Translate this page into:
Soft-Tissue Correction Method for a Sunken Eyelid
Address for correspondence: Dr. Mariam Tsivtsivadze, Department of Aesthetic and Plastic Surgery, “Total Charm,” V. Orbeliani Street No. 18, 0105 Tbilisi, Georgia. E-mail: m.tsivtsivadze@aptos.ge
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The periocular area is one of the initial parts of the face that show signs of aging, where patients usually worry about the visual manifestations of aging, such as the sunken lower eyelid. The condition is usually caused by iatrogenic factors or involutional changes in the periocular area. This study aimed to develop and improve surgical methods to fill the sunken lower eyelids and examine their efficacy and safety. This study included 26 patients who had been treated with the musculofascial flap transposition method from the upper to the lower eyelid, under the posterior lamella. In the presented method, a deepithelized triangular musculofascial flap with a lateral feeding pedicle was transposed from the upper eyelid to the lower eyelid tear through depression. In all patients, the method achieved either a complete or a partial elimination of the defect. The proposed method to fill a defect of soft tissues in the arcus marginalis can be considered useful if upper blepharoplasty has not been performed previously and the orbicular muscle has been preserved.
Keywords
Blepharoplasty
lower eyelid
musculofascial flap
periorbital deformities correction
periorbital rejuvenation
sunken eyelid
INTRODUCTION
Relief disturbance of the lower eyelid is one of the first aging-associated changes noticed in the face.
Involutional changes are known to affect the peri-orbicular convexities and grooves. The convexities (fatty hernias and malar bags) can be successfully corrected through resection methods by either lifting or redistributing the content of the fatty packs.[12345] The lower eyelid blepharoplasty procedure involves removing excess skin, muscle, and fatty-tissues; sometimes surgeons remove excess fatty-tissue from the lower eyelid, and its causes sunken eyes.
However, even if there were no excess tissues in the periorbital area, deficits of the grooves and tissue on the boundary of the cheek-eyelid junction can cause an esthetic problem. Frequently, blepharoplasty has been known to cause esthetic deformation. Studies have suggested that these deformations can be eliminated through surgical intervention in the midfacial area.[234567] Some popular methods are lipo-lifting or filling with synthetic components.[8] However, the results of using various fillers in such cases are not always predictable as they can quickly absorb, or visually appear as protrusions after encapsulation.
MATERIALS AND METHODS
The method we used aimed to preserve tissues and create a flap and use it to fulfill the defects of the lower eyelid. We treated patients who had tissue deficits at the cheek-eyelid junction using the deepithelized triangular musculofascial flap transposition method, at a private clinic within 24 months from September 2006 to September 2008. This study included 26 patients who were treated with the mentioned method from the upper eyelid to the lower one, under the posterior lamella.[910] The inclusion criteria for the study were the presence of tissue deficits of the cheek-eyelid junction and no history of upper blepharoplasty (i.e., the orbicular muscle in the upper eyelid area has been preserved).
Moreover, they often came to us mainly for upper blepharoplasty, and when we noted the “emptiness” of the lower eyelid, we suggested an operation of the upper eyelid with a similar modification. However, less often, they complained about “sunken” lower eyelids, and since we had the possibility of filling the eyelids with a flap from the upper eyelid, we suggested the transposition method.
Surgical technique
The surgeon performed a classical incision on the skin (6–8 mm above the upper-eyelid eyelash crease) for upper blepharoplasty. We then implemented skin de-epidermization, deepened the incision, and created a triangular flap with a lateral feeding pedicle on the lateral upper eyelid. The flap consisted of the orbicularis muscle palpebral part and the levator aponeurosis (fascia).
It is well known that this kind of a “sandwich” (between muscle fascia) maintains form and has good vascularization. In our case, the flap’s blood supply was obtained from the pedicle on the lateral upper eyelid whose supply was provided by the lateral palpebral artery, a branch of the lacrimal artery. Note that the arterial supply of the palpebral portion of the orbicularis oculi muscle comprised two arcades: the marginal and peripheral, which followed the same direction as the muscle fibers. The pedicle was mobilized in such a way that the turn of the flap around the pedicle did not deform the tissues [Figure 1].
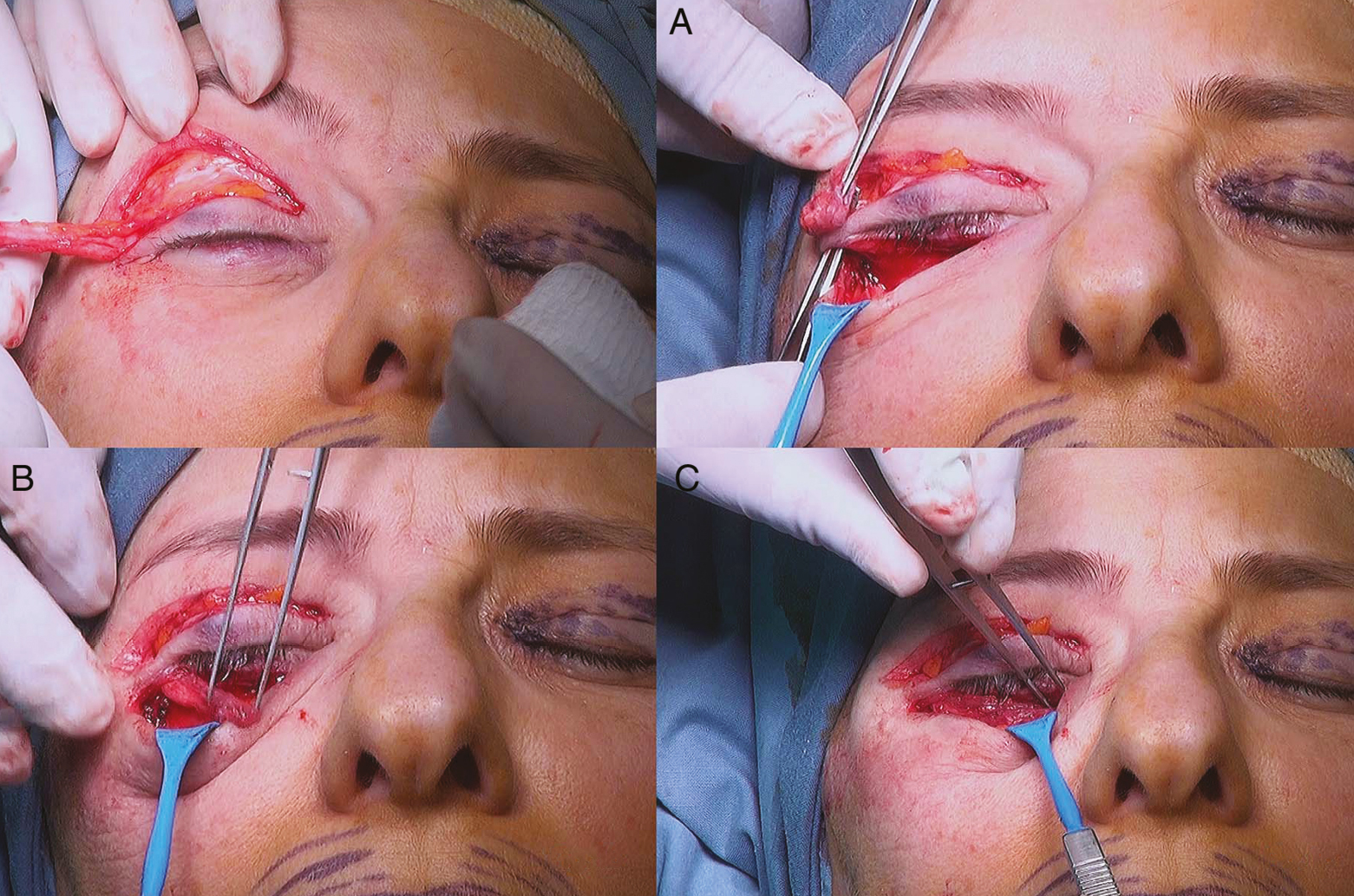
- An intraoperative image of a 42-year-old patient. Mobilization of the musculofascial flap of the upper eyelid. (A) Creation of subcutaneous “tunnel” under the skin of lateral canthus. (B) Carrying of the flap through the “tunnel” on the lower eyelid. (C) Placing a flap on the projection of the preseptal portion of the orbicularis muscle
The length, width, and shape of the transplanted flap corresponded to the possibilities available on the upper eyelid. The size usually does not differ from the same flap, if upper blepharoplasty was performed. The vascular pedicle of the flap was based on the lateral portion of the periorbital region. The edges of the wound were mobilized only by 2–3 mm for it to be easily deployable when transferred on to the lower eyelid, and the flap was then rotated no more than 10°–15°. All of this was usually sufficient to prevent damage. We believe that even if there was a lack of nutrition to the flap, it will not undergo necrosis and will take root in the same way as it does in a free transplant.
The aponeurosis that rose along with the muscle was significantly smaller than the flap itself, both in length and width. It was rather narrow by only a few millimeters and hence the wound edges were easily sutured with several interrupted sutures (6/0 proline).
Subsequently, a classical incision was made to perform lower blepharoplasty, followed by the mobilization of the musculofascial flap on to the arcus marginalis, which was moved downward to make a “tunnel” under the skin of the lateral canthus [Figure 1A]. The musculofascial flap was then rotated on its pedicle and passed through a subdermal tunnel, present on the wound surface of the lower lid [Figure 1B] and distributed between the pretarsal portion of the orbicularis muscle and the arcus marginalis. The flap was located above the upper edge of the orbicular muscle and compensated for the deficit by the preseptal portion. The flap was fixed in position using several nodal prolene 6/0 sutures [Figure 1C]. The musculofascial flap of the lower eyelid (posterior lamella) was then returned to its original location. The skin on the upper and lower lids was covered using intradermal PROLINE 6/0 sutures. In classical blepharoplasty, excess skin and tissue were generally removed. Here, we instead preserved the tissue to create a flap and used it to fill the emptied lower eyelid.
In cases where the flap was long and voluminous, it was easy to transfer to the tear through and it’s a medial part, and in case, when the flap was short and did not go to the medial portion, we filled the tear through with the upper eyelid fatty-tissues.
The flap was sutured with 6/0 prolene, the suture was interrupted, which was fixed in the periosteum, to the arcus marginalis in the lower part, and to the upper part it was fixed to the skin of lamella.
RESULTS
The wounds of all the patients healed without any complications, and sutures were removed on the 4th or 5th day. The patients were treated according to a classic rehabilitation scheme. In the early as well as the subsequent post-operational period, patients were referred for examination only at the beginning (in the first few cases). Special attention was paid not only to maintain the fullness of the lower eyelid but also to the condition of the upper eyelid and the function of its levator. The patients did not report any case of upper ptosis and did not have any complaints post-operation as they considered the obtained result to be good.
We do not believe that “patient satisfaction was high”; we saw that patients were satisfied with the results. Unfortunately, we did not conduct a postoperative survey of patients using questionnaires; therefore, we could not present a table.
DISCUSSION
The excision of excess intraorbital fat with the associated resection of the posterior lamella (skin and muscle) was the dominant method to correct the palpebromalar groove for more than half a century.[1] However, in the last two decades, the opinion of colleagues who carry the idea of the “preservation” operations and surgeries gained more support, which was based not on the idea of removal, but addition and strengthening to an existing component.[34567891011121314]
The clinical efficacy of the new concept to preserve became more apparent during the conduction of the first-ever lifting surgery in the midface area.[2345] In such surgeries, midface soft-tissues were lifted vertically upward and, in most cases, almost eliminated sinking into the arcus marginalis area. The advantage of these surgeries was probably due to the stretching of external tissues of the midface area, where enough fat is present and transferred to an area that lacked fat. Similarly, an excellent outcome can be obtained by low-invasive thread-based methods of midface lifting, which can be conducted simultaneously with or without lower blepharoplasty.[67] A sunken lower eyelid is usually caused by iatrogenic factors (fatty-tissue development or in aging patients who normally lose fatty-tissue elasticity and therefore its contact with each other). The decision of the surgeon lies in the method to correct the issue as well as obtain patient satisfaction. Some of them use fillers, grafts, and fat injections; however, these approaches have the risk of possible relapse or the presence of a visual frown, migration, atrophy, resorption, etc.
The advantage of using a flap is that it can fill defects that have strong tissue complexes, without any risk of damage. There is also no need to remove preserved tissues when using a flap. Moreover, there is a criterion that indicates when a surgeon should perform classical blepharoplasty, but in our case, the method was used only when the patients did not have upper blepharoplasty previously performed. This criterion provided the patients with a successful result. The correction of such deformation can be carried out efficiently by using the lipo-lifting method or with synthetic fillers.[8] However, fillers are known to behave unpredictably, and they result in lymhpostasis, migrate, or even quickly dissolve. Encapsulation of fillets leads to an unaesthetic look of the lower eyelids. They also resemble peas when touched during palpations and can be seen visually. In these cases, they cannot be solved through either a dissolving therapy or injection of hormonal preparations. Therefore, at the request of patients, they will be removed surgically.
In this article, we present a blepharoplasty method, which is substantially different from the traditional resection method. Our approach was based on the idea of replenishment of deficit by transfer of a de-epidermized musculofascial flap from the upper eyelid to the most vulnerable part of the lower eyelid (the projection of the preseptal portion), as well as strengthening of the myofascial carcass of the posterior lamella. In Figure 1C, the flap is shown to be placed precisely at the location of the weakest preseptal portion. This interposition, termed as “dam,” was performed by Bill Little by transplanting the flap from the temporal fascia, which was then sutured between the pretarsal portion and the arcus marginalis.[11]
A similar tendency to strengthen the “weakest point” can be seen in other methods for lifting the orbital portion, such as with the creation of a musculofascial duplex in place of the preseptal portion.[12131415]
In case the transferred flap is closed by the earlier exfoliated musculofascial flap from the front, a duplex of the preseptal portion can be created, which then strengthens the posterior lamella. The replaced flap can thus increase the volume of the eyelid cranially, beyond the boundary of the arcus marginalis. For example, the flap can smooth the boundary between the palpebral and orbital portions of theorbicular muscle, which is the anatomical name for the visually defined palpebromalar groove (boundary between the eyelid and cheek).[45678910111213141516]
The advantage of using the flap is that it fills defects with strong tissue complexes without any risk of damage, migration, frown, or resorption. In comparison to classical blepharoplasty, we do not remove tissues that are being preserved, which is a major advantage of using the musculofascial flap. Of the 26 patients who underwent surgery, 11 underwent only upper and lower blepharoplasty according to this method [Figures 2 and 3], nine received thread lifting of the midface through the Aptos method, and the remaining 6, combined with the classic Face Lift [Figure 4]. In 16 patients, we excised a moderate amount of excess fat from the lower lids and did not remove it in the remaining 10. In all the cases, the pathology of the “emptied” eyelid was expressed on both the right and left sides. However, in most patients, the deficit of soft-tissues can be mostly seen on only one particular side. Such defects of involutional etiology were detected in 16 patients, and the remaining 10 were iatrogenic patients. Of the 10 iatrogenic patients, eight presented after a transconjunctival blepharoplasty, while the remaining two presented following classical skin resection. Indications for this method should be cases of evident weakness in the projection of the preseptal portion of the orbicularis muscle of either a natural or iatrogenic origin. Most often in our practice, we encounter cases of eyelid-cheek boundary defects of involutional or natural origin. In some of them, the origin of such sinking has been associated with trauma, coagulation, or even resection of the preseptal portion during the course of removal of hernia protrusions, perforating, or stretching of this particular portion. Sometimes, such deformations occur due to excessive resection of fatty hernias.[13]
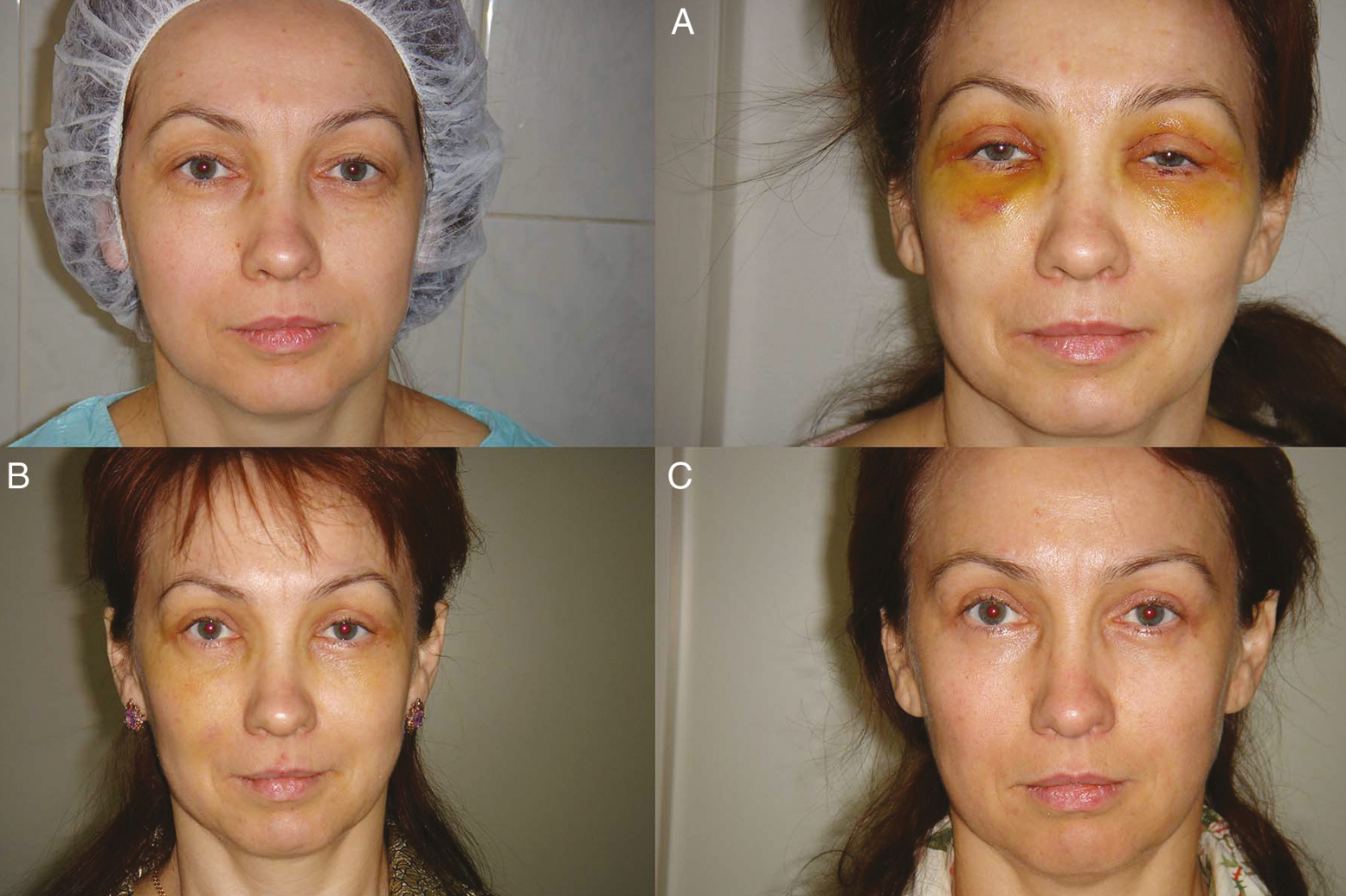
- 40-year-old patient before the operation. Patient has “emptied” eyelid with a hypertrophic of the pretarsal portion of the orbicularis muscle. This condition was the result of transconjunctival blepharoplasty. (A) Patient after the musculofascial flap transfer from the upper to the lower lid. Patient photo after the removal of sutures. (B) Condition after two months from the operation. (C) Condition after six months from the operation: The transferred flap could not fill the defect on the left eyelid since the thickness of the flap did not correspond to the defect volume
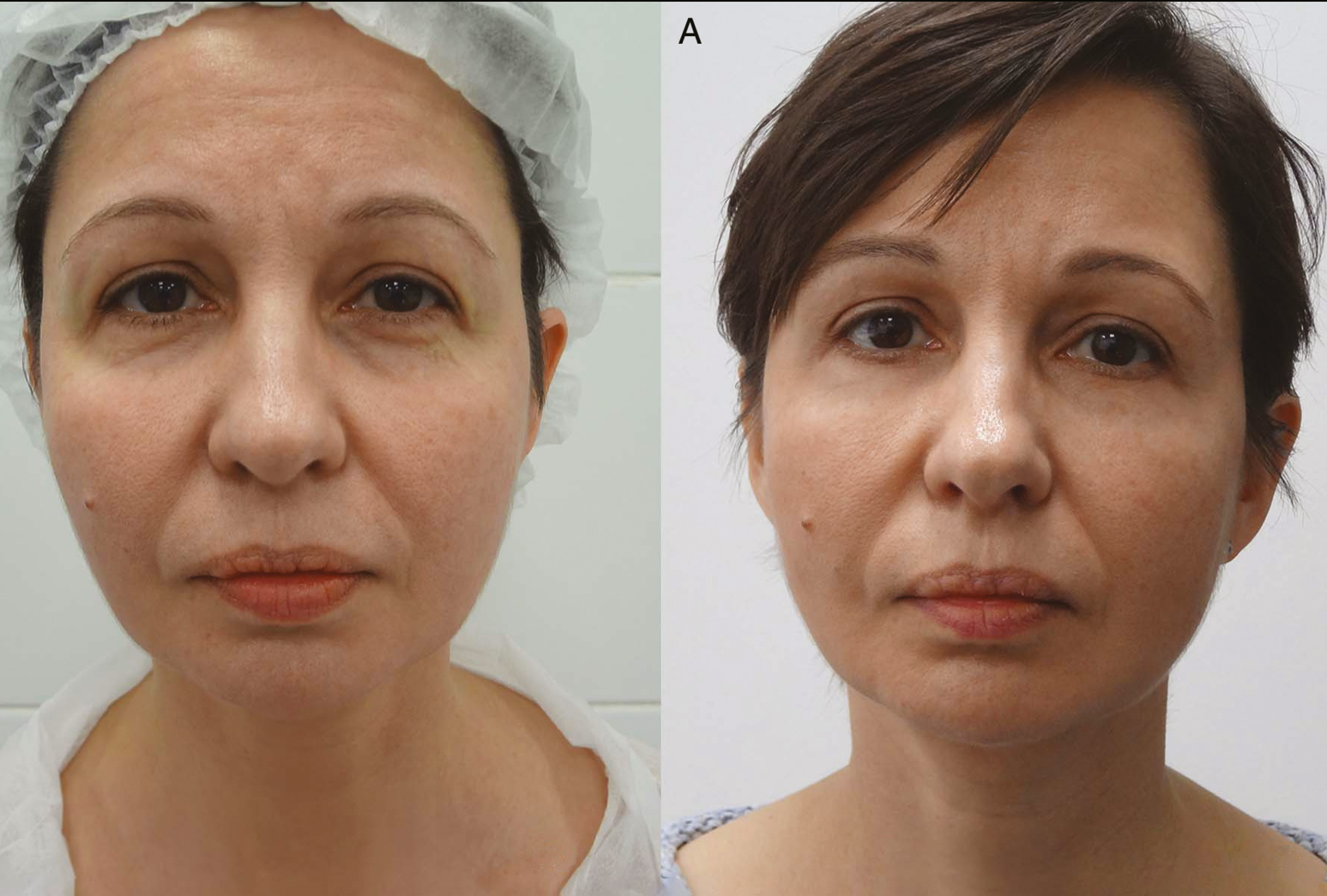
- Before the operation of a 47-year-old patient. “Emptied” eyelid and the condition after a classic lower blepharoplasty. (A) Six months postoperation with the offered technique

- Before the operation of a 59-year-old patient. Wrinkles on the face and neck, and clear “emptiness” of the lower eyelids of involutional etiology. (A) Condition 9 days after operation: SMAS (superficial musculoaponeurotic system) rhytidoplasty, upper, and lower blepharoplasty, the transfer of musculofascial flap from the upper lid to the lower one, and facial skin peeling TCA (trichloroacetic acid) 25%. (B) Seven months after the operation
Moreover, the described flap adequately compensates for a tissue deficit in the areas of the lower orbital edge, smoothing the “minus”-relief. However, in all the cases, the length of the transferred flap corresponded to the length of the defect and did not reach the medial section. In addition, in some patients, the volume and thickness of the flap were sufficient to fill the deficit of the lower eyelid tissues by height and depth [Figure 2 and C]. In such cases, we filled the missing area with fatty lumps (hernias) from the upper eyelid.
CONCLUSION
The transfer of the musculofascial flap from the upper to the lower eyelid should be considered as a useful method in cases of tissue deficit in the arcus marginalis area, which anatomically corresponds to the weakened preseptal portion of the orbicularis muscle. However, this method applies only to patients who have not undergone upper blepharoplasty previously and in whom the orbicularis muscle has been preserved. The success of the method relies on prior indications for an esthetic outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Not applicable.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Blepharoplasty for herniated intraorbital fat: Anatomical basis for a new approach. Plast Reconstr Surg (1946). 1951;8:46-58.
- [Google Scholar]
- Fat pad sliding and fat grafting for leveling lid depressions. Clin Plast Surg. 1981;8:757-76.
- [Google Scholar]
- Arcus marginalis release and orbital fat preservation in midface rejuvenation. Plast Reconstr Surg. 1995;96:354-62.
- [Google Scholar]
- Evolution of technique of the direct transblepharoplasty approach for the correction of lower lid and midfacial aging: Maximizing results and minimizing complications in a 5-year experience. Plast Reconstr Surg. 2000;105:393-406; discussion 407-8.
- [Google Scholar]
- Elimination of aesthetic deformations of the midface area our experience. Aesthetic Plast Surg. 2018;42:774-90.
- [Google Scholar]
- Lifting of soft tissues: Old philosophy, new approach – A method of internal stitching (Aptos needle) J Japan Soc Aesthet Surg. 2005;42:182.
- [Google Scholar]
- Correction of rhinolacrimal groove. The International Congress of plastic, reconstructive and aesthetic surgery, Yerevan. Med J Erebuni. 2009;39:19-20.
- [Google Scholar]
- Correction method for an “emptied” lower eyelid. J Plast Surg Cosmetol. 2010;1:1-160.
- [Google Scholar]
- Comment to the article of M. Sulamanidze et al. “Correction method for “emptied” lower eyelid. J Plast Surg Cosmetol. 2010;1:1-160.
- [Google Scholar]
- Volumetric perceptions in midfacial aging with altered priorities for rejuvenation: Three-dimensional rejuvenation of the midface: Volumetric resculpture by malar imbrication. Plast Reconstr Surg. 2000;105:286-9.
- [Google Scholar]
- Combined arcus marginalis release, preseptal orbicularis muscle sling, and SOOF plication for midfacial rejuvenation. Aesthet Med. 2006;V:495-501.
- [Google Scholar]
- What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg. 2005;115:1395-402; discussion 1403-4.
- [Google Scholar]
- Elimination of rhinolacrimal groove using the method of bringind down of orbital septum on the lower edge the orbit. Aesthet Med. 2006;V:321-29.
- [Google Scholar]
- The “round” eye problem. Our approach. 2009. Vienna: 30th Annual Meeting of the International Society for Dermatologic Surgery (ISDS); Available from: https://www.isdsworld.com/wp-content/uploads/2017/04/envoy_v_2009.pdf
- [Google Scholar]
- Fat preservation technique of lower-lid blepharoplasty. Aesthet Surg J. 2001;21:450-9.
- [Google Scholar]






