Translate this page into:
Pseudoepitheliomatous Hyperplasia: A Clinical Entity Mistaken for Squamous Cell Carcinoma
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Pseudoepitheliomatous hyperplasia (PEH) is a benign condition characterised by hyperplasia of the epidermis and adnexal epithelium closely simulating squamous cell carcinoma (SCC).[1] PEH is commonly mistaken for SCC.[2] We present a case which was initially reported as SCC but on clinical suspicion a repeat deeper biopsy was performed which confirmed the diagnosis of PEH and was managed accordingly.
An 80-year-old male patient was referred to surgical oncology department with a rapidly progressing lesion over the right preauricular region since 3 months and with a previous biopsy report of SCC [Figure 1]. The patient had no history of similar complaints in the past or in the family. The patient gives negative history of diabetes mellitus and tuberculosis. On examination the lesion measured 8 × 6 cm with everted edges with floor of the ulcer showing intervening normal skin tissue with irregular margin. Regional lymph nodes were normal on palpation and the underlying bone was normal. On clinical suspicion a repeat biopsy with wider and deeper area was performed which was reported as PEH. In order to rule out malignancy as reported in the intial biopsy report the entire specimen of the deeper biopsy and the final excised specimen were subjected to multiple surgical pathology sections before confirming the diagnosis of PEH. The patient was worked up for surgery and wide excision of the skin mass with adequate margin with posterior auricular artery-based pedicle flap reconstruction was performed with split skin graft over the flap donor area [Figure 2].

- Skin lesion 8 × 6 × 2 cm over the right preauricular region with everted margins with central area showing normal skin tissue

- Post surgery photograph showing left-sided posterior auricular artery pedicle flap reconstruction with split skin surgery cover of donor area
SCC is a common primary cutaneous malignancy, though less common than basal cell carcinoma.[3] It is locally invasive and has capacity to metastasize. On skin biopsy SCC is characterised by significant squamous cell atypia, abnormal keratinisation and invasive features. Benign mimics of SCC include PEH, eccrine squamous syringometaplasia, inverted follicular keratosis, keratoacanthoma while malignant mimics of SCC include basal cell carcinoma, melanoma and metastatic carcinoma.[4] PEH is not fundamentally a hyperplasia of epidermal epithelium, but rather a hyperplasia of adnexal epithelia, namely of follicular infundibula[5] and eccrine ducts[6] closely simulating SCC. PEH may be present in a number of conditions characterised by chronic inflammation or exist in association with many cutaneous neoplasms.[1] PEH shows irregular invasion of the dermis by uneven, jagged, often pointed epidermal cell masses and strands with horn-pearl formation. Irregular proliferation of epidermis may extend below the level of sweat gland, where they appear as isolated island of epidermal tissue. Furthermore, one often sees invasion of epithelial proliferation by leucocytes and disintegration of some of the epidermal cells in PEH, a finding that is absent in SCC. Verrucous carcinoma shows a verrucous upward and downward proliferation with more pronounced keartinisation in downward extension, which appears bulbous rather than sharply pointed as in PEH.[7] Keratoacanthoma centrifugum marginatum is a rare variant of keratoacanthoma, where the lesions typically appear on the dorsum of hand and leg. A fully developed lesion shows a large irregularly shaped crater filled with keratin. At the base of crater, irregular epidermal proliferation extends both upward into the crater and downward from base of crater. These proliferations may appear somewhat atypical. In the present case, even after extensive sampling these findings were not found.
PEH may be primary (e.g., primal gingival PEH) or secondary as in granular cell tumour or chronic irritation.[8] PEH has been reported following tattooing in a three case series,[9] and following Mohs micrographic surgery.[10] In the present case, there was no obvious similar history of trauma. However, the patient was diagnosed with chronic suppurative otitis media for which patient was on antibiotic ear drops but the skin over external auditory canal was grossly normal. A skin biopsy itself poses a difficulty in diagnosis for the pathologists as the biopsy specimen sent may not be adequate to represent the lesion as it was in the present case.[10] We would like to emphasise on understanding of this limitation and call for a strong clinico-pathological correlation and a selective need for a deeper and wider biopsy to be sent for a proper pathological evaluation.[4]
Repeat biopsy reported florid hyperplasia of squamous epithelium with invagination in the dermis forming nodular masses made of sheets, cell nest with large keratin pearls and keratin cyst and moderate inflammatory cell infiltrate in dermis and interstitial tissue with giant cell reaction with no evidence of dysplasia, thereby confirming the diagnosis of PEH.[1] This finding was further validated in the final histopatholgical report of the excised skin lesion [Figures 3 and 4]. The limitation in the case was that we could not elucidate the etiology.
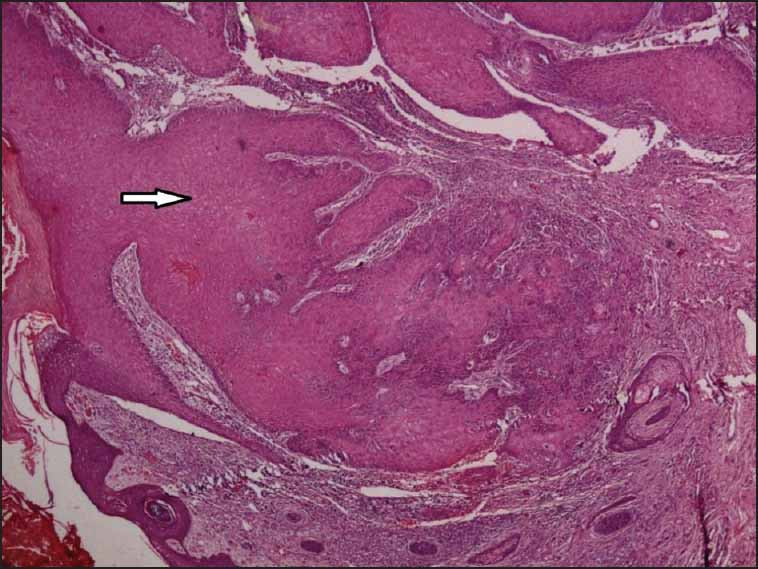
- Scanner view (40×) showing marked hyperplasia of stratified squamous epithelium with epidermal invagination in dermis (white arrow), forming nodular masses made of sheets with marked inflammatory cell infiltrate in the interstitium
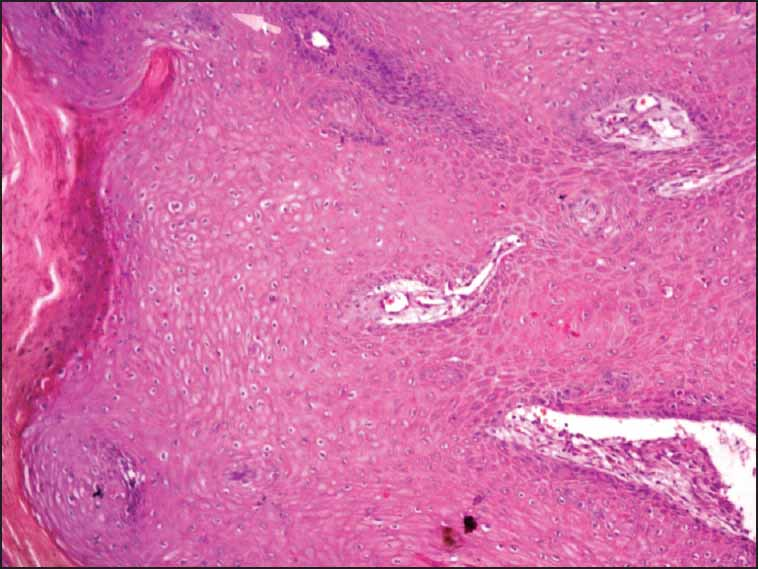
- Epidermal downgrowth from the epidermis (H and E 100×)
PEH is a benign condition and can be managed with surgical excision with adequate margin and antibiotics, hence it has to be differentiated from other mimickers of SCC both benign and malignant.[11]
PEH is a benign condition which has to be differentiated from SCC, as the treatment and prognosis for the patient changes. Erroneous diagnosis of malignancy will lead to radical surgery and surgery-related morbidity. Limitations of biopsy should be kept in mind and a strong clinico-pathological correlation is required with selective need for deeper biopsy to arrive at a final diagnosis before planning on surgical management.
REFERENCES
- Pseudoepitheliomatous hyperplasia mistaken for cancer after delayed reconstruction. South Med J. 1995;88:454-7.
- [Google Scholar]
- Simulators of squamous cell carcinoma of the skin: Diagnostic challenges on small biopsies and clianicopathological correlation. J Skin Cancer. 2013;2013:752-864.
- [Google Scholar]
- Cutaneous malignant melanoma associated with extensive pseudoepitheliomatous hyperplasia. Report of a case and discussion of the origin of pseudoepitheliomatous hyperplasia. J Cutan Pathol. 2000;27:153-6.
- [Google Scholar]
- Lever's Histopathology of the Skin (10th ed). Philadelphia: Lippincott Williams & Wilkins; 2008. p. :822-3.
- Lesions of oral cavity. In: Gnepp DR, ed. Diagnostic Surgical Pathology of the Head and Neck. Philadelphia, PA: WB Saunders; 2001. p. :205-7.
- [Google Scholar]
- Pseudoepitheliomatous epidermal hyperplasia in tattoos: Report of three cases. Am J Clin Dermatol. 2008;9:337-40.
- [Google Scholar]
- Pseudoepitheliomatous hyperplasia following Mohs micrographic surgery. J Dermatol Surg Oncol. 1989;15:557-60.
- [Google Scholar]
- Pseudoepitheliomatous hyperplasia formation after skin injury. Wound Repair Regen. 2007;15:39-46.
- [Google Scholar]





