Translate this page into:
Recurrent lymphangioma circumscriptum: Treated with microneedling radiofrequency and topical sirolimus
*Corresponding author: Balkrishna Pralhadrao Nikam, Department of Dermatology, Krishna Institute of Medical Sciences, Karad, Maharashtra, India. mangeshnikam@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Deokar NP, Nikam BP, Hussain AA, Jamale V. Recurrent lymphangioma circumscriptum: Treated with microneedling radiofrequency and topical sirolimus. J Cutan Aesthet Surg. doi: 10.4103/JCAS.JCAS_50_23
Abstract
Lymphangioma circumscriptum is a “microcystic” lymphatic malformation. Different treatments have been tried with varying success. We report here a case of recurrent lymphangioma circumscriptum who was treated with microneedling radiofrequency (MNRF) and topical preparation or sirolimus cream with good improvement. A 14-year-old girl presented to outpatient department with a cluster of small asymptomatic blisters over the unilateral inguinal area which on histopathology was confirmed to be lymphangioma circumscriptum. The patient had similar lesions 3 years back which she got surgically excised. Since the last 6 months, she had a recurrence of the similar lesions so this time we chose MNRF every 40 days to treat this case which was combined with topical sirolimus 0.01% during and after the procedure. MNRF helps in neoelastogenesis and neocollagenosis, which leads to dermal thickening. It also acts as a drug delivery system by creating dermal channels. Sirolimus with its anti-lymphangiogenic properties helps prevent recurrence.
Keywords
Lymphangioma circumscriptum
MNRF assisted drug delivery
MNRF with topical sirolimus
INTRODUCTION
Lymphangioma circumscriptum is a “microcystic” lymphatic malformation. It appears as a cluster of small firm blisters filled with lymph. It has two components, a dermal vesicular and a subcutaneous cisternal component. Lymphangioma circumscriptum, with its cosmetic disfigurement, causes a great psychological burden on patients.
Microneedle radiofrequency (MNRF) is an office procedure with no downtime, causing dermal remodeling by neocollagenesis.1 It works by administering radiofrequency directly into various depths of the skin.2 Studies have proven the efficacy of MNRF in treating lymphangioma circumscriptum.2
Oral sirolimus has been reported as an efficient drug to reduce the volume and limit complications in vascular malformations, especially with lymphatic components. It decreases the number of vesicles, bleeding, oozing, and pain. Topical sirolimus in concentrations ranging from 0.0013% to 8% has been used previously with satisfactory results in lymphangioma circumscriptum.3
We present a case that was treated with a combination of the two proven modalities.
CASE REPORT
A 14-year-old girl presented with lesions over the thigh since 5 months. She had similar lesions 3 years ago which were surgically excised. Cutaneous examination revealed asymptomatic grouped papulovesicles over the left inguinal area, extending from the anterior superior iliac spine to the pubic tubercle measuring approximately 15 cm × 10 cm, giving an appearance of frog spawn [Figure 1a]. Dermoscopy showed yellowish-brown round areas [Figure 1b]. Histopathology showed dilatation of lymphatic channels confirming the diagnosis of lymphangioma circumscriptum [Figure 2].
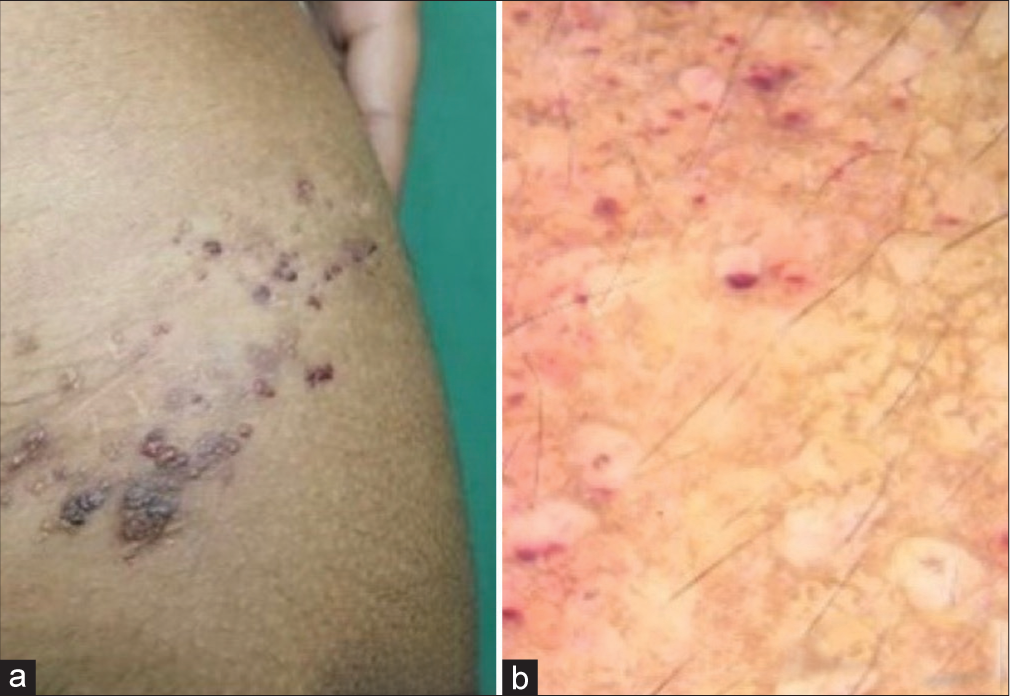
- Pretreatment photographs (a) hyperpigmented grouped papulovesicles forming an appearance of “frog spawn” overlying the scar mark from previous surgical excision. (b) Yellowish well- circumscribed round areas and few lacunae filled with blood.
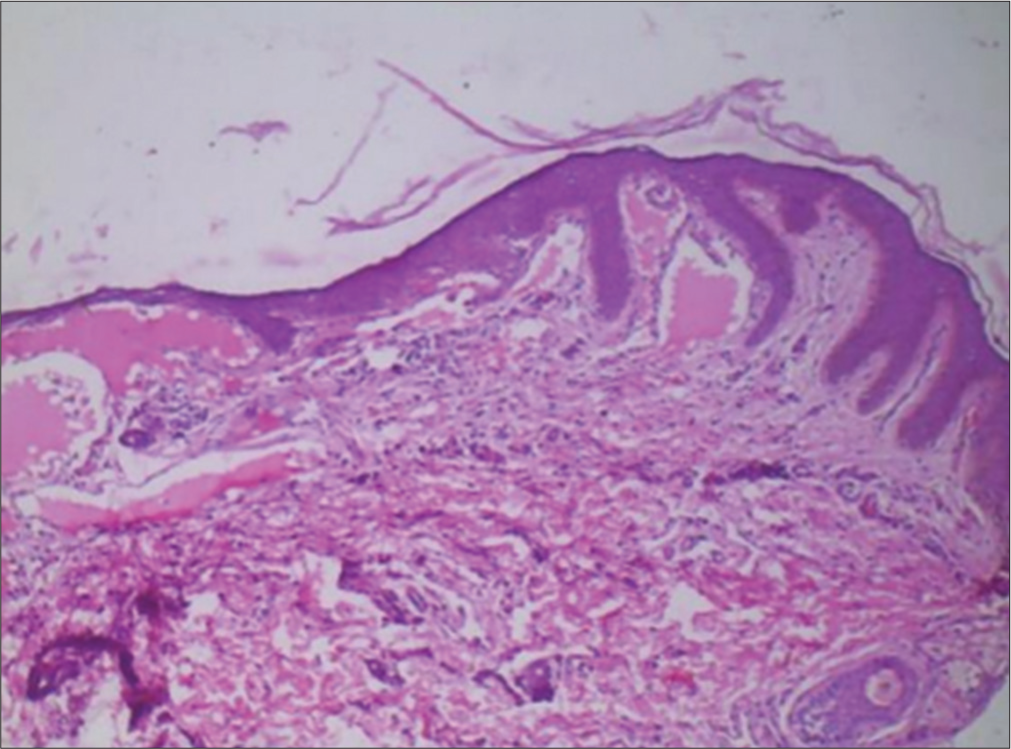
- Histopathology showing dilated lymphatic channels filled eosinophilic proteinaceous collection seen within widened dermal papillae (H&E ×10). H&E: Hematoxylin and eosin.
This being a case of recurrent lymphangioma, warranted an intervention that would ensure a good treatment outcome. MNRF and topical sirolimus, both have been used successfully in the treatment of lymphangioma circumscriptum. The combination of these two, theoretically would act synergistically and, may give better efficacy. So, we treated this case with a combination of both.
The sirolimus paste (0.01%) was made by crushing 50 tablets of 1mg of sirolimus and mixing in 5 grams of emulsifying cream with the help of an electrical stirring machine (Remi RQ 121). The patient was treated with a microneedle radiofrequency device (ENDYMED/PURE). The area was anesthetized with topical lidocaine 2.5% + prilocaine 2.5% cream 40 min before the procedure and local infiltration anesthesia with lignocaine 2% was given as and when required. MNRF was done on fractional mode with 3–3.5 mm and 2–2.5 mm depth and energy of 15 watts using a non-insulated tip. At every session, two consecutive passes of MNRF were given over the lesion, with the application of topical sirolimus (0.01%). A total of five sessions were done, at an interval of 6 weeks [Figure 3a and b]. The patient was also asked to apply the same topical sirolimus cream twice daily throughout the treatment period. Clinically significant improvement started after two sessions and a 90% improvement in the lesions was seen at the end of five sessions [Figure 4a]. Posttreatment dermoscopy of the lesions showed the disappearance of the lesions and blood-filled lacunae [Figure 4b].
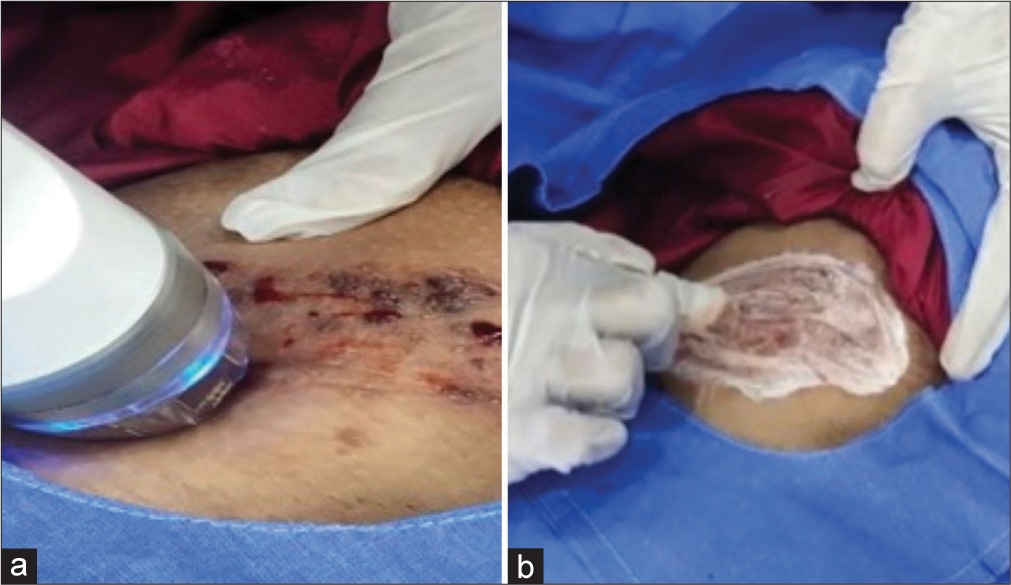
- Treatment (a) Microneedle radiofrequency (MNRF). (b) Application of sirolimus cream during the procedure.
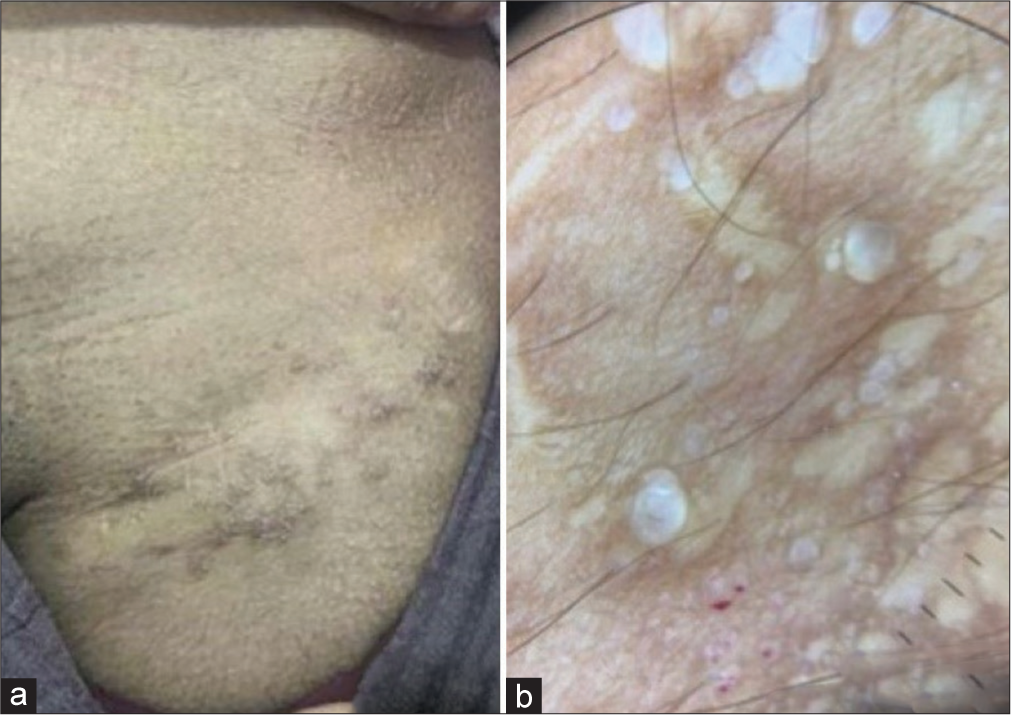
- Posttreatment 9 months (a) showing resolution of lesions and (b) dermoscopy showing resolution of blood-filled lacunae.
DISCUSSION
Cutaneous microcystic lymphatic malformations (CMLMs) present as clusters of vesicles filled with lymph and blood. Various treatments such as surgical excision, sclerotherapy, electrocoagulation, and cryotherapy have been attempted. However, most of these methods are invasive, prone to scarring, and have long recovery periods.4 Microneedle radiofrequency minimizes heat damage to the epidermis and exerts radiofrequency heat only to the target area. This has the advantage of minimal scarring and short recovery periods.5,6 In addition, overall remodeling of the dermal layer may help reduce the lymphatics and blood vessels thereby preventing recurrence. Sirolimus belongs to the mammalian target of rapamycin (mTOR) inhibitors and has anti-lymphangiogenic properties.7
The advantages of combining both modalities are multifold. MNRF destroys deeper tissue by coagulating the dilated lymphatics, helps in neocollagenesis due to trauma by needle penetration, and acts as a drug delivery system by creating dermal channels.8 Sirolimus with its anti-lymphangiogenic properties helps prevent recurrence. Further, lower concentrations of sirolimus cream can be used because of the channels created by MNRF, thereby reducing overall cost.
CONCLUSION
The results with this combination are satisfactory, as seen in our case. The aim of this case report was to encourage dermatologists to use multiple modalities to treat refractory cases instead of relying on one single or conventional treatment modality. Further, we recommend MNRF being used as a drug delivery system for other commonly used topicals.
Authors’ Contributions
All authors contributed equally. Neha Pralhad Deokar: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Balkrishna Pralhadrao Nikam: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Asma Arif Hussain: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review. Varsha Jamale: Concepts, Design, Definition of intellectual content, Literature search, Manuscript preparation, Manuscript Editing, and Manuscript review.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest
Dr Balkrishna Nikam is on the Editorial Board of the Journal.
Financial support and sponsorship
Nil.
References
- The clinical efficacy and safety of microneedling fractional radiofrequency in the treatment of facial wrinkles: A multicenter study with the INFINI system in 499 patients. Dermatol Surg. 2013;39:263-73.
- [Google Scholar]
- Microneedle radiofrequency treatment of lymphangioma circumscriptum. Dermatol Surg. 2019;45:1333-5.
- [CrossRef] [PubMed] [Google Scholar]
- A case of microcystic lymphatic malformation successfully treated with topical sirolimus. Dermatol Ther. 2018;31:e1267312673.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of lymphangioma circumscriptum with combined radiofrequency current and 900 nm diode laser. Dermatol Surg. 2006;32:790-4.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of lymphangioma circumscriptum with sclerotherapy: An ignored effective remedy. J Cosmet Dermatol. 2011;10:156-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lymphangioma circumscriptum treated with pulsed dye laser. Pediatr Dermatol. 2001;18:509-10.
- [CrossRef] [PubMed] [Google Scholar]
- Carbon dioxide laser for the treatment of microcystic lymphatic malformations (lymphangioma circumscriptum): A systematic review. Dermatol Surg. 2013;39:1147-57.
- [CrossRef] [PubMed] [Google Scholar]
- Lymphangioma circumscriptum treated with radiofrequency ablation. Indian J Dermatol. 2011;56:77-8.
- [CrossRef] [PubMed] [Google Scholar]






