Translate this page into:
Small Incision Upper Blepharoplasty in the Treatment of Upper Eyelid Solitary Nasal Pad Fat Protrusion
Address for correspondence: Dr. Tarek R. Elhamaky, Department of Ophthalmology, Faculty of Medicine, Benha University, Benha, Qalyubia Governorate 13511, Egypt. E-mail: dr_thamakyy@yahoo.com; tarek.mahgob@fmed.bu.edu.eg
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Purpose:
The aim of this article is to investigate the efficacy of small incision blepharoplasty in the treatment of upper eyelid single nasal pad fat bulge.
Materials and Methods:
This is a prospective study of 43 eyes of 24 patients who underwent small incision upper blepharoplasty for the treatment of solitary nasal pad fat bulge. All patients underwent a comprehensive ophthalmic examination, periorbital evaluation, and patient satisfaction evaluation using Global Aesthetic Improvement Scale (GAIS) and Blepharoplasty Outcomes Evaluation (BOE) at baseline, 1 week, 3 months, and 6 months after the surgery. All patients underwent small incision upper eyelid blepharoplasty for excision of nasal fat pad bulge.
Results:
Baseline nasal fat bulge was graded into grades 1, 2, and 3 in 4 (9.3%), 12 (27.9%), and 27 (62.8%) eyes, respectively. While at 6-month follow-up, grade 0 was recorded in 38 (88.4%) eyes, and grade 1 was recorded in 5 (11.6%) eyes. The mean operative time was 11.7 ± 1.9 min. GAIS showed degrees 1, 2, and 3 in 2 (8.3%), 19 (79.2%), and 3 (12.5%) patients at 6-month follow-up, respectively. Twenty-two patients (91.7%) reported a BOE scale of more than 95%, whereas two patients (8.3%) reported a scale of 80–90% at 6-month follow-up.
Conclusion:
Our cohort highlights the beneficial effects of small incision upper blepharoplasty in the treatment of upper eyelid solitary or lone nasal pad fat bulge, providing a safe, short-timing, and effective option.
Keywords
Blepharoplasty
fat
nasal
small incision
INTRODUCTION
The upper eyelid fat is divided into nasal (medial) and central (pre-aponeurotic) fat pads by the superior oblique muscle tendon and the medial horn of the levator aponeurosis.[12]
The whitish nasal fat pad is similar in appearance to intraconal orbital fat, whereas the central fat pad is more yellow in color and similar in appearance to the body adipose tissue. The nasal fat pad contains more connective tissues and less carotenoids, compared with the central fat pad explaining the difference in their gross appearance. The nasal fat pad may be an excellent source for free fat grafting due to its progenitor cell composition.[345]
The upper eyelid nasal fat pad is often prolapsed with aging. There is an apparent increase in the volume of the upper eyelid nasal fat pad and a decrease in the volume of the central fat pad with advancing age due to the overall atrophic changes of the central fat pad.[2]
The upper eyelid nasal fat pad bulge is a common cosmetic problem creating a tired and unsightly appearance that requires nasal fat removal for upper eyelid rejuvenation. The upper eyelid blepharoplasty is one of the commonest esthetic surgeries for upper eyelids. Traditional blepharoplasty includes removing the medial fat pad by opening the entire horizontal length of the eyelid. This requires an incision of the entire length of the eyelid.[46,7]
This cohort aims to investigate the efficacy of the small incision technique in the management of the upper eyelid solitary nasal fat pad bulge.
PATIENTS AND METHODS
Patient selection
this is a prospective study of 43 eyes of 24 patients who underwent small incision upper blepharoplasty for the treatment of solitary nasal pad fat bulge between May 2020 and November 2021.
Inclusion criteria
at least 18 years of age patients with upper eyelid solitary nasal pad fat bulge.
Exclusion criteria
upper eyelid dermatochalasis, upper eyelid blepharoptosis, central fat pad protrusion, and other orbital or eyelid disease.
Patient evaluation
All patients underwent a comprehensive ophthalmic examination, visual field test (VFT), and periorbital evaluation at baseline, 1 week, 3 months, and 6 months after the surgery.
-
•
The periorbital evaluation includes assessment of globe position, palpebral fissure size and shape, upper eyelid position and symmetry, brow position and symmetry, skin assessments, Bell’s phenomenon, and facial nerve function.[8]
-
•
-
•
Duration of surgery from the time of the incision to the closure of the wound is measured by a stopwatch in minutes.
-
•
Patient satisfaction evaluation:
-
1.
Global Aesthetic Improvement Scale (GAIS)[10];
-
2.
Blepharoplasty Outcomes Evaluation (BOE): Six items are scored on a 0–4 scale, with 0 being scored for the most negative response and 4 being scored for the most positive response. Dividing the total score by 24 and multiplying by 100 yields the scaled instrument score. This range is 0–100, with 0 representing the least patient satisfaction and 100 representing the most patient satisfaction.[11]
-
-
•
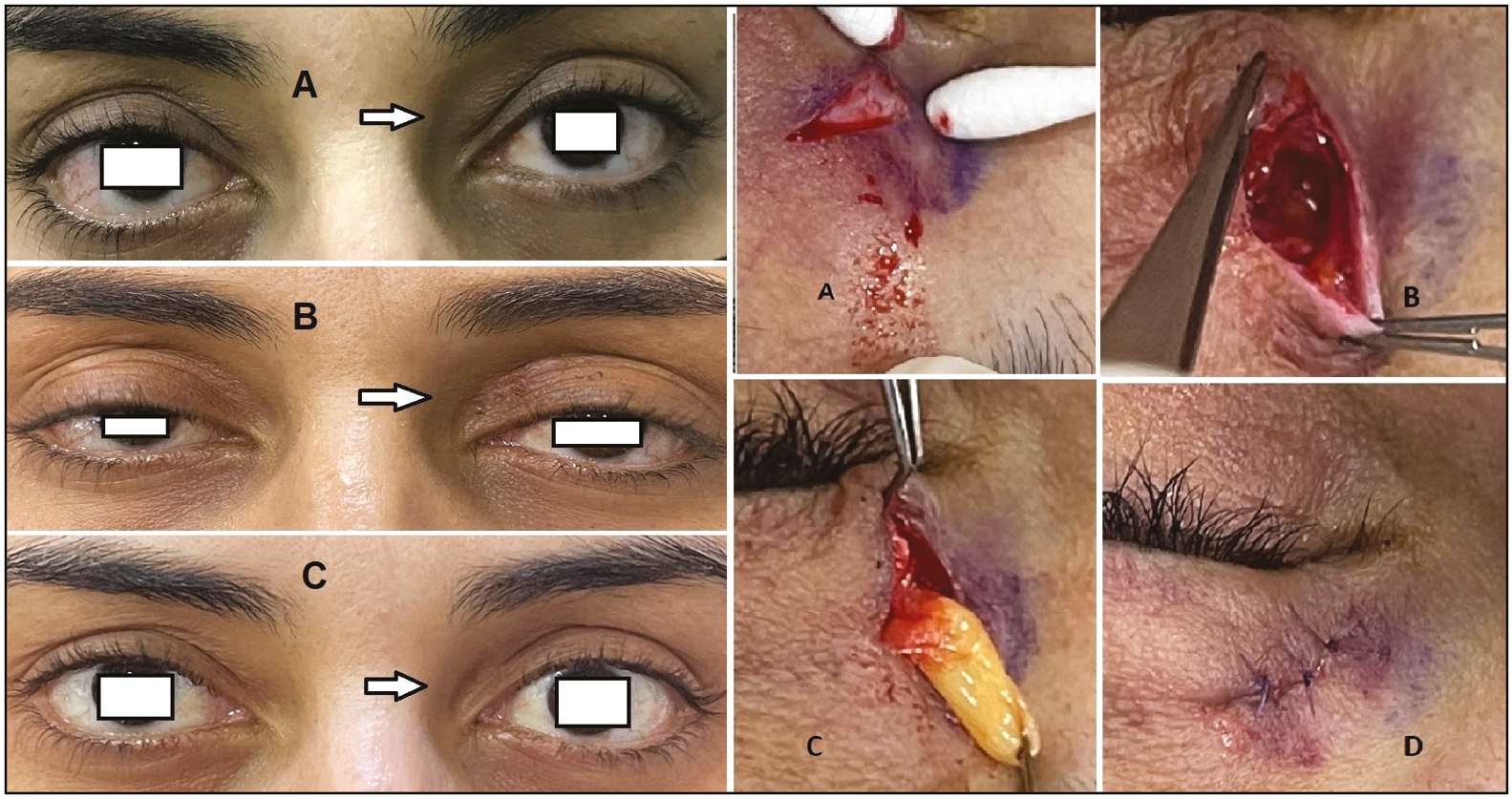
- Left: (A) baseline photograph of the left eye with nasal fat pad bulge, (B) 6-month post-operative photograph, and (C) 2-year follow-up photograph. Right: surgical technique: (A) small incision 4 mm in the nasal eyelid crease, (B) blunt dissection of orbicularis muscle toward nasal fat pad, (C) nasal fat pad isolation and excision, and (D) wound closure
Surgery
Pre-operative markings: The upper eyelid medial crease is marked with the patient in the upright primary position. A mark is placed 4 mm in length just inferior to the eyelid crease. Marking is rechecked with the patient in the supine position after surgical preparation and draping.[914]
Surgical procedure: All procedures are performed under local and conscious sedation. The skin is infiltrated subcutaneously with 2–5 mL of lidocaine 1% with 1:100,000 epinephrine after surgical preparation and draping. Incision of the skin for 4 mm is done with a scalpel blade. Separation of the nasal skin edges of the wound for surgical exposure was achieved. Blunt dissection of nasal orbicularis muscle was performed. After identification and proper isolation of the nasal fat pad, a local anesthetic was injected into the fat pad and then it was clamped with a hemostat and excised with Colorado tip electrocautery. The eyelid skin closure was done with two to three interrupted 6-0 Prolene sutures [Figure 1].[1415]
Post-operative treatment: It includes application of topical antibiotic and steroid ophthalmic ointment twice daily on the incisions, cold compresses at 30-min intervals for the first 3 days, and head elevation during sleep.[16]
Primary outcome measures
Included nasal fat grading and patient satisfaction at 6-month follow-up compared with baseline
Statistical analysis
Variables were expressed as a percentage or mean ± standard deviation. SPSS Windows version 16.0 (SPSS, Chicago, IL, USA) was applied for statistical analysis. Paired Student’s t-test was used for statistical analysis. A P-value of less than 0.05 was statistically significant.
RESULTS
Study population
This is a prospective study of 43 eyes of 24 patients who underwent surgical treatment of upper eyelid nasal pad fat bulge from May 2020 to November 2021. Mean follow-up was 7.6 ± 1.6 months (range 6–11 months). Bilateral nasal fat pad bulges were recorded in 19 (79.2%) patients. The mean age of patients was 40.8 ± 5.6 years (range 33–51) with 21 females (87.5%) and 3 males (12.5%). Primary and secondary nasal fat excision was done in 33 (76.7%) and 10 (23.3%) eyes, respectively.
Clinical results
Baseline nasal fat bulge was graded into grades 1, 2, and 3 in 4 (9.3%), 12 (27.9%), and 27 (62.8%) eyes, respectively. While at 6-month follow-up, grade 0 was recorded in 38 (88.4%) eyes and grade 1 was recorded in 5 (11.6%) eyes. The mean operative time was 11.7 ± 1.9 min. GAIS showed degrees 1, 2, and 3 in 2 (8.3%), 19 (79.2%), and 3 (12.5%) patients at 6-month follow-up, respectively. The mean baseline BOE increased significantly from 30.1 ± 4.4 points to 84.4 ± 4.3 points at 6-month follow-up. BOE scale was 70–80%, 80–90%, and more than 90% in 4 (16.7%),18 (75%), and 2 (8.3%) patients at 6-month follow-up, respectively.
Safety
Local anesthesia and conscious sedation were used in all surgeries. No serious ocular adverse events were recorded in our study. Minimal post-operative eyelid edema and ecchymosis were recorded in the majority of cases. Nasal fat pad re-excision was done in one patient 5 months after the initial procedure. None of the patients reported a scar at the incision site. Post-operative residual upper eyelid fullness, hollowness, or sulcus depression was not recorded.
DISCUSSION
The upper eyelid fat pads show unique behavior and differential volume changes with advancing age. The orbital septum and orbital fat relaxation aggravate sagging, leading to a fatigued tired appearance. The reduction of the nasal fat pad improves a tired eyelid appearance.[4]
The standard blepharoplasty procedure involves removing excess skin, preserving the central fat pad, and conservative removal of the nasal fat pad yields good results and high patient satisfaction. The open sky blepharoplasty approach involves traditional long horizontal upper eyelid incision to visualize the different fat compartments of the upper eyelid. This approach is not necessary to successfully and completely excise lone nasal fat pad bulge.[417,18]
Our small incision blepharoplasty procedure shows good cosmetic results and patients’ satisfaction in the treatment of either primary or secondary lone medial fat bulge cases.
Our study adopted a small incision blepharoplasty procedure which is similar to a stab incision technique of Barbarino et al.,[7] who concluded that the stab incision procedure for upper medial fat pad removal is a safe, effective, and time-efficient surgery yielding an aesthetically pleasing result. Both procedures adopt the same principle; minimally invasive techniques without skin excision to cover the slight concavity and minimize the skin closure tension should decrease the chance of medial canthus scarring. Small incision procedure follows the same pre-operative and post-operative precautions for a traditional blepharoplasty and intraoperative meticulous orbital fat removal and hemostasis.[1920]
Barbarino et al. applied a stab incision through the skin, muscle, and septum, whereas in our cohort, a skin incision followed by blunt dissection of the nasal orbicularis muscle toward the nasal pad of fat was done.
Traditional bilateral upper eyelid blepharoplasty with fat removal required approximately 1 h. Barbarino et al.[7] reported that the stab procedure for medial fat pad removal took approximately 5–10 min. The mean operative time in our cohort was 11.7 ± 1.9 min.
Our procedure belongs to tissue and orbital fat excision techniques which may lead to a high crease, large tarsal platform and a generally hollow upper sulcus. Nasal fat repositioning in upper blepharoplasty can be a useful adjunct to traditional surgery as a preventative measure for post-operative superior sulcus depression and hollowing, minimizing the volume-deficient results. Fat repositioning-related complications included ptosis, pseudo-Brown syndrome, and excessive swelling.[921,22]
The medial fat pad prolapse can be easily diagnosed by inspection only. Vaidya et al.[6] reported patients with malignant lymphoma mimicking the medial fat pad prolapse, highlighting the importance of rubbery and hard mass palpation for the diagnosis.
The limitations of this study include short follow-up interval and absence of the control group.
Although our nasal fat excision with small incision upper blepharoplasty and nasal fat repositioning upper blepharoplasty techniques has different indications, further studies, with longer follow-up, are needed to more critically assess eyelid volumetric changes.
CONCLUSION
Our cohort highlights the efficacy of small incision upper blepharoplasty in the treatment of upper eyelid solitary nasal pad fat bulge, providing a safe, short-timing, and effective option.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Study approval
The local Ethics Committee of Ibn Nafees Medical Center, Abu Dhabi, UAE approves this study. The study followed the tenets of the Declaration of Helsinki.
ClinicalTrials.gov ID of this study is NCT04689230.
Data sharing statement
All data used to support the findings of this study are available from the corresponding author upon request without an end date.
Authors contribution
The manuscript has been read and approved by the author.
Acknowledgement
No substantial contribution was provided for this submission.
References
- Upper eyelid blepharoplasty with voltaic arc dermabrasion. J Craniofac Surg. 2018;29:2263-6.
- [Google Scholar]
- Modified upper blepharoplasty using combination of incision and nonincision surgical approaches. J Craniofac Surg. 2019;30:235-6.
- [Google Scholar]
- Analysis of eyelid fat pad changes with aging. Ophthalmic Plast Reconstr Surg. 2011;27:348-51.
- [Google Scholar]
- Malignant lymphoma mimicking medial fat pad prolapse: A pitfall for upper eyelid rejuvenation. J Craniofac Surg. 2020;31:e359-60.
- [Google Scholar]
- The stab incision procedure for upper eyelid medial fat pad removal. Am J Cosmet Surg. 2012;29:141-4.
- [Google Scholar]
- Brow/upper lid anatomy, aging and aesthetic analysis. Facial Plast Surg Clin North Am. 2015;23:117-27.
- [Google Scholar]
- Nasal fat preservation in upper eyelid blepharoplasty. Ophthal Plast Reconstr Surg. 2011;27:352-5.
- [Google Scholar]
- Safety and efficacy of a volumizing hyaluronic acid filler for treatment of HIV-associated facial lipoatrophy. JAMA Dermatol. 2017;153:61-5.
- [Google Scholar]
- Outcomes research in facial plastic surgery: A review and new directions. Aesthetic Plast Surg. 2020;44:1210-5.
- [Google Scholar]
- Fat grafting in the hollow upper eyelids and volumetric upper blepharoplasty. Plast Reconstr Surg. 2017;140:889897.
- [Google Scholar]
- Six-position, frontal view photography in blepharoplasty: A simple method. Aesthetic Plast Surg. 2018;42:1312-9.
- [Google Scholar]
- Refinements in upper blepharoplasty: The five-step technique. Plast Reconstr Surg. 2018;141:1144-6.
- [Google Scholar]
- Upper eyelid blepharoplasty: Evaluation, treatment, and complication minimization. Semin Plast Surg. 2017;31:51-7.
- [Google Scholar]
- A comprehensive approach to upper eyelid rejuvenation surgery. Aesthetic Plast Surg. 2021;45:1047-55.
- [Google Scholar]
- The orbital oval balance principle: A morphometric clinical analysis. Plast Reconstr Surg. 2018;142:451e-61e.
- [Google Scholar]
- Integrating fat graft with blepharoplasty to rejuvenate the Asian periorbita. Plast Reconstr Surg Glob Open. 2019;7:e2365.
- [Google Scholar]
- Transconjunctival blepharoplasty for upper and lower eyelids. Plast Reconstr Surg. 2010;125:384-92.
- [Google Scholar]
- Minimally invasive complementary adjuncts to upper blepharoplasty. Master Techniques in Facial Rejuvenation E-Book. 2018;107
- [Google Scholar]
- Midface and Periocular Rejuvenation, An Issue of Facial Plastic Surgery Clinics of North America, E-Book. Philadelphia, PA: Elsevier Health Sciences; 2015.






