Translate this page into:
Role of High Magnification Using Operative Microscope in Surgical Clearance of Glomus Tumor in Distal Phalanx: An Experience of 13 Cases
Address for correspondence: Dr. Narendra S. Mashalkar, Department of Burns and Plastic Surgery, St John’s Medical College and Hospital, Bengaluru, Karnataka, India. E-mail: plasticnaren2005@yahoo.co.in
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Glomus because of their small size in fingers presents difficulty in clear visualization in the operation theater and requires magnifying techniques. Because of the dearth of infrastructure in many hospitals, the excision of these is done with either no or inadequate magnification. Magnetic resonance imaging (MRI) has become the gold standard investigation as glomus tumors can be visualized on radiology very clearly. The reason for recurrence given in the literature is access to tumors by the type of surgical approach for clear visualization, but high magnification being the most important, as the size of glomus is very small has no or limited mention in the literature. Being in a tertiary care hospital, we have analyzed the role of high magnification in the excision of glomus and its impact on recurrence as the end outcome.
Aim:
To understand the role of intraoperative high magnification using operative microscope and its advantages in the surgical clearance of glomus tumor of fingers.
Settings and Design:
Retrospective record review.
Materials and Methods:
Thirteen cases of glomus tumor in the phalanges over a period of 7 years were operated under operative microscope with a magnification ranging from 10× to 12.5×; data and mean follow-up to 5.5 years have been analyzed.
Results:
Age ranged from 24 to 72 years; all the glomus tumors were in the distal phalanx. Three cases had bony erosion on MRI scan. We had an equal distribution of three cases each in the thumb, ring, and middle finger.
Conclusions:
(1) High magnification with operative microscope is essential during the excision of glomus tumor especially in the distal phalanx in order to prevent recurrence; (2) advantages of high magnification are clear delineation with complete tumor excision, with meticulous repair of nail bed.
Keywords
Glomus tumor
high magnification
operative microscope
recurrence
KEY MESSAGES
High magnification is a requirement for the clear delineation of tumor with a complete tumor excision to prevent recurrence.
INTRODUCTION
Glomus is a type of benign tumor arising from neuromyoarterial cells[1] occurring in the hand[2]; they are tiny but present with severe pain with temperature variation.[34] Magnetic resonance imaging (MRI) has become the gold standard investigation as these can be visualized clearly.[5] Clear visualization in the operation theater requires magnifying techniques. Because of the dearth of infrastructure in many hospitals, excision is done with either no or inadequate magnification. The reason for recurrence given in the literature is access to tumors by the type of surgical approach for clear visualization, but high magnification being the most important, as the size of glomus is very small has no or limited mention in the literature.[678] The complete excision under high magnification is essential to give gratifying results and necessary for the prevention of recurrence.
Even though using magnification for the excision of glomus tumor has become a standard practice, the literature is very scarce in giving a detailed description of using microscopic high magnification. Hence, we have made an attempt to analyze the role of high magnification using operative microscope in the excision of glomus and its impact on recurrence as the end outcome
MATERIALS AND METHODS
We have operated on 13 cases of glomus tumor in the phalanges over a period of 7 years under operative microscope with a magnification varying from 10× to 12.5×. We routinely operate all cases under brachial block with application of tourniquet inflated at 250 mmHg. Our microscope is OPMI VARIO from Carl Zeiss but without photography or video-recording feature. We have done a retrospective record analysis and have called the patient on telephone and have asked them about the pain in the operated finger.
RESULTS
The age group ranged from 24 to 72 years with seven males and six females; all the glomus tumors were in the distal phalanx, and we had one case in the distal phalanx of the third toe. Three cases had bony erosion on MRI scan. We had an equal distribution of three cases each in the thumb, ring, and middle finger with two cases in the index and one in the little finger. MRI was done for all the cases [Figure 1] except in three cases where we did not consider MRI as a necessity.

- MRI of glomus tumor
All our cases had dramatic relief in pain in the early postoperative period except minimal postoperative pain, and the patient could very well distinguish the pain they had preoperatively. The entire glomus tumor was located on the dorsal aspect except for one case; the location was on the volar aspect.
We have done a retrospective record analysis of the data and have mean follow-up to 5.5 years, obtained by a telephonic interview.
To specifically mention our long-term follow-up, we got a maximum follow-up of 6 years for two patients, 7 years for three patients, 8 years for one patient, and 3 years for two patients, our mean follow-up being 56 months. The rest three patients had a range of follow-up from 6 to 21 months. We could not follow up two patients as their contact numbers had changed.
DISCUSSION
We have presented glomus tumors in the distal phalanx in the age group of 24–72 years; eight cases of 13 were young adults in contrast to Samaniego et al. who stated it affects middle age[9]; we had one case in the distal phalanx of the third toe. In our series, subungual tumors were more common in males, but Gombos and Zhang have reported that females have increased incidence of subungual glomus distribution.[10] Muramatsu et al. have reported 11 female patients in their series of 12 cases; however, in our series, three out of 13 cases (23%) had bony erosion on MRI, VanGeertruyden et al. reported 36% and Chen et al. reported 48% in their respective series.[1112] We had an equal distribution of three cases each in thumb, ring and middle finger with two cases in the index and one in the little finger. We have done MRI for 10 cases confirming glomus; except in three cases, patients had classical clinical signs and symptoms and confirmed glomus intraoperatively. All the lesions were sent to histopathology and diagnosis was confirmed.
The most common concerns for patient with glomus tumor is the recurrence of pain; etiological factors related in the literature are inadequate excision because of poor visualization based on surgical approach remains to be ascertained,[13] and the other etiology is synchronous lesions.[4]
Recurrence are again divided into early and late: early recurrence are usually due to inadequate excision,[9] and late recurrences are due to synchronous or second tumor.[49] To counter inadequate visualization, the approach would be to choose a proper surgical exposure technique and more importantly magnification. To counter the synchronous and the tiny size of tumor, preoperative localization by high resolution MRI can be employed now.[9]
The role of high magnification using operating microscope intraoperatively has to be given significant importance. We have operated all our cases with operative microscope with a magnification at 10× to 12.5×. The microscopic appearance of glomus tumor with tourniquet inflated appears reddish-yellow [Figure 2] with a bluish hue color, and there is a very clear demarcation from the surrounding nail bed; the capsule overlying the glomus tumor is very thin, and upon incision, there is a clear plane available between the tumor and the adjacent nail bed soft tissue; dissection all around the tumor is easy and can be easily retrieved from the underlying bed; the depth of erosion into the bone can be made out with high magnification [Figure 3]. We routinely remove the total nail plate [Figure 4]; hence, normal area of the surrounding healthy nail bed can be visualized under operating magnification with greater details, and if there are any synchronous lesions, it can be retrieved; however we have not encountered any synchronous lesions till now. A meticulous repair of the nail bed postremoval can be managed under operating magnification.
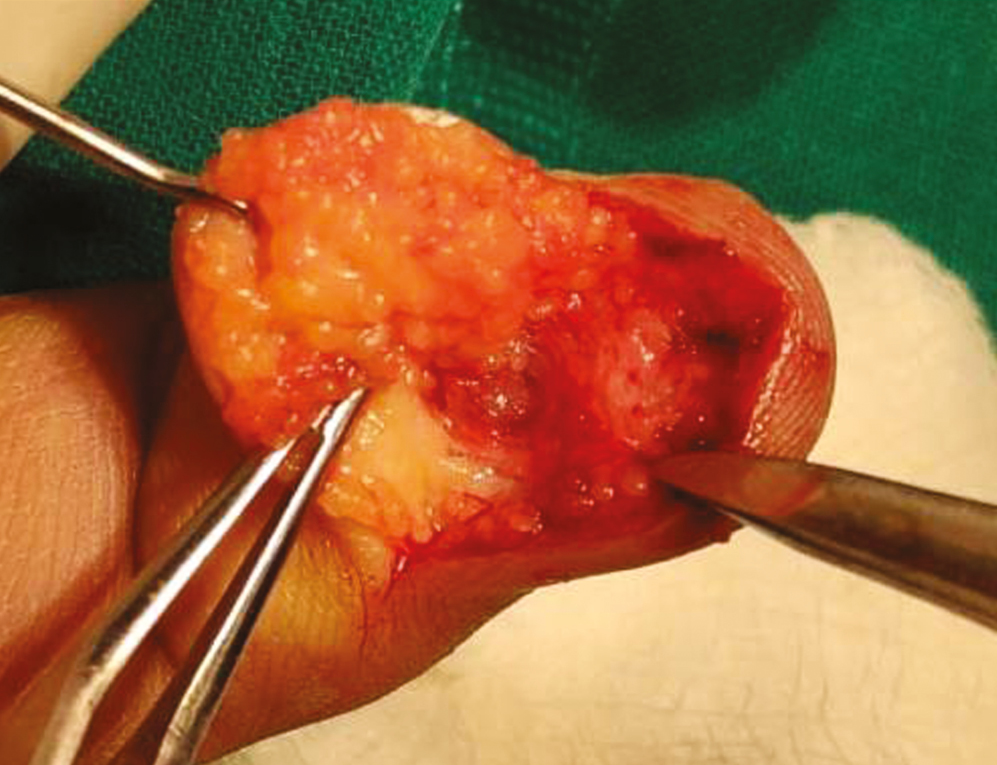
- Intraoperative view of glomus before excision
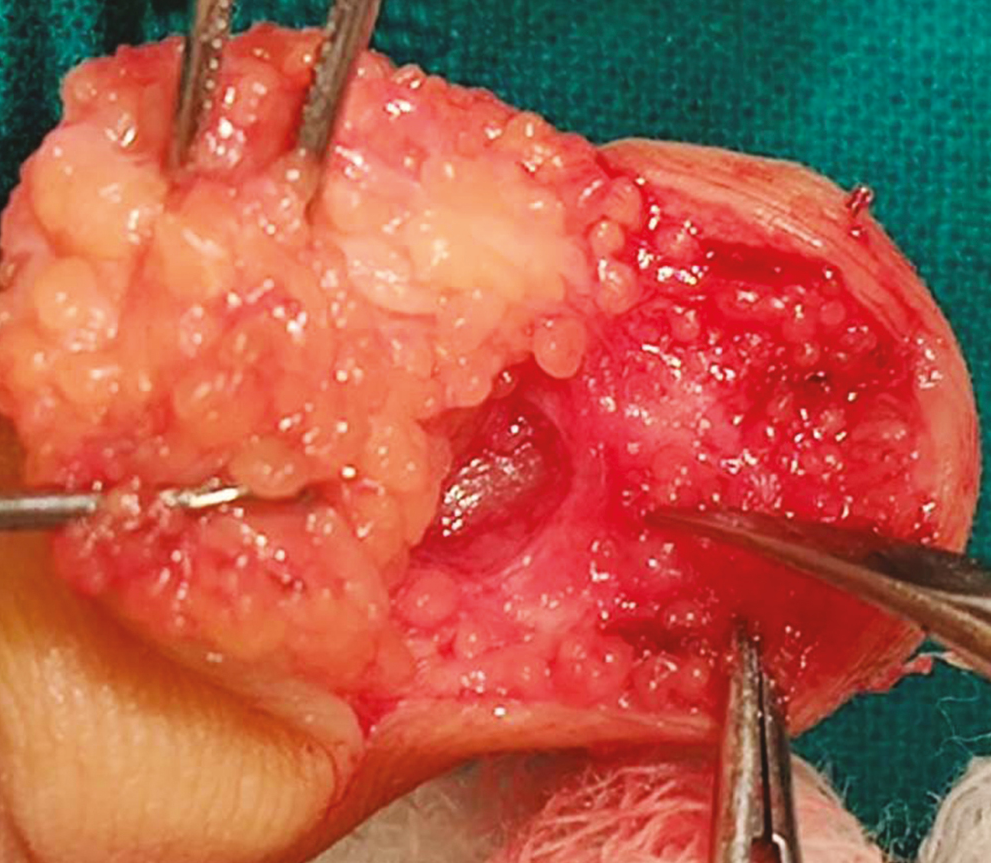
- Intraoperative view showing bony erosion

- Glomus after total nail plate removal
The current literature search on magnification has not yielded any details of the magnification used. Muramatsu et al. have mentioned that microscope allows careful visualization of the tumor, Lee et al. have mentioned surgical microscope to localize and excise the tumor and to repair the nail bed. Huang et al. have mentioned that microscopic surgical excision has helped them to completely remove the glomus tumor, but in none of these above articles, there is a detailed description of microscopic magnification that has been used with the details of the intraoperative microscopic appearance of the glomus tumor. Hence, with the paucity of magnification and details in the literature, we have made an attempt to associate the significance of intraoperative high magnification in delineating, dissecting, retrieval of glomus tumor, and observing the peripheral normal nail bed and its relation to the ultimate outcome, that is recurrence. One of the limitations of study quoted by Huang et al. is the short follow-up period. Garg et al. have also mentioned about magnification improving the clearance of tumors.[14]
We had done a telephonic questionnaire to asses for the pain component after excision for our patients, as we were prevailing in the current COVID times and physical follow-up was very difficult for patients because of lockdown restrictions, and the literature search also quotes about telephonic interview as adequate evidence for end outcome measurement.
Eleven of 13 of our cases had no pain. Our long-term mean follow-up being 56 months is quite reliable, as among the entire literature search, the maximum long-term follow-up of 48 months is noted by Huang et al.
CONCLUSION
High magnification with operative microscope is essential and has to be used routinely during the excision of glomus tumor especially in the distal phalanx in order to prevent recurrence.
The advantages of high magnification with operative microscope are clear delineation of tumor with complete tumor excision with the observation of the surrounding nail bed for any suspicious lesions, with meticulous repair of nail bed.
Limitation and further scope
A large series follow-up would be ideal to stamp the superiority of high magnification in the excision of glomus tumor.
Comparison of loop magnification with operative microscope magnification would give us better understanding about the role of high magnification and its ultimate importance.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Nil.
REFERENCES
- Vascular disorders. In: Green DP, Hotchkiss RN, Peterson WC, Wolfe SW, eds. Green’s Operative Hand Surgery. Philadelphia, PA: Elsevier; 2005. p. :2312.
- [Google Scholar]
- Subungual glomus tumours of the hand: Diagnosis and treatment of 14 cases. Scand J Plast Reconstr Surg Hand Surg. 2003;37:121-4.
- [Google Scholar]
- Glomus tumours of the hand: Review of the literature and report on twenty-eight cases. J Bone Jt Surg Am. 1972;54:691-703.
- [Google Scholar]
- Subungual glomus tumors of the hand: Treated by transungual excision. Indian J Orthop. 2015;49:403-7.
- [Google Scholar]
- Outcome of microscopic excision of a subungual glomus tumor: A 12-year evaluation. Dermatol Surg. 2015;41:487-92.
- [Google Scholar]
- Subungual glomus tumours of the hand: Diagnosis and outcome of the transungual approach. J Hand Surg Eur Vol. 2009;34:685-8.
- [Google Scholar]
- Subungual glomus tumours: Diagnosis and microsurgical excision through a lateral subperiosteal approach. J Plast Reconstr Aesthet Surg. 2014;67:373-6.
- [Google Scholar]
- [Key diagnostic features and treatment of subungual glomus tumor] Actas Dermosifiliogr. 2009;100:875-82.
- [Google Scholar]
- Glomus tumors of the hand, a retrospective study of 51 cases. J Hand Surg. 1996;21B:257-267.
- [Google Scholar]
- The use of ultrasonography in preoperative localization of digital glomus tumors. Plast Reconstr Surg. 2003;112:115-9; discussion 120.
- [Google Scholar]
- Digital glomus tumors: A 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg. 2004;114:1486-9.
- [Google Scholar]






