Translate this page into:
“Something Better Than Nothing” Using the House Hold Electric Chimney in the Procedure Room as an Attempt to Reduce the Smell and Biohazard
Address for correspondence: Dr. K. T. Ashique, Karalikkattil House, Karakkaparamba, P. O. Vaniyambalam, Malappuram Dt.-679 339, Kerala, India. E-mail: drashique@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Laser and radiofrequency (RF)-based procedures are very commonly done in many dermatology centres. Surgical smoke and plume generated from these procedures (especially ablative RF procedures) is an often neglected part of the standard operating procedures. The need for adequate health protection for the operating personnel, their assistants and the patient, apart from the need for a smell-free environment is important, especially in small centres and private clinics where space is a constraint.
The commercially available smoke evacuators are usually used in conjunction with ablative LASERs. These are costly devices, priced anywhere between 50000 and 1 Lakh INR (approx. 1000–2000 USD) making it an additional burden for the small-time dermatologist who is more into RF-based procedures.
Wearing a surgical mask alone does not give protection from diseases and health hazards associated with surgical smoke.[1] Basically there are two issues to be addressed with regard to the surgical plume and the dermatologist: Occupational hazards to the personnel on inhalation of surgical plume and the need to reduce the unpleasant smell produced in the process of charring live tissue using instruments like the Radio Frequency (RF) unit. The dermato-surgery procedures generally being of lesser duration, there is a comparatively less, yet very real risk of occupational hazard. The unpleasant smell is a major issue after any RF surgery or laser procedure in the operation room and may last for almost a day, especially in a poorly ventilated room. The ideal smoke evacuator should have characteristics such as ease of use, foot pedal activation/automatic on-off, portability, efficiency and should also be quiet and cost-effective. Most newer portable smoke evacuators have a triple filtration method — a pre-filter for capturing large particles, a second filter for capturing smaller particles and a third filter like a charcoal filter for capturing odors and other gases. Smoke evacuators also have consumables involved and filter needs to be replaced from time to time and are very expensive. Most good LASER centres use portable smoke evacuators with most of the previously mentioned characteristics. However, these portable smoke evacuators tend to be costly and might be difficult to procure for smaller establishments.
Here we present an attempt to use the conventional electric-operated kitchen chimney(Butterflame™) commercially available for less than 10K INR — approx. 200 USD) [Figure 1], as an arguably better alternative than doing the procedures without any smoke evacuator in place and a sure help to reduce the obnoxious smell in the operating room.

- Commercially available kitchen chimney fitted right above the operation table about half a meter away from the patient
DESCRIPTION OF THE APPARATUS
The electric chimney is a ready made small-sized kitchen cabinet placed at head level of the surgeon fixed to the wall adjacent to the operating table. It has an inbuilt motor which can suck air at a pressure of 6Pa and has a filtering wire mesh facing downwards. The air sucked is propelled upwards by the same motor and sent out through the outlet connected to the roof of the apparatus. [Figure 2]
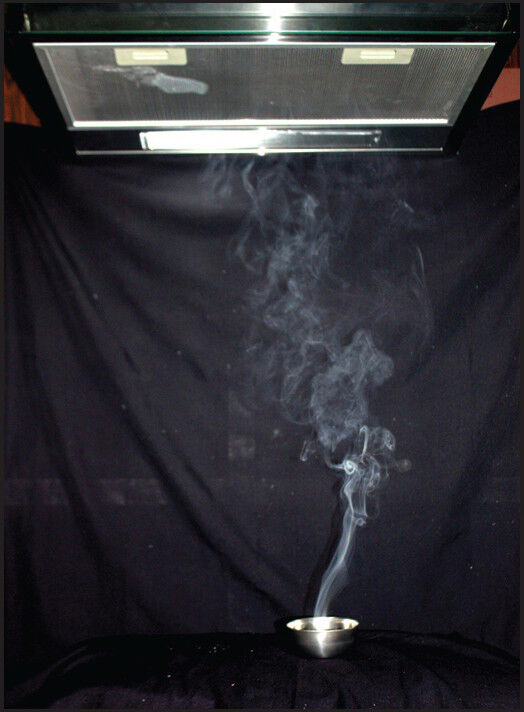
- Artificial smoke produced with camphor to show the flow of smoke when the suction is at work
The limitation of the system is the need to keep the apparatus fixed to the wall or the operating table and the practical difficulty in moving the patient who may have a procedure on the face and the leg simultaneously.
The outlet opens to the outside environment and hence the harmful effects and the smell are almost negligible [Figure 3]. Fixing an air conditioner filter at the outlet or placing some activated charcoal in the outlet pipe (as an adsorbent)are additional steps that can be employed to decrease the hazards of the sucked smoke.
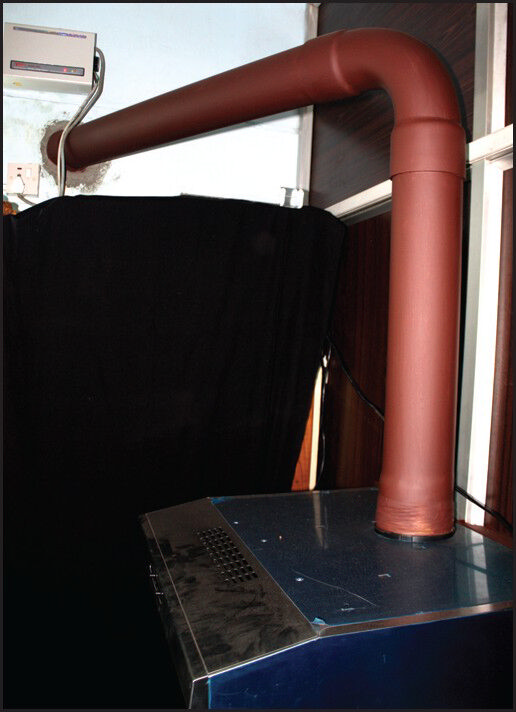
- The outlet of the smoke evacuator (chimney) routed out of the operating room through the overhead outlet
We have been using the electric chimney in a busy dermato surgery theatre for the last 1 and half years and have found a subjective yet very significant and perceptible difference in the smell especially associated with RF procedures. We conducted studies with healthy volunteers (professional colleagues) who could very well appreciate considerable difference in the offensive smell in the operating room with the apparatus on and off while RF cautery of warts were undertaken. Surgical smoke is produced by the thermal destruction of tissue. Chemical analysis has shown its constituents to be mainly (approximately 95%) water vapour, with the remaining containing chemicals and cellular debris.[2]
Electrocautery and ablative RF/lasers heat the target cells producing surgical smoke when the target cells reach a point of boiling which in turn leads to membrane rupture and dispersal of cellular contents and fine particles.[3]
Surgical plume may contain toxic components such as acrylamide, acetaldehyde, formaldehyde and benzene. Composition and toxicity varies according to the applied technique, energy and processed tissue. High temperature induces more toxic aerosols.[4] Acrylonitrile, which is a pungent- smelling colourless liquid that forms hydrogen cyanide is classified as class 2A carcinogen to humans and is absorbed through the skin and lungs.[5] Mutagenicity and pulmonary effects of the surgical smoke inhalation have also been documented in various reports.[6]
Studies have shown that awareness about the health hazards of surgical smoke is very minimal among the surgeons as evident in a questionnaire base survey across 14 hospitals in the UK. The protection taken was also negligible as evident in the fact that only 3 of 98 surgeons used dedicated smoke extractors. Due to the more widespread use, greater smoke production and the charring effect, electrosurgery unit smoke may be more harmful.[7]
Most commercial surgical smoke evacuation systems are basically high-flow suction and filtering devices used to remove, the smoke generated at the surgical site during the use of lasers and electrosurgical units. This process helps to minimise patient and staff exposure to the aerosols and gases carried by the smoke. Alternatives include local exhaust ventilation and room suction units, but these are not considered as effective as dedicated smoke evacuators. Smoke evacuators contain a suction unit (vacuum pump) as the centre of the unit and have a filter, hose and an inlet nozzle. A capture velocity of about 100-150 feet per minute at the inlet nozzle is generally recommended and a high efficiency particulate air (HEPA) filter or equivalent is recommended for trapping particulates.[8] Various filtering and cleaning processes also exist which remove or inactivate airborne gases and vapors. The various filters and absorbers used in smoke evacuators require monitoring and replacement on a regular basis and are considered a possible biohazard requiring proper disposal. The commercial smoke evacuators inlet nozzles should be kept within 2 inches of the surgical site for best efficiency and the device must be switched ON throughout the procedure. All tubing and steriliseable material must be either disposed or sterilised as needed. The disadvantages of this system include the fact that one of the assistants must be holding the inlet hose nozzle throughout the procedure and also the post-usesterilisation process must be strictly adhered to. The use of a stationary electric chimney does not require any help from the assistant and neither does it need extensive post-use sterilisation procedures.[9]
When the device is installed in a laser clinic, there are chances for light being reflected from the reflecting surfaces. However, this can be overcome by applying matte finish paint or sticking a non-reflecting tape over the glistening areas especially those that fall in the route of the laser light.
LIMITATIONS AND CONCLUSIONS
This can be a good and effective addition if not a complete alternative to smoke evacuators for smaller centres where cost of investments and space constraints are a major issue. Being a fixed device, the electric chimney has a definite disadvantage with regard to portability and the patients position has to be adjusted according to where the device is fixed. This device, will not replace a smoke evacuator but would at least help to bring down the obnoxious smell and some amount of biohazard compared to doing the procedure with nothing in place.
We advocate more studies to analyse the efficacy of this device, in decreasing the disease transmissibility of the smoke and the smell of plume. More comparative studies with the commercially available smoke evacuators are also recommended to come to a final and effective conclusion. Various methods like the use of a domestic vacuum cleaner or connecting a funnel tipped tube to the tip the hospital wall suction connected to the central suction line after incorporating appropriate filters are also worth exploring as cheaper alternatives.
ACKNOWLEDGEMENTS
We would like to acknowledge the help provided by the Hospital Management, Staff (Purchase and maintenance departments), Alshifa Hospital, Perinthalmanna, Kerala for helping us in executing the plan.
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- Aerosol penetration and leakage of masks used in the health care industry. Am J Infect Control. 1993;21:167-73.
- [Google Scholar]
- Infectious papillomavirus in the vapour of warts treated with carbon dioxide laser or electrocoagulation: Detection and protection. J Am AcadDermatol. 1989;21:41-9.
- [Google Scholar]
- Chemical composition of surgical smoke produced by electrocautery, harmonic scalpel and argon beaming – a short study. Eur Surg. 2007;39:118-21.
- [Google Scholar]
- International Agency for research on Cancer (ARC). Monograph: Overall evaluation of carcinogenicity to humans. 2008. Available from: URL http://www.monographs.iarc.fr/ENG?Classification/crthall.php
- [Google Scholar]
- Current attitudes and practices towards diathermy smoke. Ann R Coll Surg Engl. 2007;89:162-5.
- [Google Scholar]
- Control of Smoke From Laser/Electric Surgical Procedures. [Internet] Available from: http://www.cdc.gov/niosh/docs/hazardcontrol/hc11.html
- [Google Scholar]





