Translate this page into:
Real-time Intraoperative Dermoscopic Monitoring of Common Acquired Melanocytic Nevi Following Shave Excision
Address for correspondence: Dr. Ishika Muradia, Department of Dermatology and Sexually Transmitted Diseases, Vardhman Mahavir Medical College and Safdarjung Hospital, Delhi, India. E-mail: dr.ishika.138@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
The treatment of common acquired melanocytic nevus (CAMN) is mostly desired for cosmetic purposes due to which a number of “faster and less traumatizing” techniques have been developed. The major cause of recurrence is incomplete removal; there is a need for early detection of any residual pigment.
Aims and Objectives:
This study aimed to assess the recurrence of common acquired melanocytic nevi and whether dermoscopy can be used as a noninvasive tool for the assessment of residual pigment following shave excision.
Materials and Methods:
A total of 100 patients of age more than 18 years with clinical features suggestive of common acquired melanocytic nevi were enrolled in the study. The nevi were assessed clinically and dermoscopically and, if found benign, were excised using shave excision. The specimen obtained was sent for histopathological examination. Dermoscopy was used immediately after shave excision for observing any residual pigment and, if present, was removed using radiofrequency current. The patients were followed up at 6 and 12 weeks for recurrence.
Results:
On histopathology, 87% nevi were intradermal, 8% were compound, and 5% had insufficient tissue for diagnosis, which were clinically diagnosed as junctional nevi. Dermoscopy immediately after shave excision helped in detecting residual pigment in 91% nevi, which was immediately ablated with radiofrequency, thus decreasing the risk of recurrences. Recurrences were seen in 33% nevi and all were intradermal with the presence of hair in the majority (66.67%) of them.
Conclusion:
Shave excision is a minimally invasive and easily performed procedure. Dermsocopy can be used for assessing residual pigment after shave excision and thus reducing the risk of recurrences. On combining shave excision with radiofrequency ablation and assessing by dermoscopy, majority of patients were satisfied with the cosmetic results. Using dermoscope for follow-up helps in early recognition of recurrence and thus appropriate treatment can be provided at the earliest.
Keywords
Common acquired melanocytic nevi
radiofrequency current
real-time intraoperative dermoscopic monitoring
shave excision
INTRODUCTION
Common acquired melanocytic nevus (CAMN) is a benign proliferative lesion of melanocytes that occurs after birth.[1] It can be broadly divided into intradermal, junctional, and compound nevi according to the site of the nevus cell nests. People seek removal of melanocytic nevi mainly for cosmetic purposes. Surgical treatment of benign melanocytic lesions demands the application of simple and effective surgical techniques with low morbidity, a low rate of recurrences, acceptable cosmetic results, and the possibility to provide adequate specimens for histopathologic examination.[2] An acceptable cosmetic result is a major consideration for these procedures to be accomplished because most of such lesions are removed for cosmetic reasons. Different methods have been used like radiofrequency ablation, carbon dioxide (CO2) or erbium-doped yttrium aluminum garnet laser (Er:YAG) lasers, shave excision, punch excision and simple elliptical sutured excision. Before using any of these techniques the possibility of melanoma and dysplasia should be ruled out.[3] All of these determining factors have turned shave excision into a widely used surgical technique for excision of benign pigmented lesions with the best cosmetic results.[2]
A dermoscope (dermatoscope) is a noninvasive, diagnostic tool that visualizes the subtle clinical patterns of skin lesions and subsurface skin structures that are normally not visible to the unaided eye. The basic principle of dermoscopy is transillumination of a lesion and studying it with a high magnification.[4] It is seen that the melanocytic nevi usually recur due to its incomplete removal. Two types of the clinical appearance of these recurrences are observed. The lesion may reappear as an area of pigmentation or an elevation at the site of previous removal.[5]
Recurrences following shave excision can be minimized if all the melanocytic tissue is adequately removed. This study aimed to use dermoscopy as a noninvasive assessment tool to detect and remove residual pigment immediately following surgery and hence minimize the incidence of recurrence.
MATERIALS AND METHODS
After taking proper approval from the ethical committee, a prospective interventional cohort study was carried out in a tertiary care center for a duration of 18 months. The sample size of 100 nevi was taken. Adult males and females of more than 18 years of age with clinical features suggestive of common acquired melanocytic nevi and who have not undergone any prior procedure for its removal were included in the study after obtaining proper informed consent.
Patients with nevi showing dermoscopic findings suggestive of atypical nevi or suspicious changes or with histopathological findings of atypical nevi or malignant changes, nevi over nail bed, genitals and mucosa, and patients with a history of keloid formation were excluded from the study.
Dermoscopic assessment was performed using Dermlite DL4 dermoscope (3 Gen, California) using both polarized and nonpolarized mode. The images of all the relevant findings were taken under both 10× and 20× optical zoom and recorded in the proforma as well. Dermoscopic assessment was done at the initial visit according to ABCD rule to confirm that the nevi are benign[67] [Tables 1,2–3].
| Dermoscopic features | Definition |
|---|---|
| A = asymmetry | The lesion is bisected by two lines that are placed 90degree to each other. The first line attempts to bisect the lesion at the division of “most symmetry” and the other line is then placed at 90 degrees to it. Symmetry takes into account the contour, colors and structures within a lesion. Lesions that are symmetric in both axes are given zero points, one axial asymmetry one point and biaxial asymmetry 2 points. Thus, the points range from 0 to 2. |
| B = border sharpness | First the lesion is divided into eight pie-shaped pieces. Next, the number of segments that have an abrupt perimeter cut off are counted. Thus, the points range from 0-8. |
| C = colors | Number of following colors present: light brown, dark brown, black, red, white, blue-grey. Thus, the points range from 1 to 6. |
| D = dermoscopic structures | Number of following 5 structures: dots, globules, structureless (homogenous) areas. Network and branched streaks. |
| Features | Points | Weight factor | TDS score |
|---|---|---|---|
| Asymmetry | 0–2 | *1.3 | 0–2.6 |
| Border sharpness | 0–8 | *0.1 | 0–0.8 |
| Colors | 1–6 | *0.5 | 0.5–3.0 |
| Dermoscopic structures | 1–5 | *0.5 | 0.5–2.5 |
| Total dermoscopic score (TDS range) | 1.0–8.9 |
*Stands for “multiplied by”
| Category | Score range |
|---|---|
| Benign | <4.75 |
| Suspicious | 4.75-5.45 |
| Malignant | >5.45 |
Shave excision of the nevus was performed using a 15 number surgical blade and biopsy specimen was collected in a glass vial containing 10% formalin. Dermoscopy was repeated immediately after shave excision. If pigment was detected it was removed with radiofrequency ablation and repeated again, till pigment was no longer detected. Radiofrequency was performed using Ellman Surgitron Dual RFTM 120 (New York) machine with a solid 2 mm ball probe. Combined electrodessication and electrocoagulation mode at power 2–8 W was used for removing the residual pigment if present and simultaneously obtaining hemostasis. Visual analog scale was used for pain assessment immediately after the procedure[8] [Figure 1]. All patients were reviewed after 6 and 12 weeks for assessing patient’s satisfaction and dermoscopy for assessing recurrences.
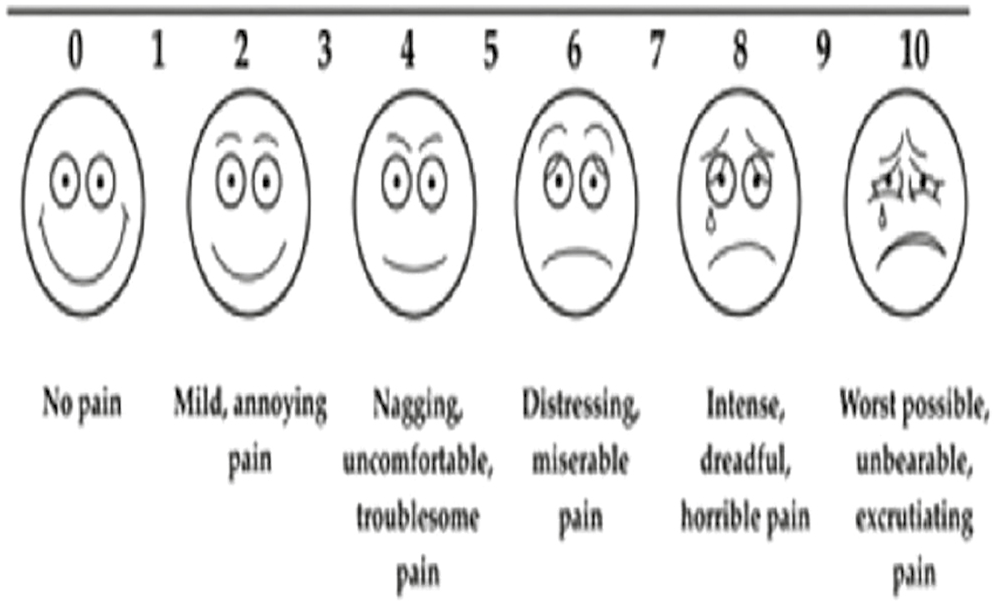
- Visual analog scale
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± standard deviation (SD) and median. Normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected then nonparametric test was used. Quantitative variables were compared using Mann–Whitney test (as the data sets were not normally distributed) between the two groups.
Qualitative variables were associated using chi-square test/Fisher’s exact test.
Data were analyzed using Statistical Package for Social Sciences (SPSS) version 21.0.
RESULTS
The age of the patients varied from 18 years to 50 years, with mean age (years) of patients 23.59 ± 8.1. Out of 100, 83 patients were females and only 17 were males. On dermoscopy, different structures were observed in nevi. Pigmented dots were seen in 89% nevi, globules in 61% nevi, structureless areas in 59% nevi, pigment network in 37% nevi and branched streaks in 6% nevi. Three different dermoscopic structures were seen in 53% nevi, 2 in 40% nevi, 1 in 5% nevi and 4 in 2% nevi [Figure 2A-D]. On histopathological examination, 87% of the nevi were found to be intradermal [Figure 3A], 8% were compound [Figure 3B]. In 5% nevi the tissue was insufficient for diagnosis that were clinically diagnosed as junctional nevi [Figure 3C]. On performing dermoscopy after shave excision, residual pigment was observed in 91% nevi and rest 9% were completely clear of any residual pigment. To remove this residual pigment, radiofrequency current was used and the removal was confirmed using dermoscopy. On follow-up after 6 and 12 weeks, 67% nevi did not recur [Figure 4A-D] and recurrence was seen in rest 33% nevi [Figure 5A and B]. Hair was present in total 25 nevi out of which 22 recurred. Recurrence was present in 33% nevi with significantly higher recurrence rate of 88% in hairy nevi [Table 4]. Recurrence was seen in none of the macular nevi, 34.29% of papular nevi, 33.33% of dome shaped papules, 50% of papillomatous papules [Figure 6]. On performing real-time dermoscopy immediately after shave excision, residual pigment was present in 98.85% of intradermal nevi which was significantly higher as compared to 62.50% of compound nevi [Figure 7]. Significant association was seen between residual pigment on dermoscopy immediately after shave excision tissue with type of nevi (P < .05) On performing dermoscopy after 6 weeks and 12 weeks, recurrence was seen in 37.93% of intradermal nevi which was significantly higher as compared to none of the compound nevi [Figure 8]. A significant association was observed between recurrence on dermoscopy after 6 and 12 weeks with type of nevi (P < .05) [Table 5].
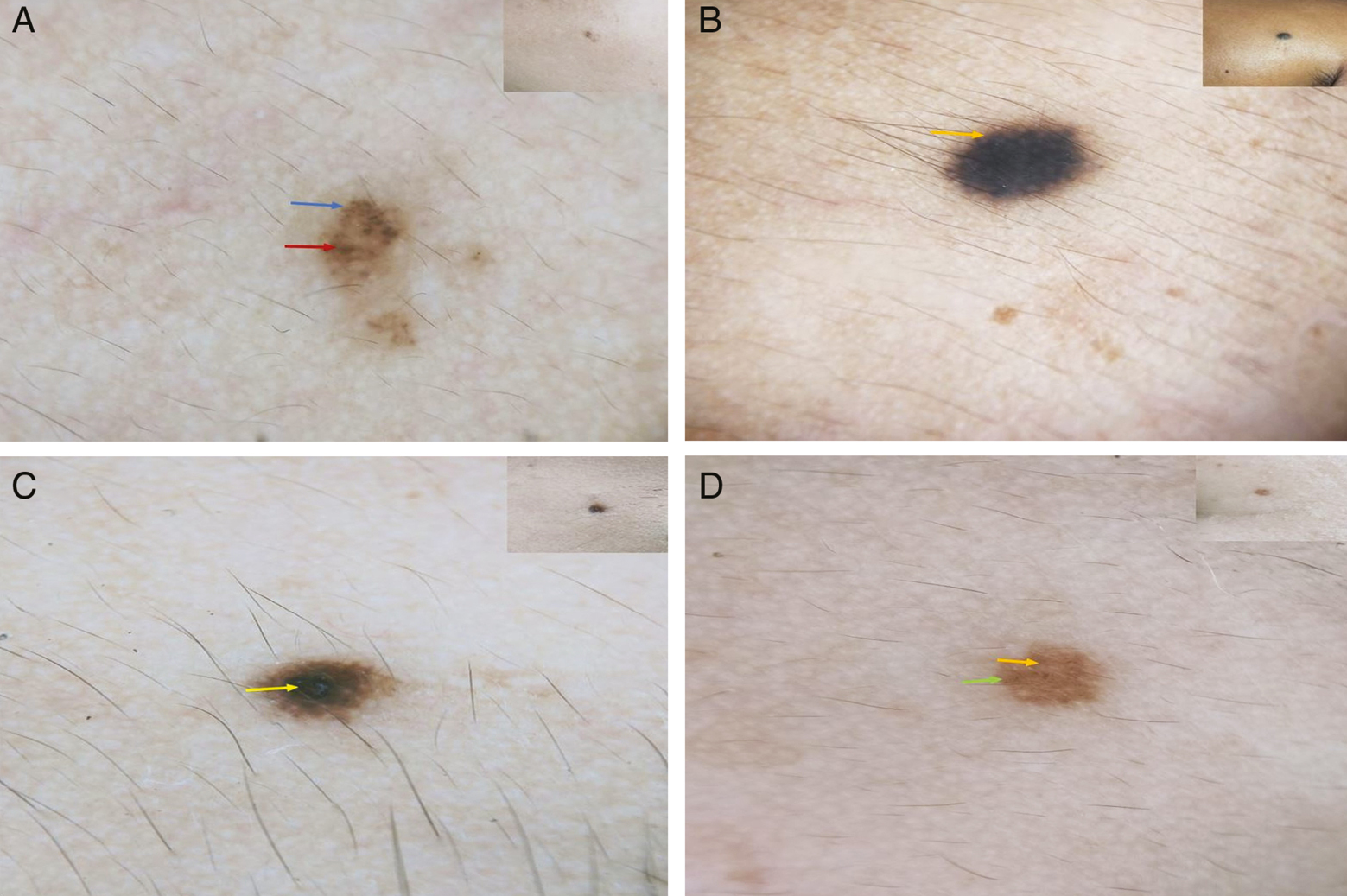
- Dermoscopic polarized view images with corresponding clinical images in inset. (A) Dots (blue arrow) and globules (red arrow). (B) Pigment network (orange arrow). (C) Structureless areas (yellow arrow). (D) Dots (yellow arrow) and structureless areas (green arrows)
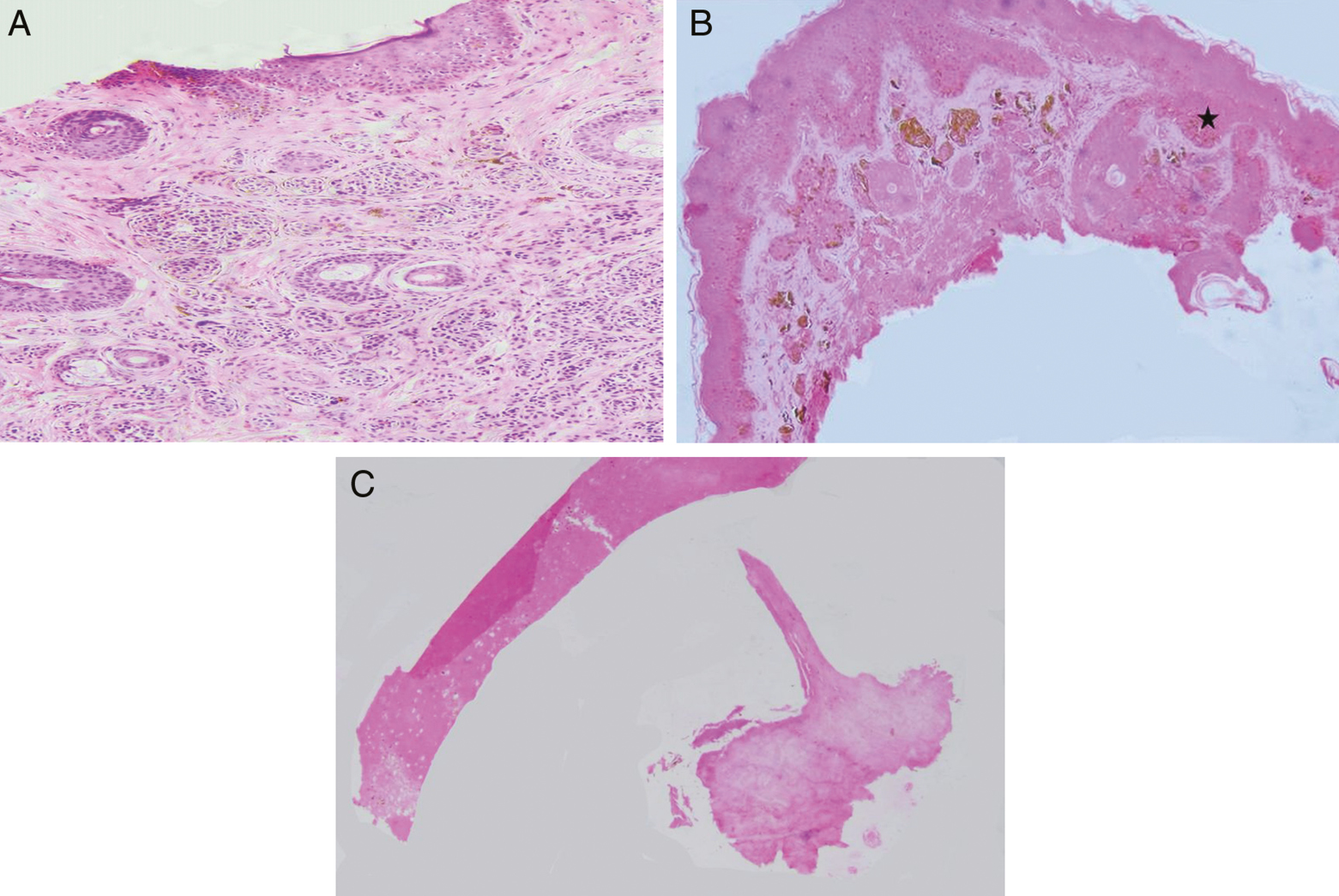
- (A) Intradermal nevus showing nevus cell nest in the dermis with type A, B and C nevus cells with no junctional activity (100×, H&E). (B) Compound nevus showing nevus cell nest both in epidermis as well as in dermis with junctional activity (star) (100×, H&E). (C) Section shows unremarkable epidermis and dermis (100×, H&E)
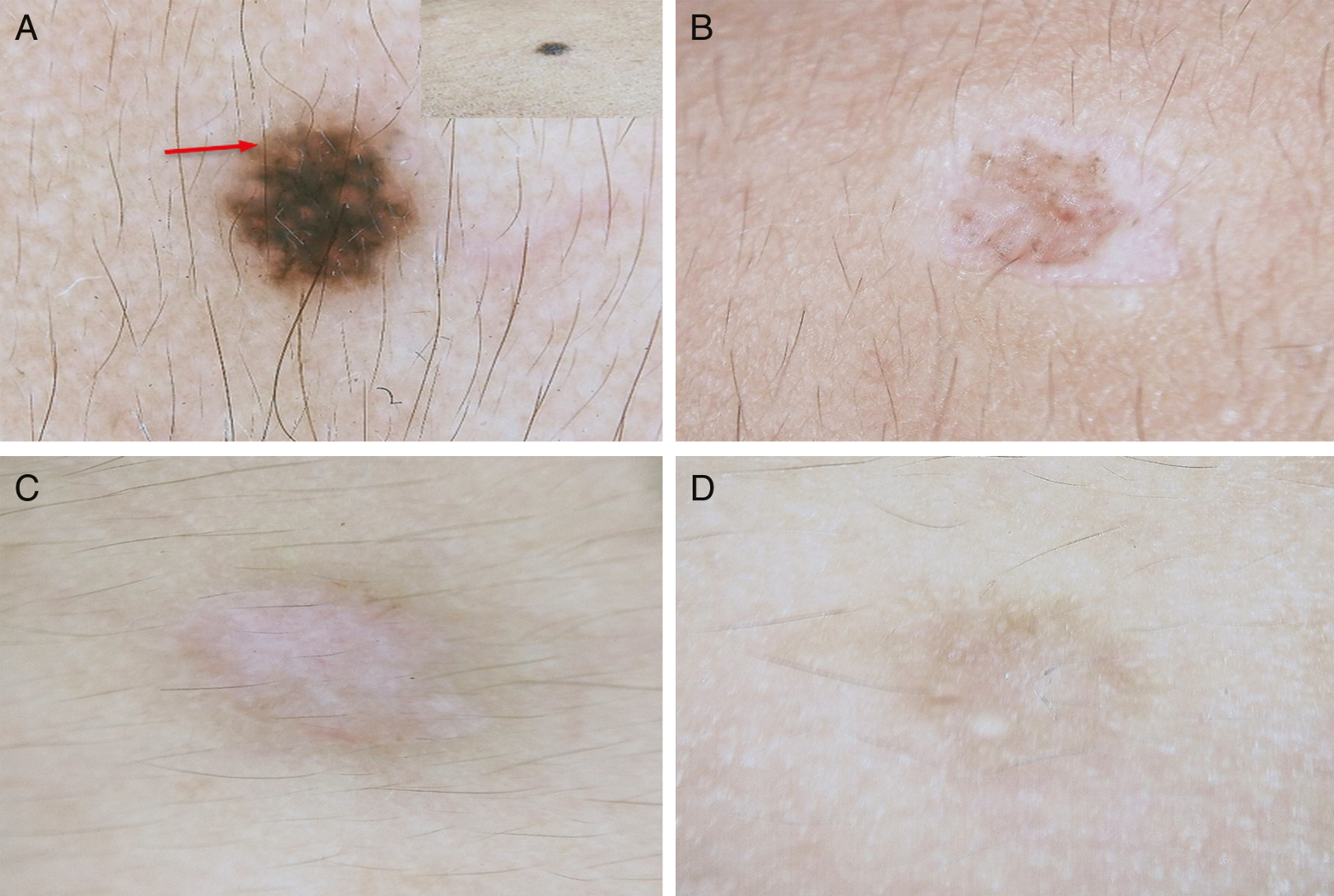
- Dermoscopic polarized view images of a nonrecurrent nevi. (A) Dermoscopic image showing pigment network with clinical image of the nevus in inset. (B) Dermoscopic image following shave excision and radiofrequency. (C) Dermoscopic image after 6 weeks, no recurrence. (D) Dermoscopic image after 12 weeks, no recurrence
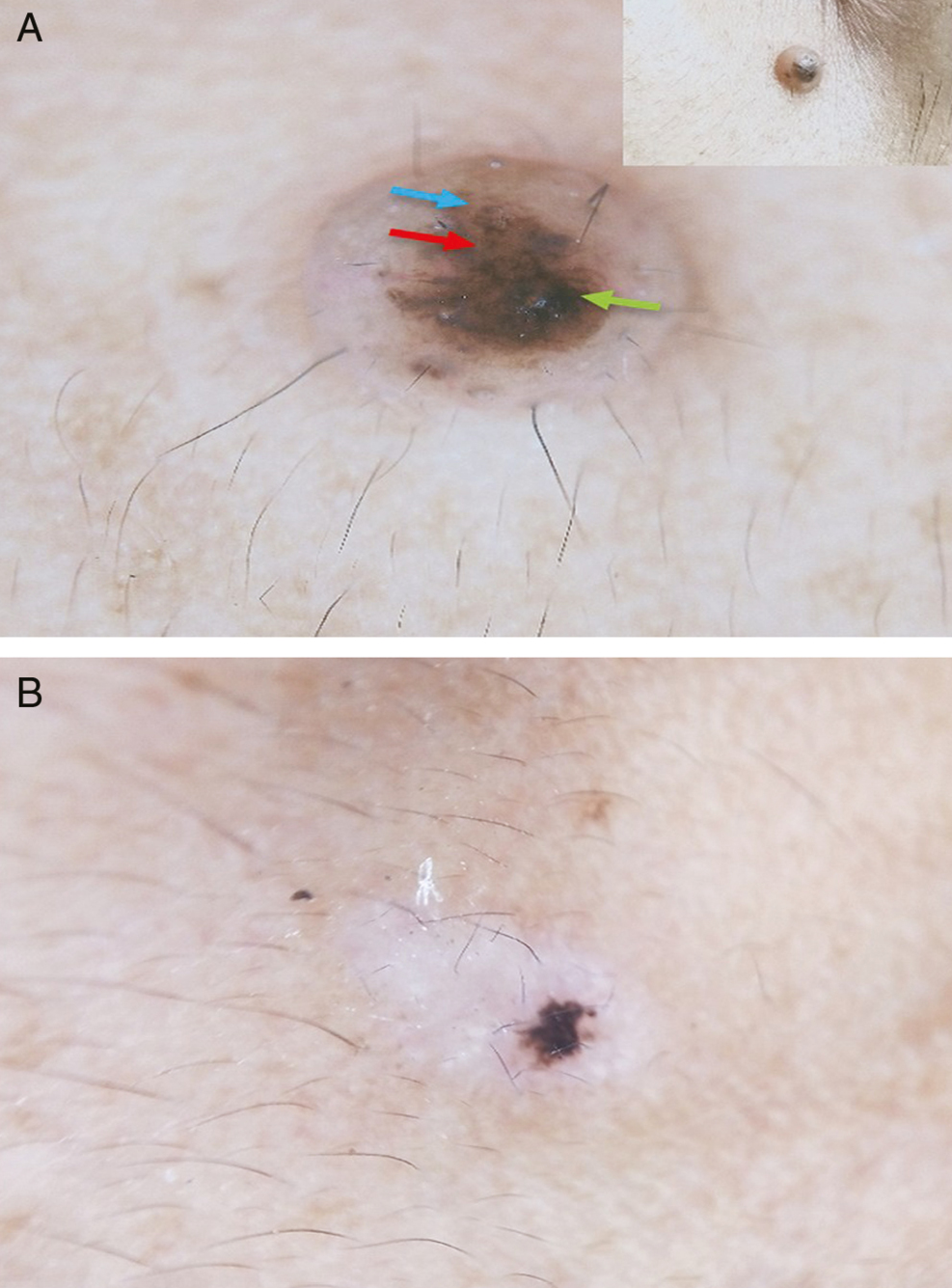
- Dermoscopic polarized view images of a recurrent nevus. (A) Dermoscopic image showing dots (red arrow), globules (blue arrow), and structureless areas (green arrow) of an intradermal nevus with clinical image in inset. (B) Dermoscopic image of a recurrent nevus after 12 weeks.
| Recurrence | Hair present | Hair absent | P Value | Test performed |
|---|---|---|---|---|
| Present (n = 33) | 22 | 11 | 0.0001 | Fisher exact test |
| Absent (n = 67) | 3 | 64 | ||
| Total (n = 100) | 25 | 75 |
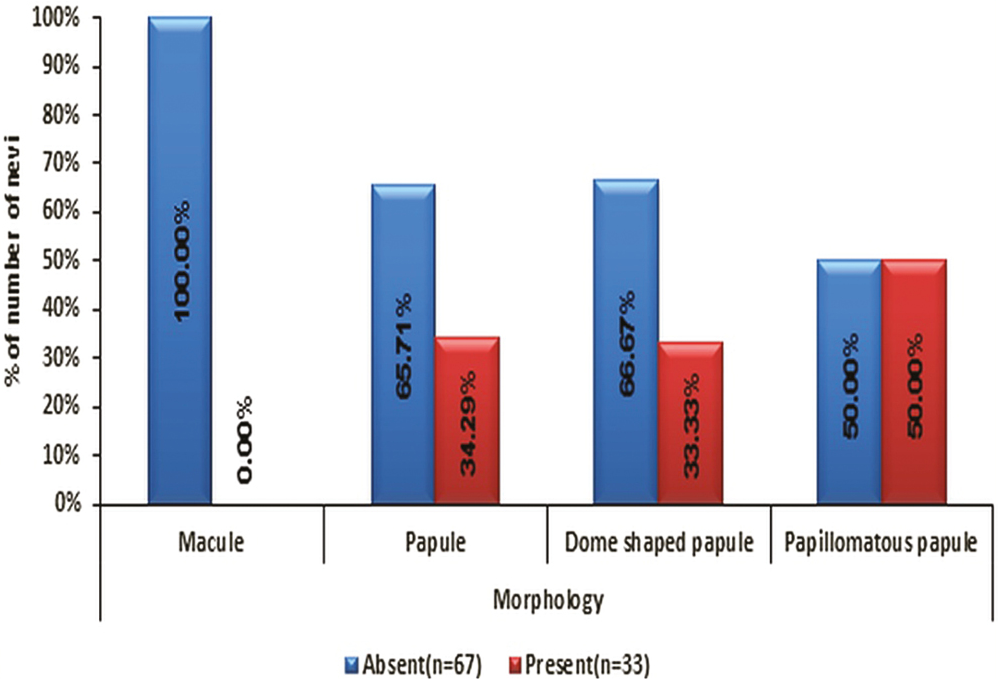
- Distribution of morphology of nevi with recurrence
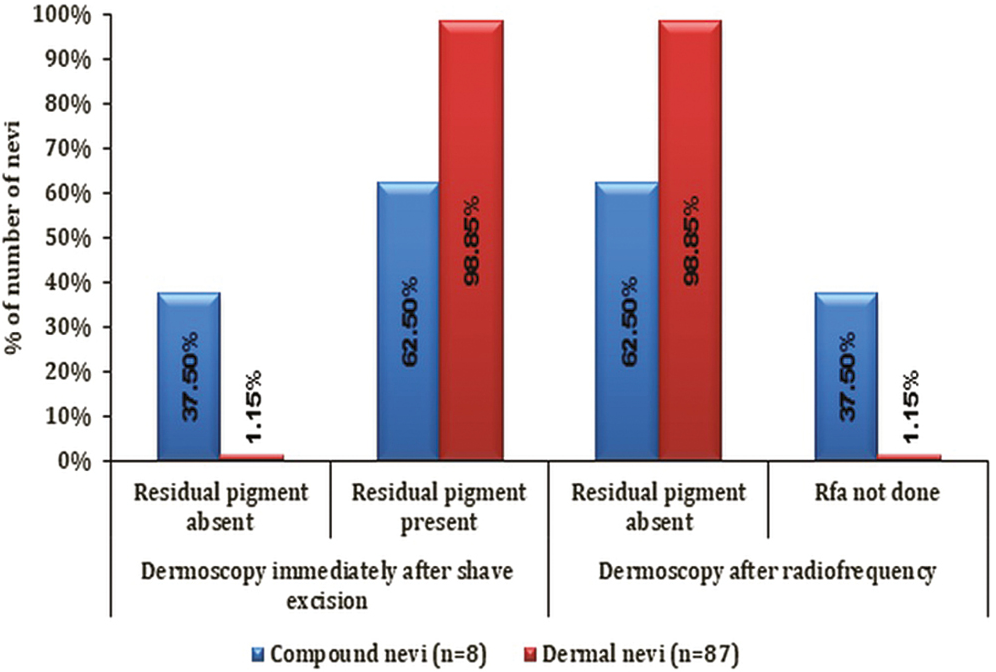
- Distribution of dermoscopy assessment after shave excision and radiofrequency with type of nevi
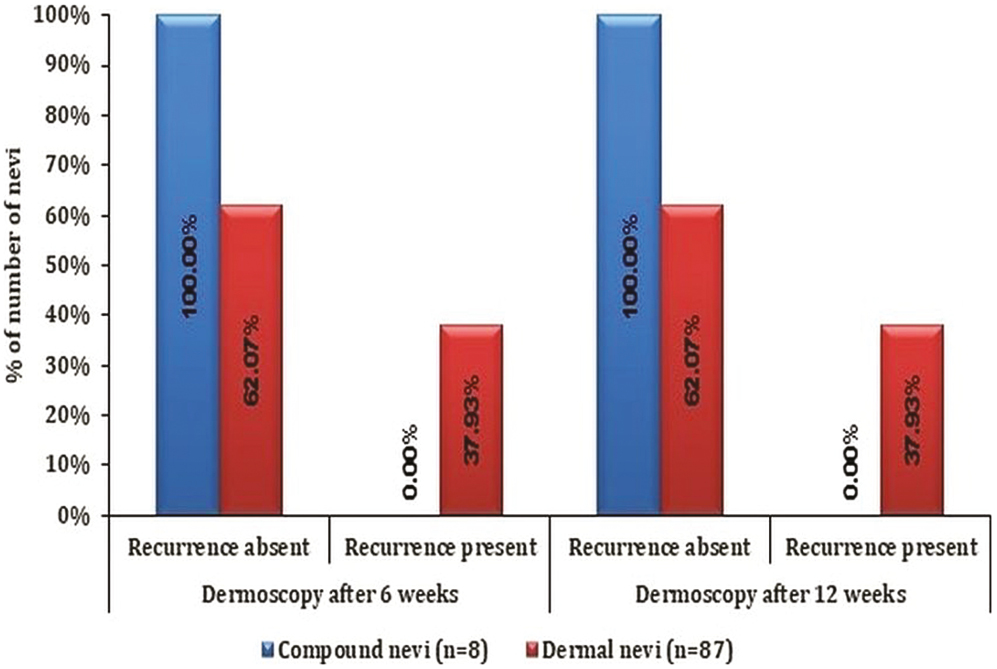
- Distribution of dermoscopy assessment for recurrence with type of nevi
| Dermoscopy assessment | Compound nevi (n = 8) | Intradermal nevi (n = 87) | Total | P Value | Testperformed |
|---|---|---|---|---|---|
| Dermoscopy immediately after shave excision | |||||
| Residual pigment absent | 3 (37.50%) | 1 (1.15%) | 4 (4.21%) | 0.002 | Fisher exact test |
| Residual Pigment present |
5 (62.50%) | 86 (98.85%) | 91 (95.79%) | ||
| Dermoscopy after radiofrequency | |||||
| Residual pigment absent | 5 (62.50%) | 86 (98.85%) | 91 (95.79%) | 0.002 | Fisher exact test |
| Radiofrequency not done | 3 (37.50%) | 1 (1.15%) | 4 (4.21%) | ||
| Dermoscopy after 6 weeks | |||||
| Recurrence absent | 8 (100%) | 54 (62.07%) | 62 (65.26%) | 0.047 | Fisher exact test |
| Recurrence present | 0 (0%) | 33 (37.93%) | 33 (34.74%) | ||
| Dermoscopy after 12 weeks | |||||
| Recurrence absent | 8 (100%) | 54 (62.07%) | 62 (65.26%) | 0.047 | Fisher exact test |
| Recurrence present | 0 (0%) | 33 (37.93%) | 33 (34.74%) | ||
On pain assessment immediately after procedure, using visual analog scale, 67% of patients had no pain with a VAS score of 0, 23% patients had mild annoying pain with a score of 2 and 10% patients had pain in between in the two with a score of 1 [Figure 9]. On assessing patient satisfaction after 12 weeks, 31% of patients were very satisfied, 37% were satisfied and 32% were slightly satisfied. Amongst all the patients with compound nevi, 87.50% were very satisfied which was significantly higher as compared to 21.84% of patients with intradermal nevi patients. A significant association was observed between the patient satisfaction with type of nevi (P < .05) [Table 6].
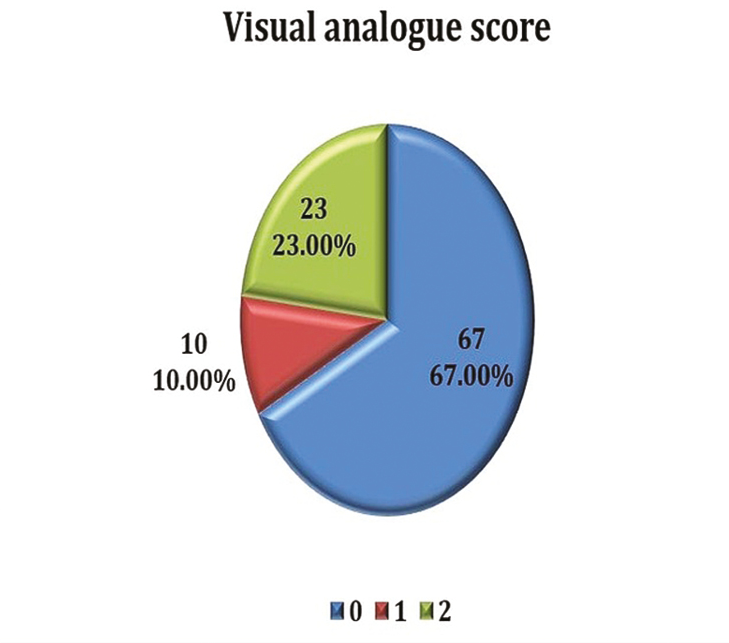
- Distribution of visual analogue score
| Patient satisfaction | Compound nevi (n = 8) | Intradermal nevi (n = 87) | Total | P Value | Test performed |
|---|---|---|---|---|---|
| Very satisfied | 7 (87.50%) | 19 (21.84%) | 26 (27.37%) | 0.0005 | Fisher exact test |
| Satisfied | 1 (12.50%) | 36 (41.38%) | 37 (38.95%) | ||
| Slightly satisfied | 0 (0%) | 32 (36.78%) | 32 (33.68%) | ||
| Total | 8 (100%) | 87 (100%) | 95 (100%) |
DISCUSSION
We did a detailed study of 100 common acquired melanocytic nevi and studied its clinical and dermoscopic features and confirmed the diagnosis on histopathology. We used shaved excision for removal of the nevi and if on dermoscopy any residual pigment was observed, it was removed using radiofrequency current. Patients were followed up after 6 and 12 weeks for recurrence.
The mean age of patients in our study was 23.59 ± 8.1 years with majority of cases seen in second and third decade with 48% and 36% patients respectively. A study by Ghosh et al.[9] showed similar results, with a mean age of 28 years, and maximum no. of patients in third decade followed by second decade with 32.4% and 25.6% patients respectively. Most of other studies had a mean age of 32 years.[101112]
In our study, 83 were females and 17 were males which was very similar to a study by Bong and Perkins[13] with 82% females and 18% males. Since there is no sex predilection, this difference might be due to greater cosmetic concerns in females.
Different dermoscopic algorithms can be used for differentiating benign melanocytic nevi from melanoma. ABCD algorithms were used in our study for assessing all the common acquired melanocytic nevi. Only those who were benign on dermoscopic assessment were included in our study for further intervention.
Histopathology is the gold standard for making the diagnosis. On histopathology, 87% of the nevi were intradermal, 8% were compound nevi and for 5% nevi the tissue was insufficient for diagnosis. Heck et al.[14] in their study performed shave excision of 224 acquired melanocytic nevi and found that on histopathology 92% nevi were intradermal, 8% were compound nevi. In a study by Ferrandiz et al.,[2] shave excision of 204 nevi was done and on histopathological examination 78.4% nevi were intradermal, 21.6% were compound. In both the studies none of the cases included were diagnosed as junctional nevi. However, in this study all the clinically diagnosed junctional nevi had insufficient tissue for histopathological diagnosis whereas it was adequate for compound and intradermal nevi. This could be because shave excision could not provide a proper specimen for junctional nevi since all were macules.
After shave excision, we found that on dermoscopic examination residual pigment was present in 91% of the nevi which was then removed using radiofrequency current. Overall recurrence was seen in 33% of the nevi at 6 and 12 weeks. Among the 33 nevi which recurred, 22 (66.67%) were hairy which was significantly higher as compared to nonhairy nevi.
In a study by Heck et al.,[14] after shave excision of 195 nevi, recurrences were observed in 30.3% nevi after 6 months of follow-up which was very much similar to our study. Bong and Perkins[13] performed shave excision of benign facial melanocytic nevi and recurrence was observed in 28% of nevi after 12 months of follow-up with significantly higher recurrence rate of 41% in hairy nevi. Ferrandiz et al.[2] observed recurrence after shave excision in 19.6% of CAMN.
Hair was present in none of the compound nevi and 28.73% of dermal nevi. Recurrence was seen in 88% of hairy nevi which was significantly higher as compared to nonhairy nevi.
The morphology of the nevi was neither significantly associated with the type of the nevi nor with the recurrence. Majority of both compound and intradermal nevi were papules. Recurrence was seen in papular nevi, dome shaped papules and papillomatous papules.
On performing dermoscopy immediately after shave excision, the residual pigment was seen in a significantly higher number of intradermal nevi as compared to compound nevi. Thus, a significantly higher number of intradermal nevi required radiofrequency for the removal of the residual pigment.
Both after 6 and 12 weeks, recurrence was seen in 37.93% of intradermal nevi which was significantly higher as compared to none of the compound nevi. Heck et al.[14] conducted a study and found that 84.7% of recurrent nevi were intradermal and 15.3% were compound nevi thus maximum recurrence was seen in intradermal nevi. Park et al.[15] in their study observed that 54% of recurrent nevi were compound, 32% were junctional and 9% were intradermal. These results were in discordance with our study. The reason for the discordance in results could be that most of the nevi (87%) included in our study were intradermal and only 8% were compound.
Visual analog scale was used for pain assessment and was performed immediately after the procedure. We found 67% of our patients had no pain and mild annoying pain in rest. At the end of 12 weeks, none of our patients were unsatisfied. The reason for most of the patients being satisfied with the cosmetic result could be attributed to the use of combination of two superficial modalities, shave excision and radiofrequency current, for the removal of nevi along with use of dermoscopy as an adjunct for detection of any residual pigment thus decreasing the risk of recurrences. A significantly higher number of patients with compound nevi were very satisfied as compared to intradermal nevi. This is because no recurrence was seen in compound nevi.
CONCLUSION
All the nevi diagnosed as benign using ABCD rule on dermoscopy were benign on histopathology as well. These are more likely to recur with shave excision particularly if they are hairy nevi. Shave excision is a minimally invasive and easily performed procedure. It can also provide a proper histopathological specimen for both intradermal and compound nevi but not for clinically diagnosed junctional nevi. Dermsocopy can also be used for assessing any residual pigment after shave excision and thus reducing the risk of recurrences. On combining shave excision with radiofrequency ablation and assessing by dermoscopy, majority of patients were satisfied with the cosmetic results with minimal or no pain following procedure. Using dermoscope for follow-up helps in early recognition of recurrence and thus appropriate treatment can be provided at the earliest.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
REFERENCES
- Clinicopathological analysis of acquired melanocytic nevi and a preliminary study on the possible origin of nevus cells. Am J Dermatopathol. 2020;42:414-22.
- [Google Scholar]
- Shave excision of common acquired melanocytic nevi: Cosmetic outcome, recurrences, and complications. Dermatol Surg. 2005;31:1112-5.
- [Google Scholar]
- Optimal management of common acquired melanocytic nevi (moles): Current perspectives. Clin Cosmet Investig Dermatol. 2014;7:89-103.
- [Google Scholar]
- Dermoscopic features of small, medium, and large-sized congenital melanocytic nevi. Ann Dermatol. 2017;29:26-32.
- [Google Scholar]
- ABCD rule. In: Marghoob AA, Manehy J, Braun RP, eds. Atlas of Dermoscopy (2nd ed.). United Kingdom: Informa Healthcare Publishing; 2012. p. :113-7.
- [Google Scholar]
- ABCD rule of dermatoscopy: A new practical method for early recognition of malignant melanoma. Eur J Dermatol. 1994;4:521-7.
- [Google Scholar]
- Measures of adult pain: Visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (Sf-36 Bps), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res (Hoboken). 2011;63:S240-52.
- [Google Scholar]
- Benign melanocytic lesions with emphasis on melanocytic nevi–A histomorphological analysis. J Path Nepal. 2018;8:1384-8.
- [Google Scholar]
- Principles of dermoscopy and dermoscopic equipment. In: Marghoob AA, Manehy J, Braun RP, eds. Atlas of Dermoscopy (2nd ed). United Kingdom: Informa Healthcare Publishing; 2012. p. :3-9.
- [Google Scholar]
- Round excision of small, benign, papular and dome-shaped melanocytic nevi on the face. Int J Dermatol. 2004;43:844-6.
- [Google Scholar]
- Deep shave excision of macular melanocytic nevi with the razor blade biopsy technique. Dermatol Surg. 2000;26:662-6.
- [Google Scholar]
- Shave excision of benign facial melanocytic naevi: A patient’s satisfaction survey. Dermatol Surg. 2003;29:227-9.
- [Google Scholar]
- Clinical and dermoscopic (in vivo and ex vivo) predictors of recurrent nevi. Eur J Dermatol. 2019;29:179-84.
- [Google Scholar]
- Recurrent melanocytic nevi: Clinical and histologic review of 175 cases. J Am Acad Dermatol. 1987;17:285-92.
- [Google Scholar]






