Translate this page into:
Split-face Comparative Study of Efficacy of Platelet-rich Plasma Combined with Microneedling versus Microneedling alone in Treatment of Post-acne Scars
Address for correspondence: Dr. Sowmya C. S., Department of Dermatology, Venereology and Leprosy, Kempegowda Institute of Medical Sciences Hospital and Research Centre, K. R. Road, Parvathipuram, Vishweshwarapura, Basavanagudi, Bengaluru 560004, Karnataka, India. E-mail: sowmya.cs17@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Context:
Skin conditions contribute substantial burden toward global morbidity and mortality. Acne vulgaris, with its rising prevalence, has become a cause of concern among researchers as well as dermatologists due to scarring.
Aims:
The aim of this study was to compare the efficacy of microneedling alone versus microneedling combined with platelet-rich plasma (PRP) in post-acne scars using a split-face method.
Materials and Methods:
Thirty patients with atrophic post-acne facial scars were offered four sittings of treatment monthly once. As a standard protocol, the right side of the face was subjected to microneedling with PRP (Group A) and the left side of the face with microneedling alone (Group B). Objective evaluation of improvement was performed by the physician recording the acne scar assessment score at baseline and thereafter at every visit using Goodman and Baron scale. Alongside patients also graded the improvement in acne scars at the end of the study.
Statistical Analysis Used:
The collected information was entered in MS Excel (Bellevue, WA, USA) and analyzed using appropriate statistical methods with Statistical Package for the Social Sciences software (IBM Corp., Armonk, NY). The significance of the outcomes of the study was assessed by calculating the P value and the value of P < 0.05 was considered statistically significant.
Results:
The mean age of patients was 25 years. Thirteen (43%) patients in Group A had an excellent response as compared to 6 (20%) patients in Group B according to physician assessment. Patient’s satisfaction was more in Group A as compared to Group B as 11 (36%) patients had more than 75% improvement in Group A as compared to 1 (3%) patient in Group B.
Conclusion:
The study showed a decrease in scar severity grade in all the patients enrolled for treatment. However, the combined use of microneedling and PRP was found to be more effective than a single method used for treatment of acne scars.
Keywords
Acne
microneedling
PRP
split-face method
treatment
Microneedling is a simple method of treatment for reducing scars, having little downtime and satisfactory results, and its combined use with PRP increases its effectiveness.

INTRODUCTION
Acne associated with great psychosocial stress is a disease of pilosebaceous gland associated with papules, comedones, pustules, and cysts. Primary request of patients with acne is clearance of scars.[1] Although it is considered a normal phase in the life course of a human being, this condition has been found to be associated with a greater psychological burden than a variety of other disparate chronic disorders.[2]
With advances in medicine and availability of innovative technologies, diverse treatment strategies such as chemical peeling, dermabrasion, laser treatment, punch techniques, fat transplantation, other tissue augmenting agents, needling, subcision, and combined therapy have been tested and recommended for treatment.[3] However, considering the complex multifactorial nature of acne wherein endocrine, environmental as well as dietary factors[456] play their role, the satisfactory treatment results are not achievable with a single set of treatment. Moreover, limited efficacy, poor satisfaction of patients, and side effects of techniques warrant exploration of newer techniques or trials of diverse combinations of different techniques to overcome the challenges. One novel modality of treatment is microneedling therapy (also known as collagen induction therapy).[7] However, results vary from patient to patient and also with different combinations of microneedling. Although various studies regarding efficacy of microneedling alone or in combination with platelet-rich plasma (PRP) in acne scars have been undertaken, this study was undertaken for the efficacy of microneedling alone versus microneedling combined with PRP in post-acne scars using split-face method.
Thirty patients with atrophic post-acne facial scars, who attended the cosmetology outpatient department in Kempegowda Institute of Medical Sciences from April to October 2018, were offered four sittings of treatment with 1-month interval between each session. The patients were followed up for 6 months posttreatment.
INCLUSION CRITERIA
All patients aged 20–40 years presenting with Fitzpatrick skin types II–IV were included in the study as patients with Fitzpatrick skin type I were rare to find at our hospital setup, and skin types I–III have minimal risk of pigmentary complications with resurfacing procedures. In patients with Fitzpatrick skin types IV–VI, the risk of pigmentary change is higher with the deeper wounding. In addition, assessment of scars was made using Goodman and Baron scale [Table 1]. Acne scars of Grades II, III, and IV were included to be part of the study.
| Level of Diease | Charecteristics | Examples |
|---|---|---|
| macular disease | erythematous, hyper- or hypopigmented flat marks visible to patient or observer irrespective of distance | erythematous hyper or hypopigmented flat marks |
| mild disease | mild atrophy or hypertrophy that may not be obvious at social distance of 50 cm or greater and may be covered adequately by makeup or the normal shadow of shaved beard hair in males or normal body hair if extrafacial | mild rolling, small soft papular |
| moderate disease | moderate atrophic or hypertrophic scar that is obvious at social distance of 50 cm or greater and is not covered easily by makeup or the normal shadow of shaved beard hair but is still able to be flattened by manual stretching of the skin | more significant rolling, shalloe “boxscar”, mild to moderate hypertrophic or opular scars |
| severe disease | severe atrophic or hypertrophic scar that is obvious at social distance of 50 cm or greater and is not covered easily by makeup or the normal shadow of shaved beard hair in males or body hair (if extrafacial) and is not able to be flattened by manual stretching of the skin | punched out atrophic (deep “boxscar”), “icepick”, bridges and tunnels, gross atrophy, dystrophic scars significant hypertrophy or keloid |
EXCLUSION CRITERIA
We included patients with atrophic scars only; thus, patients with active acne lesions were excluded. In addition, patients with keloid scarring or keloidal tendency, history of bleeding disorder and anticoagulant therapy, oral steroid therapy, active skin infection such as warts and herpes, and bacterial infection were also excluded from the study because of the nature of lesions or concomitant complications due to these conditions. Pregnancy and lactation were also considered as exclusion criteria.
Once grading of the acne scars was carried out for both sides of face using Goodman and Baron scale, patients were explained about the treatment offered along with potential implications of treatment in terms of expected results, duration of treatment, follow-ups, side effects to be reported, and prognosis of treatment.
In addition, the patients with acne included in the study were thoroughly evaluated. Complete blood counts were undertaken. Digital photographs of both sides of face were taken by taking written informed consent from patients. Topical anesthetic cream eutectic mixture of local anesthetic was applied 30–45 min before the procedure to anesthetize the area. The list of side effects reported during the course of treatment was maintained. After procedure, antibiotic medication for 2–3 days, sun protection, and regular usage of sunscreens were advised.
PRP was prepared under strict aseptic conditions by drawing 6-mL blood in one vial having 1.5-mL Anticoagulant Citrate Dextrose (ACD) in 8.5-mL BD Vacutainer (BD Company, Bangalore, India) glass blood collection tubes. ACD vials were used to inhibit platelet aggregation. It was then centrifuged for 15 min at 3600 rotations per minute. The whole process was carried out under strict aseptic conditions as well as optimum temperature regulations, that is, 20–22°C. Microneedles with 1.5 mm length and 192 needles on roller drum were used. Pre- and post-procedure, platelet count was measured and found to be 1.5–2 lakhs and 4–5 lakhs, respectively.
As a standard protocol, the right side of the face was subjected to microneedling with PRP and the left side of the face with microneedling alone. The skin was stretched and microneedling was carried out in vertical, horizontal, and both diagonal directions for about 4–5 times following which PRP was applied and also injected intradermally on the right side only. Icepacks were applied over the treated areas.
Prior to visit completion, all patients were instructed to follow strict photo-protective measures. All the patients were reviewed after 1 week for any side effects and advised next sitting at completion of 1 month. Similar protocols were followed at each visit. At the end of four treatments, the scars were regraded. Photographs were retaken with as much similarity in background, positioning of face, and lighting for after treatment comparisons with the pretreatment images. In addition to grading by physician, patient’s assessment of improvement was also recorded for all patients.
The observed and patient-reported baseline and end line information was entered in MS Excel (Bellevue, WA, USA) and analyzed using appropriate statistical methods with Statistical Package for the Social Sciences software (IBM Corp., Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp.). The significance of the key outcomes of the study was assessed by calculating the P value, and the value of P < 0.05 was considered statistically significant. Physician’s assessment was classified as excellent, good, and poor. The improvement was rated as poor, good, and excellent depending on the change in grade of acne scars by both treating physician and the patient. An improvement by two grades was considered as excellent. Grade I was rated as good and no upgradation on assessment was labeled as poor response. Patients’ perceptions of improvement were noted by using the visual analogue scale, where the patient was asked to mark on the line the point that they feel represents their perception of their current state. Overall, differences in final grading by physician and patient’s perceptions were analyzed to report percentage matching as successful result of treatment.
RESULTS
All the enrolled 30 patients completed the procedure, that is, four visits at a gap of 1 month each. Patients belonged to the age group of 19–35 years with mean age of 25 years. About 60% of the patients were men. All the patients were given sittings according to their basic scar types. Details of different scar combinations of patients treated under the study are presented in Figure 1. About 60% of the patients belonged to scar type 3, that is, box and rolling scar. This was followed by 13% of the patients with ice pick and box scar. Average time per sitting for the procedure was approximately 30 min.
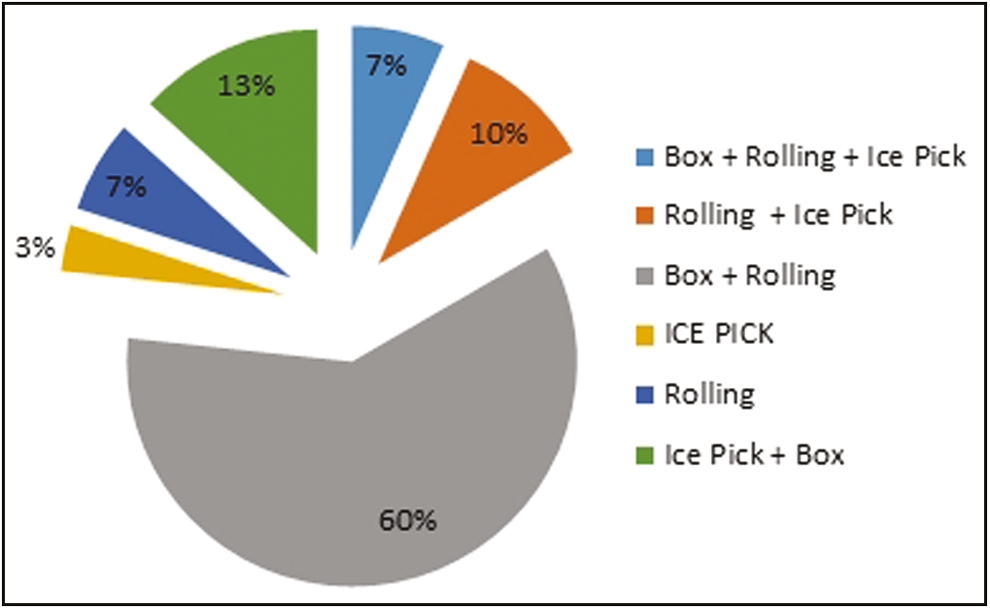
- Scar type
Overall, 24 patients (80%) achieved a reduction in scar level on either side of face. However, as our objective was to compare the reduction in level of scar using two different techniques, we compared the percentage cases achieving reduction on different sides. Reduction in scar level was observed in 22 patients on the left side of the face (73%), that is, on the side treated using microneedling alone. In comparison, the right-side scars were observed to be reduced in 28 patients (93%).
Reduction in scar levels was found to be present for all scar types and on both sides of face. It was found that the percentage reduction in scar level was highest for mixed scar types. For box and rolling scar (the most common scar type among patients), reduction was observed in 78% of patients [Table 2]. The difference in number of patients observed to be having reduced scar levels in different scar types was, however, statistically nonsignificant, thus highlighting the applicability of this procedure for all types of scars.
| No of patients (a) | Number observed to be having reduced scar level (b) | Percentage scar reduction by scar type (b*100/a) |
|---|---|---|
| 2 | 2 | 100 |
| 3 | 3 | 100 |
| 18 | 14 | 78 |
| 1 | 1 | 100 |
| 2 | 1 | 50 |
| 4 | 3 | 75 |
In addition, improvements in scar levels were found to be independent of age, gender, or scar severity of patients. Mean decrease of one point was observed among the patients at the end of treatment. Recoding of physician’s assessment of improvement revealed excellent improvement, that is, a decrease of scar by two levels on right side in 43% of patients (i.e., the side using microneedling and PRP). The decrease by just one level was found on left side of 67% of patients [Figure 2].
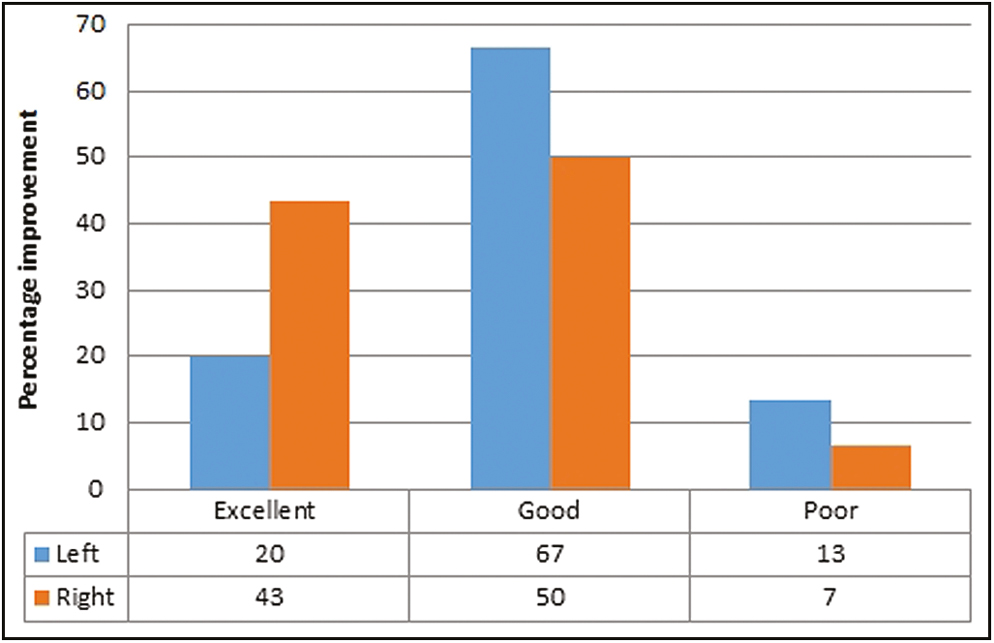
- Percentage improvement by physician’s assessment of scar
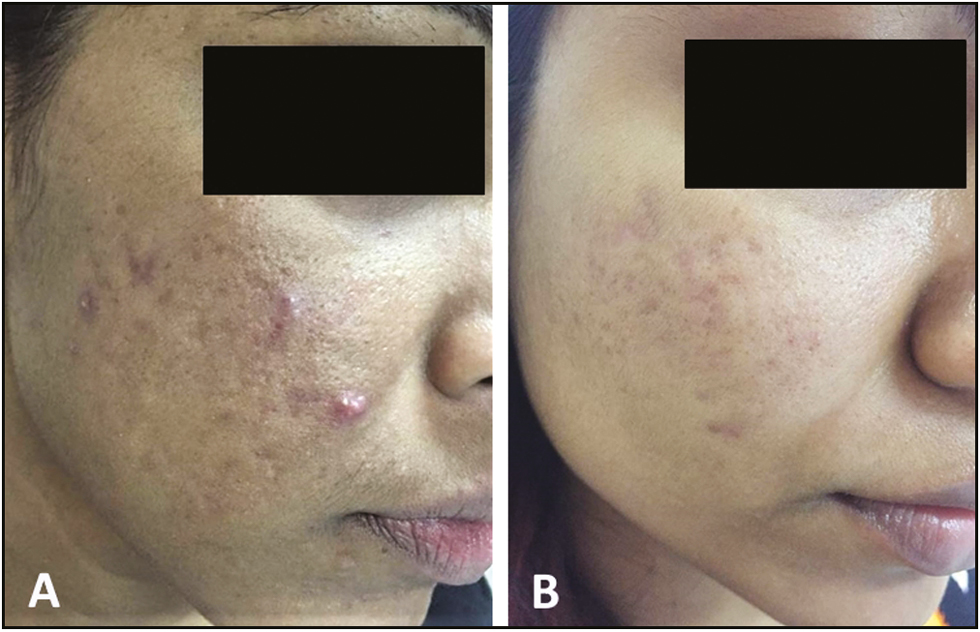
About 57% of the patients reported a decrease of 25%–50%, which was given a score of 2. More than 75% improvement was reported by only 3% of the patients for the left-side lesions as compared to 37% for the right-side lesions [Table 3]. Patients’ assessment was found to be matching the physician’s observed improvement in 27% of the cases for the right-side lesions followed by 17% cases for the left-side lesions [Figures 3-8].
| Patient Assessment | Left n (%) | Right n (%) | |
|---|---|---|---|
| Assessment | Score | ||
| 0–25 | 1 | 8 (27) | 3 (10) |
| 26–50 | 2 | 17 (57) | 6 (20) |
| 51–75 | 3 | 4 (13) | 10 (33) |
| >75 | 4 | 1 (3) | 11 (37) |
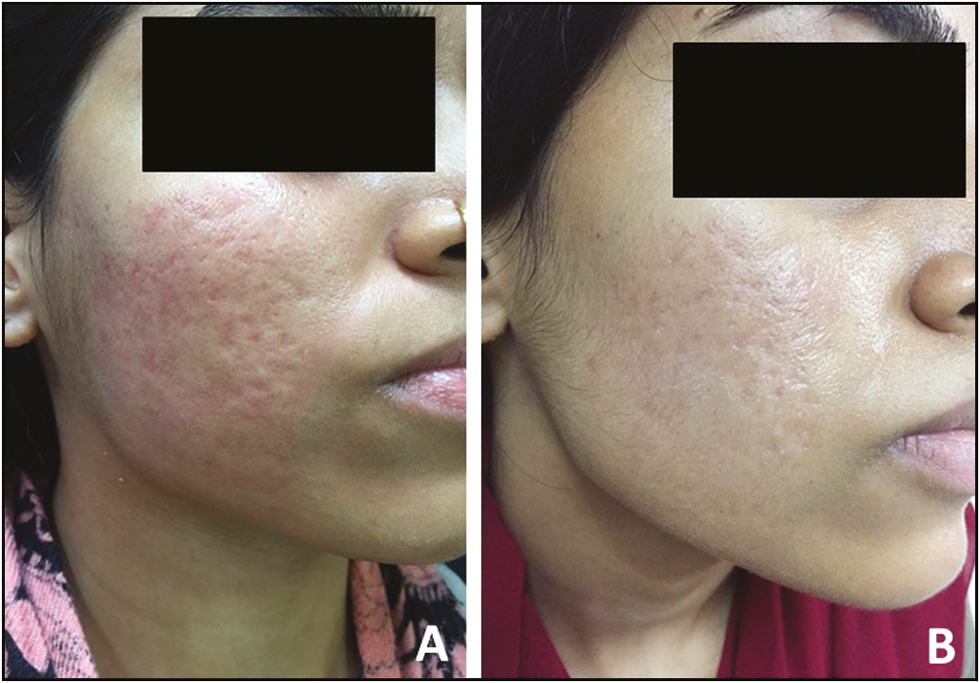
- Pre- and posttreatment with four sessions (A and B) of microneedling combined with PRP
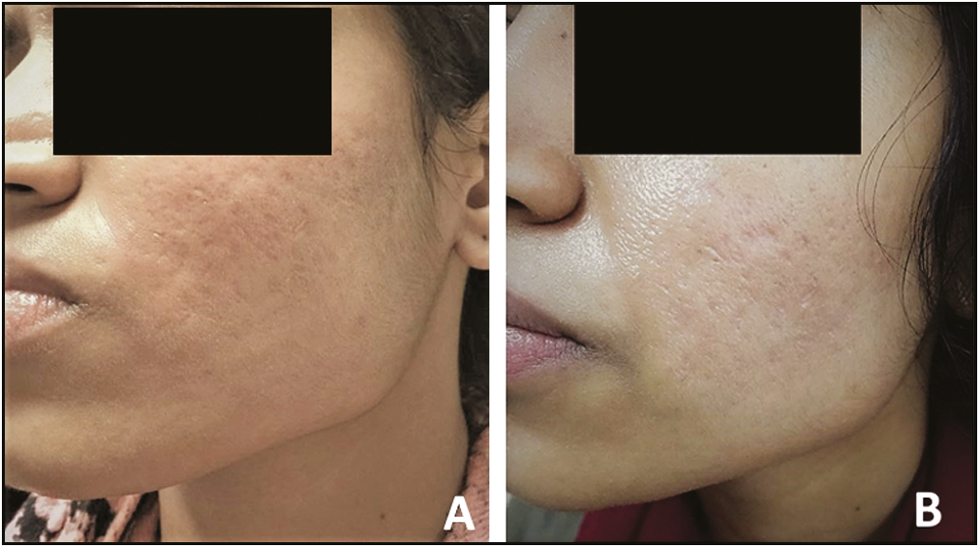
- Pre- and posttreatment with four sessions (A and B) of microneedling
- Pre- and posttreatment with four sessions (A and B) of microneedling combined with PRP
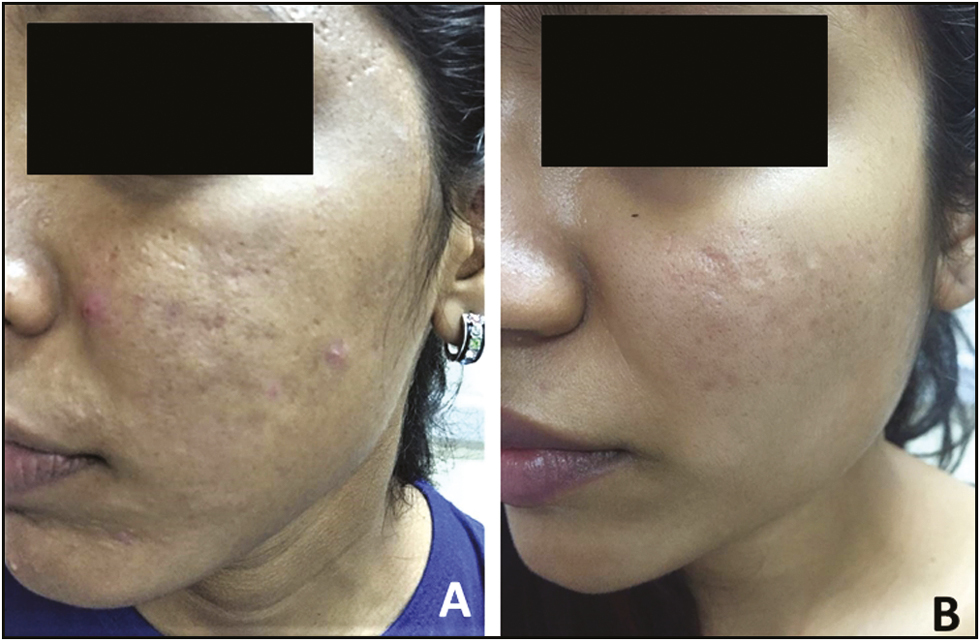
- Pre- and posttreatment with four sessions (A and B) of microneedling

- Pre- and posttreatment with four sessions (A and B) of microneedling combined with PRP
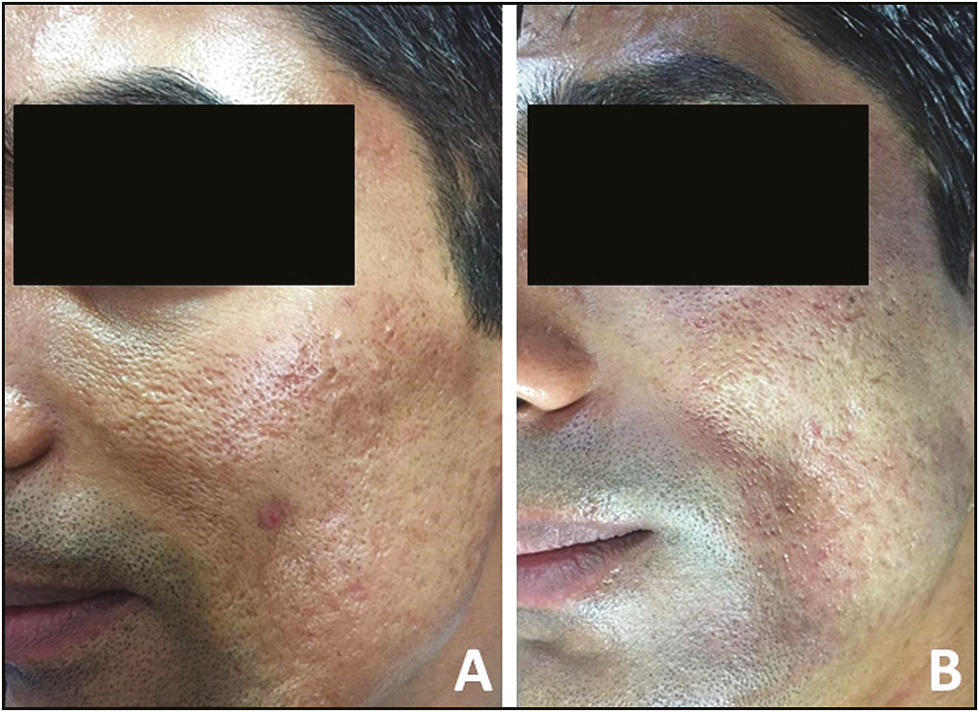
- Pre- and posttreatment with four sessions (A and B) of microneedling
DISCUSSION
Microneedling is a process involving repetitive skin puncturing using sterilized microneedles originated in 1995.[8] Since then it has been used in clinical practice as well as subjected to research all over the world.[91011] Several combinations of the procedure have been practiced worldwide.[10121314] Results, however, differ between different population primarily due to difference in skin types as well as pattern of acne scarring.[1315]
In this study, we have reported improvement in scars because of acne in a South Indian population using a simple, low-cost procedure along with its variation. The study population was similar to as reported in the recent literature, that is, young adults.[12] Patients showed improvement as per with those reported by other researchers for similar techniques, thus making it a feasible intervention for acne scars.[161718] A study by Dogra et al. also reported the procedure as being well tolerated by most of the patients.[14] They reported post-inflammatory hyperpigmentation (PIH) and tram track scarring as chief complaints. None of our patients reported the same. Ibrahim et al.[14] also reported that both microneedling and microneedling combined with PRP show satisfactory results with beneficial effects of microneedling with PRP for tough scar types.
Considering the multifactorial nature and diverse presentation of acne, the improvement after the procedure was studied by types of scars. All scar types were found to be improved by use of microneedling irrespective of use of PRP. The excellent improvement, that is, improvement by two grades was, however, more for microneedling used along with PRP. Other researchers in similar populations have also reported similar findings [Figures 3, 5, and 7],[1219] although many of them also reported the difference to be nonsignificant as in our study.[14]
Despite patient-to-patient tailoring as per scar type, the assessment of improvement in scar by patient was low as compared to clinical observation by researchers. Few other researchers had the similar experience.[1218] Gadkari and Nayak[17] reported higher average perceived improvement by subjects as compared to clinically observed improvement. The lack of satisfaction can be explored in terms of age group of patients who are young and are biased toward their assessment of improvement as their ultimate goal is a flawless radiant skin. The physician’s assessment should be reliable considering the use of standard scales for assessing change in scar levels. The risk of bias at physician level can be reduced by double-blind assessments by equally trained physicians so that the difference in perception levels does not affect the study outcomes.
Because of logistics constraints, we had to limit the sample size of study to 30 patients, thus making it difficult to study the differences by age or sex. However, studies with similar sample sizes conducted across the globe have shown effectiveness of use of microneedling along with PRP.[12161718,20] We have tried to adhere the recommended protocols of conducting the procedure, thus facilitating pooling of results by reviewers in future. This has widened the scope of using the research further to assess effectiveness of microneedling in treatment of acne scars. Further studies can be planned with higher sample size to see the determinants affecting the improvement in scar.
A systematic review by Abdel Hay et al.[3] reported low-cost, shorter recovery period, and low risk for PIH as factors contributing toward success of microneedling method.[2] In our study, adherence to procedure by all the patients was also found to be good and that also reflects indirectly on the positive patient experience with the technique used. Microneedling treatment was reported as well-tolerated acne interventions by most people because of minimal pain and lower side effects.[2122]
This study is an addition to recent emerging field of research of exploration of effectiveness of use of microneedling among different populations.[1823] A clinical trial by Dogra et al.[18] evaluated the utility of microneedling for treating atrophic acne scars in Asian populations. They found that patients’ assessments of their scars decreased from 11.7 to 6.5, indicating significant improvement.
As in our study, researchers have attempted different combinations of treatment procedures to suit patient requirement as per skin and scar type. In a study by Fabbrocini et al.,[24] the combined use of skin needling and PRP was found to be more effective in improving scar lesions than skin needling alone. In this study, we also found a combination method to be effective most effective. In an another study with patients of darker pigmented skin, microneedling was combined with glycolic acid peels for the treatment of acne scars. There was a significant improvement in skin texture and scarring in the group treated with the combined approach as compared to microneedling alone.[25]
CONCLUSION
The study showed a decrease in scar severity grade in all the patients enrolled for treatment. Scars were reduced on both sides of face with more decrease reported for the right side. Our study showed that the combined use of microneedling and PRP is more effective than single method used for the treatment of acne scars; however, there is need to strengthen the evidence with larger studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Standard guidelines of care for acne surgery. Indian J Dermatol Venereol Leprol. 2008;74:28-36.
- [Google Scholar]
- Psychosocial impact of acne vulgaris: evaluating the evidence. Skin Therapy Lett. 2004;9:1-3, 9.
- [Google Scholar]
- Hormonal and dietary factors in acne vulgaris versus controls. Dermatoendocrinol. 2018;10:e1442160.
- [Google Scholar]
- The influence of genetics and environmental factors in the pathogenesis of acne: a twin study of acne in women. J Invest Dermatol. 2002;119:1317-22.
- [Google Scholar]
- Chemical environmental factors: Can they affect acne? Indian J Dermatol Venereol Leprol. 2017;83:522-4.
- [Google Scholar]
- Microneedling therapy for atrophic acne scars: an objective evaluation. J Clin Aesthet Dermatol. 2015;8:36-42.
- [Google Scholar]
- Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543-9.
- [Google Scholar]
- Review of applications of microneedling in dermatology. Clin Cosmet Investig Dermatol. 2017;10:289-98.
- [Google Scholar]
- Microneedling: Where do we stand now? A systematic review of the literature. J Plast Reconstr Aesthet Surg. 2018;71:1-14.
- [Google Scholar]
- Split face comparative study of microneedling with PRP versus microneedling with vitamin C in treating atrophic post acne scars. J Cutan Aesthet Surg. 2014;7:209-12.
- [Google Scholar]
- Microneedling therapy with and without platelet-rich plasma. Cutis. 2017;99:239-42.
- [Google Scholar]
- Skin microneedling plus platelet-rich plasma versus skin microneedling alone in the treatment of atrophic post acne scars: a split face comparative study. J Dermatolog Treat. 2018;29:281-6.
- [Google Scholar]
- Microneedling in skin of color: a review of uses and efficacy. J Am Acad Dermatol. 2016;74:348-55.
- [Google Scholar]
- Microneedling therapy in atrophic facial scars: an objective assessment. J Cutan Aesthet Surg. 2009;2:26-30.
- [Google Scholar]
- A split-face comparative study to evaluate efficacy of combined subcision and dermaroller against combined subcision and cryoroller in treatment of acne scars. J Cosmet Dermatol. 2014;13:38-43.
- [Google Scholar]
- Microneedling for acne scars in Asian skin type: an effective low cost treatment modality. J Cosmet Dermatol. 2014;13:180-7.
- [Google Scholar]
- Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol. 2016;15:434-43.
- [Google Scholar]
- Topical vitamin C: a useful agent for treating photoaging and other dermatologic conditions. Dermatol Surg. 2005;31:814-7; discussion 818.
- [Google Scholar]
- Efficacy of a needling device for the treatment of acne scars: a randomized clinical trial. JAMA Dermatol. 2014;150:844-9.
- [Google Scholar]
- Skin microneedling for acne scars associated with pigmentation in patients with dark skin. J Cosmet Dermatol. 2018;17:390-5.
- [Google Scholar]
- Combined use of skin needling and platelet-rich plasma in acne scarring treatment. Cosmetic Dermatol. 2011;24:177-83.
- [Google Scholar]
- Combination of microneedling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol. 2011;10:317-23.
- [Google Scholar]





