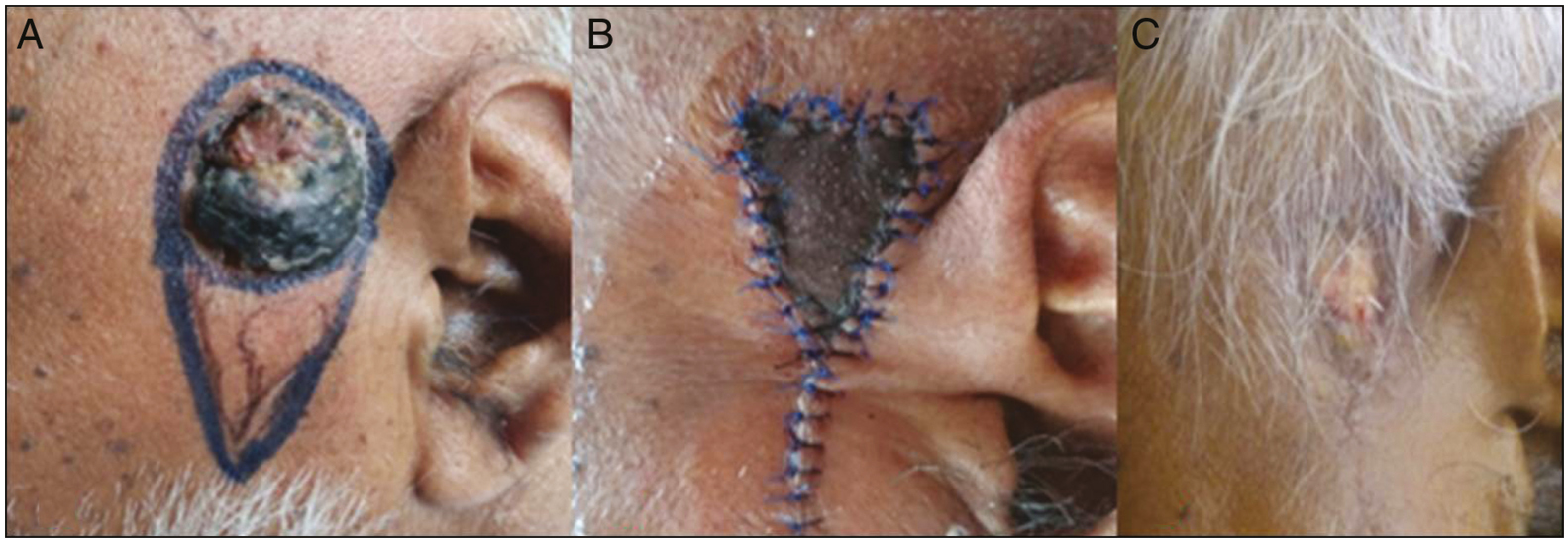
- (A–C) Full-thickness flap necrosis healed with secondary intention

- (A and B) Full-thickness flap necrosis healing with hypertrophic unacceptable scar
Impending flap necrosis should be identified early by discolouration of flap. Hematomas should be evacuated as described above. In case of pale flap which indicates compromised vascularity due to increased tension should be managed by releasing few sutures to reduce tension. Pinprick test is very useful in assessing flap perfusion.[9]
Once necrosis has occurred unhealthy tissue and slough should be removed, regular dressing to be done. Care should be taken to avoid secondary infection. Defects left behind can be managed with skin graft, or alternative flap or allowed to heal with secondary intension. Platelet rich plasma and platelet rich fibrin can be added for faster healing and a better scar.
Hematoma
Haematoma is another common cause of flap necrosis. Control of hypertensive status, achieving good haemostasis during surgery and compression dressing, restriction of mobility post surgery alleviate the risk of haematoma. All flap cases should be examined within 24 to 48 hours to look for any haematoma which can be identified by bluish or dusky erythematous disclouration of flap. In such cases, haematoma should be drained by removing two or three sutures. If active bleeding is there, bleeder should be ligated followed by compression dressing. If neglected at this stage, it can result in full thickness skin necrosis. We encountered a case of flap necrosis due to haematoma as the patient was not followed up in immediate post operative period to identify the haematoma which lead to flap necrosis.
Hypertrophic scar
Scarring is an inevitable risk with flap surgeries. However, it can be made minimal and aesthetical acceptable with proper designing so that final suture lines fall along RSTL. Surgical areas over jaw line, chest back carry risk of hypertrophic scar. Patients with keloidal tendency should be taken care during surgery with minimal traumatising techniques followed by intralesional corticosteroids. In our study we had two patients with hypertrophic scar, one resolved with intralesional steroid [Figure 5A and B] and other case was lost to follow up.
- (A and B) Hypertrophic scar managed with three sittings of intralesional steroid
Pincushion deformity
Pincushioning also called as trapdoor deformity or biscuiting, is a complication seen in facial reconstruction. Its etiology is varied. According to some authors this deformity is more common in Melolabial, U, V, and C shaped flaps[10] and also more frequently if their apex is in dependent as in our case. Contraction of the scar underlying the flap bed, excess subcutaneous fat on the undersurface of the flap, persistent edema, lymphedema of the wound edge, hypertrophy of the underlying scar bed, and beveled wound edges are some of the causes that have been proposed for the development of pincushioning.[11] Ensuring a tension-free closure with appropriate eversion of the wound edges will help reduce pincushioning.[12] However pincushion deformity is dissapointing to both the surgeons and patients. In our study we had one patient with pincushion deformity which was managed with intralesional steroid [Figure 6A and B].
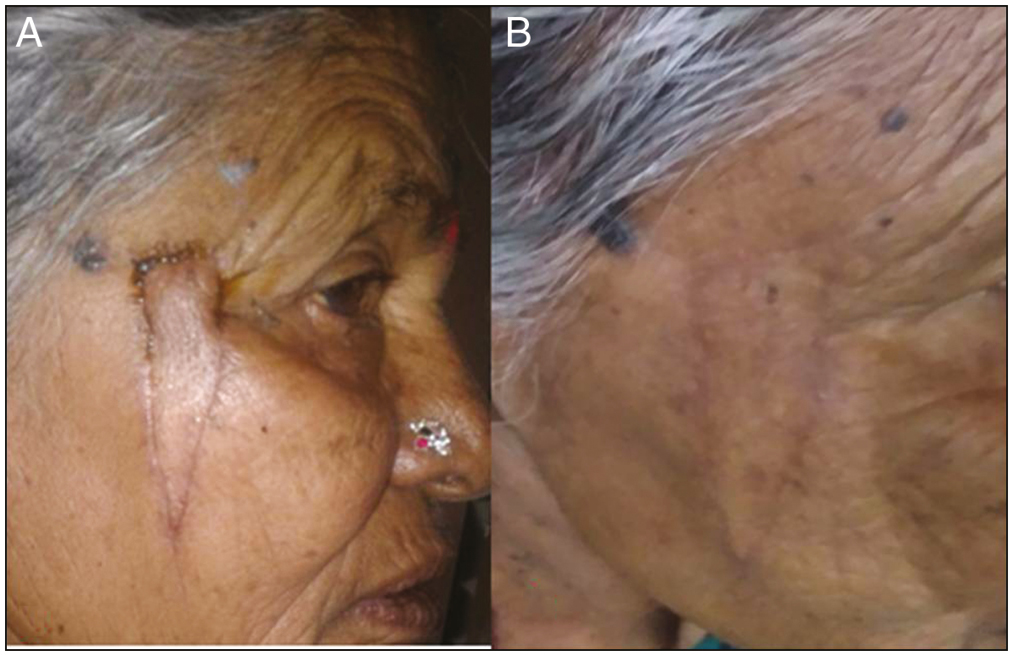
- (A and B) Pin cushion deformity managed wih intralesional steroid
Anatomical distortion
Flaps for facial reconstruction around orifices have to be meticulously planned. Defect closure around nose, eyelids, and lips are particularly susceptible to this distortion. Achieving a tension-free closure is fundamental to avoid this complication. As the wound heals flap contracts thus exerting pulling effect on adjacent structures. In our study, flap for large lesion near to lower eyelid excision resulted in ectropion [Figure 7] which was referred to a oculoplasty surgeon. Any lesion within one cm of the orifices flap should be planned in such way that vectors of tension will not distort these orifices or free grafts can be considered as an alternative.

- Ectropion following a flap surgery near the eye
We also encountered case of temporary facial nerve paresis which recovered within 48 hours.[Figure 8A and B] This is common in flap surgeries done in the area of facial nerve course. In our patient the lesion was in reauricular area. This is a temporary complication as result of local anaethesia impairing sensory and motor nerve function. However permanent nerve injuries is a possibility, if deeper dissection done or nerve runs a superficial course. One should be aware of the normal course of neurovacular bandle in operative area to avoid permanent injury.

- (A and B) Temporary facial nerve palsy with spontaneous recovery
Recurrence
Recurrence of primary lesion is a late complication of flap surgery. We had one case of BCC reccurrence [Figure 9] after an year following surgery though histopathological examination had confirmed tumor free margins. Hence such cases with high grade malignant tumours should be followed up regularly for early detection of recurrence or adjutants like radiotherapy can be considered.

- Recurrence following BCC excision
CONCLUSION
Avoidance of complications are a essential integral part of surgical management which should begin in the preoperative period itself with a comprehensive history, medical co-morbidities, risk assessment and physical examination. Successful outcome can be achieved with systematic, comprehensive analysis of the tumor defect, appropriate technique, judicious wound management and follow up care.
Cutaneous malignancies are which are localised and surgically treatable, should be evaluated, confirmed diagnostically and removed at the earliest. Local fascio-cutaneous flaps give cosmetically best results. However, though at an outlook appear simple, can also manifold into long term complications like keloid and hypertrophic scars. Hence, we need to be vigilant while surgically treating these cases and follow them up periodically.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
References
- Annual report to the nation on the status of cancer (1973 through 1998), featuring cancers with recent increasing trends. J Natl Cancer Inst. 2001;93:824-42.
- [Google Scholar]
- Pattern of skin malignancies in Manipur, India: A 5-year histopathological review. Journal of Pakistan Association of Dermatologists. 2010;20:128-132.
- [Google Scholar]
- Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis. Wien Klin Wochenschr. 2017;129:303-16.
- [Google Scholar]
- Perioperative management of patients who are receiving warfarin therapy: An evidence-based and practical approach. Blood. 2011;117:5044-9.
- [Google Scholar]
- Flap necrosis and pincushioning. Operative Techniques In Otolaryngology-Head And Neck Surgery. 1993;4:82-5.
- [Google Scholar]
- Local Flaps in Head and Neck Reconstruction. St. Louis, MO: CV Mosby; 1985.
- The use of keystone flaps in periarticular wound closure: A case series. Front Surg. 2017;4:68.
- [Google Scholar]
- The pinprick test: Key considerations in execution of skin flap perfusion testing. Plast Reconstr Surg Glob Open. 2019;7:e2370.
- [Google Scholar]
- The nasolabial flap: A problem and its correction. Plast Reconstr Surg. 1982;69:30-4.
- [Google Scholar]
- Trapdoor effect in nasolabial flaps. Arch CUPP AND MURAKAMI Otolaryngol Head Neck Surg. 1985;111:421-4.
- [Google Scholar]
- Complications in facial flap surgery. Facial Plast Surg Clin N Am. 2013;21:599-604.
- [Google Scholar]






