Translate this page into:
Split-thickness Skin Graft Harvest under Local Anesthetic: A Single Pass Technique
Address for correspondence: Mr. Ardit Begaj, Department of Plastic Surgery, Royal Preston Hospital, Preston PR2 9HT, United Kingdom. E-mail: ardit.begaj@doctors.org.uk
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Adequate local anesthetic, in harvesting a split-thickness skin graft (SSG), traditionally involves multiple passes of a needle across the length and width of the marked donor site.
We describe a technique using hyaluronidase to uniformly anaesthetize an SSG donor site with one injection, in one pass, of one needle.
1. Preop application of EMLA cream/AMITOP to the donor site
2. Mix 10 mL 1% lidocaine solution with Adrenaline 1:200,000 with 1 vial of Hyaluronidase 1500 units. The mixture is buffered with 1 mL 8.4% sodium bicarbonate to neutralize acidity and minimize pain.
3. Mark out the SSG donor site
4. Using a 27-G long needle (sterican), enter perpendicular to the skin in the middle of the proximal aspect of the donor site. Inject some local anesthetic subdermally, creating a mound.
5. Change the angle of the needle to 180° and continue to inject the remaining anesthetic along one half of the width of the donor site.
6. Using a rolled 4 × 4 swab, apply firm advancing pressure to distribute the mound across the remaining width and length of marked donor site.
7. As the mound advances, the hyluronidase/anesthetic mixture will distribute uniformly across the donor site within the same plane. The skin blanches secondary to the adrenaline during its distribution.
The technique described is a fast, reproducible way to improve patient comfort through the elimination of repeated passes of a needle, distributing the anesthetic uniformly across the donor site, and facilitating the acquisition of an SSG of uniform thickness
Keywords
Graft
hyaluronidase
local anesthetic
split thickness
SSG
INTRODUCTION
Split thickness skin graft (SSG) is one of many tools in a plastic surgeons’ reconstructive toolbox, frequently harvested under local anesthetic (LA) for small clean defects. Donor site pain can prove the most distressing symptom to the patient perioperatively through multiple passes of a needle during LA infiltration and stimulation of nociceptive fibers during the partial thickness injury caused by the graft harvest.[12]
The use of hyaluronidase has been described in a variety of settings: treating extravasation of chemotherapy agents and its potentiating effect when used with LA in ophthalmic surgery.[3] Hyaluronidases are a family of endoglycosideses breaking down hyaluronic acid, the main component of extracellular matrix linking protein filaments, collagen fibers, and connective tissue cells within the skin.[4]
We describe a technique using hyaluronidase to uniformly anesthetize an SSG donor site with one injection, in one pass, of one needle.
TECHNIQUE
Preop application of EMLA cream to the donor site minimizing pain of needle entry.
Buffer 9 mL 1% lidocaine with adrenaline 1:200,000 with 1 mL 8.4% sodium bicarbonate. Mix this 10 mL with 1 vial of Hyaluronidase 1500 units powder for injection.
The SSG donor site margins are determined.
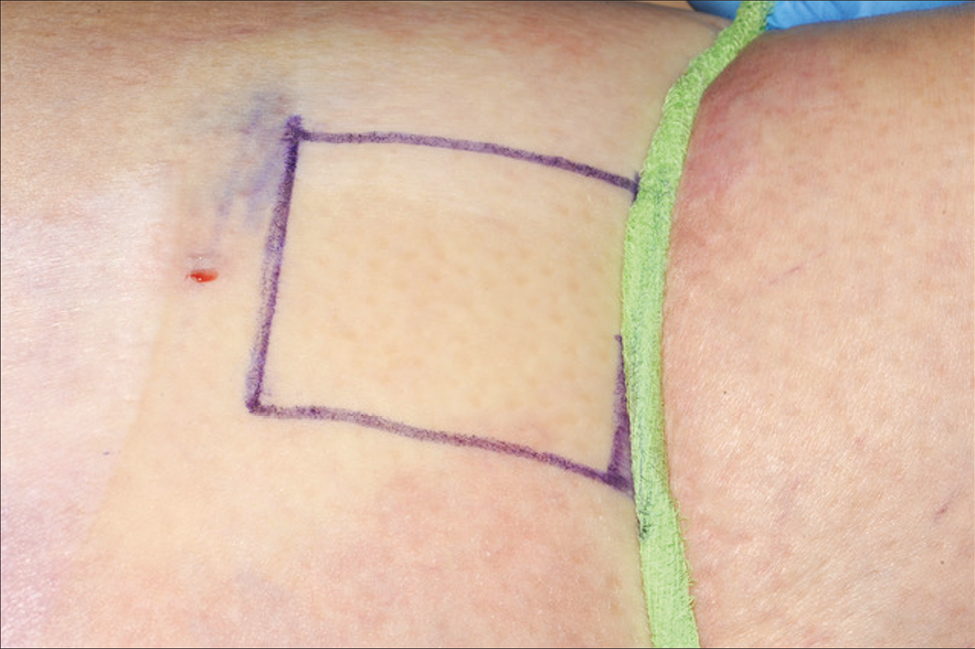
In the middle of the proximal aspect of the donor site, enter perpendicular to the skin and inject the LA mixture subdermally using a long 27G needle creating a mound [Figure 1].
Maneuver the needle near parallel to the skin and inject the remaining anesthetic along the width of the donor site [Figures 2 and 3].
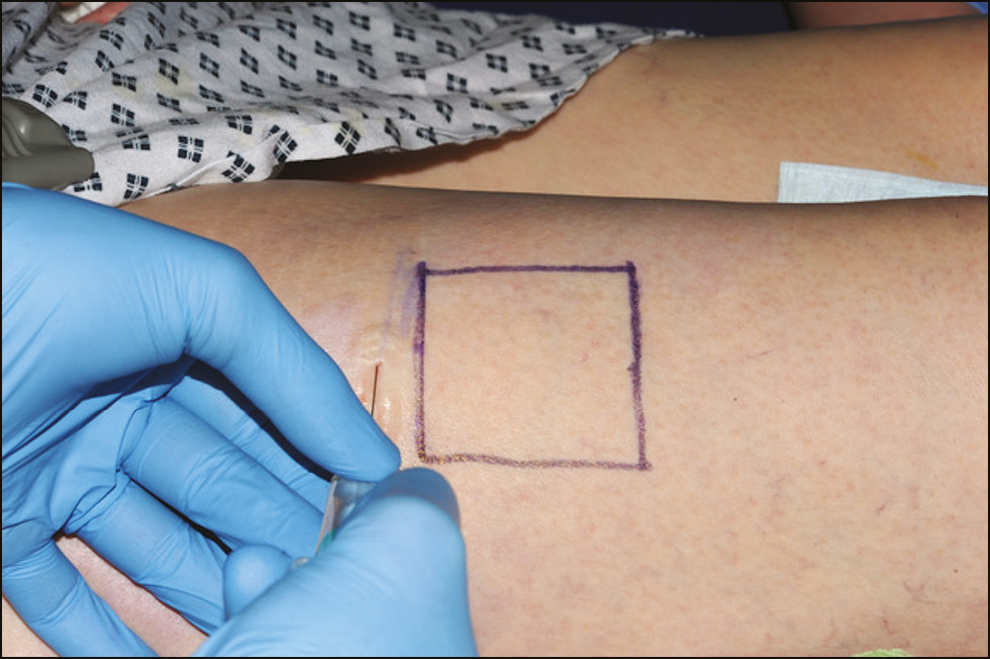
Using a rolled 4 × 4 swab, apply firm advancing pressure to distribute the mound across the remaining width and length of marked donor site [Figure 4].
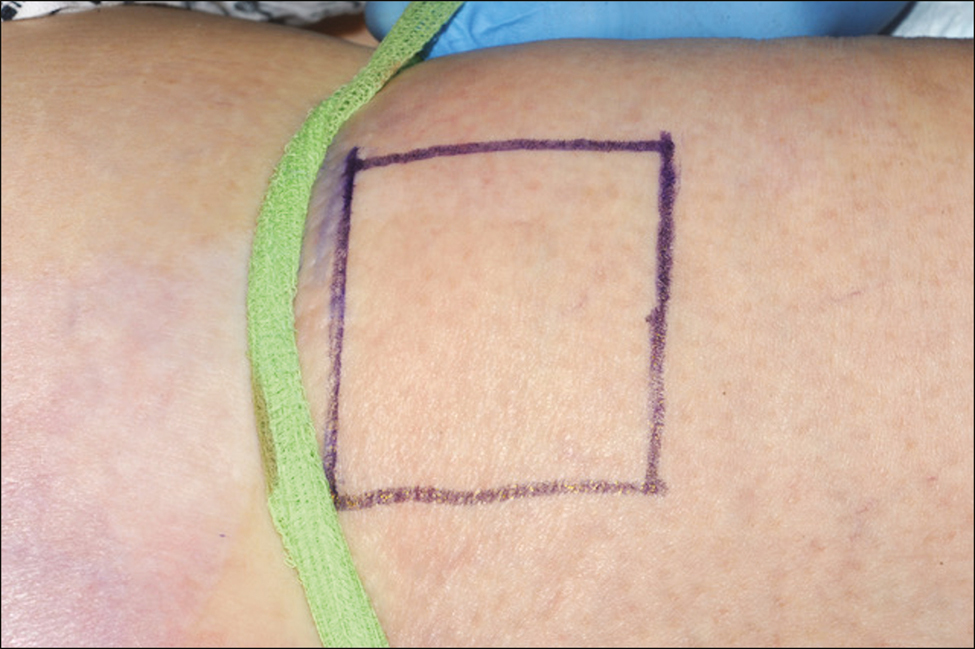
As the mound advances, the LA mixture distributes uniformly across the donor site within the same plane. Blanching skin secondary to the adrenaline identifies its distribution [Figure 5].
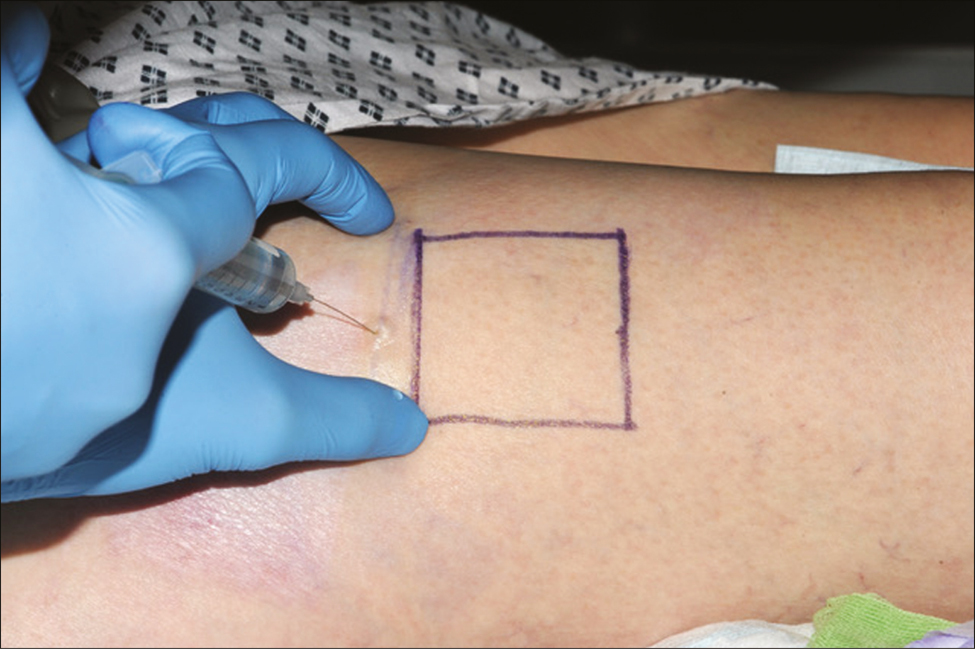
- Injection of local anesthetic by creating a mound
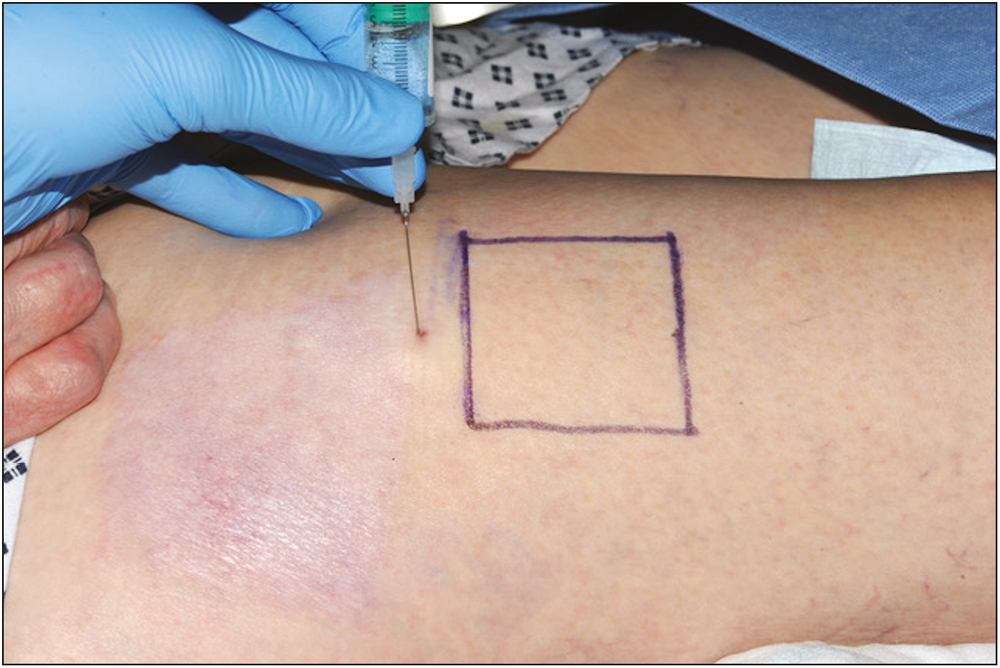
- Injection of local anesthetic along one half of the width of the donor site
- Injection of the remaining local anesthetic along the other half of the width of the donor site
- Apply firm advancing pressure to distribute the local anesthetic using a 4 x 4 swab
- Advance the rolled swab across the full length of the marked area
DISCUSSION
Harvesting an SSG under LA is known to be painful for patients for a number of reasons:
Cold LA
Secondary to the acidic PH of the LA
Multiple injections to the donor site for anesthetic and hemostatic control
The blade of the dermatome or knife in incompletely anaesthetized donor sites
Exposure of nerve endings following graft harvest
Patient anxiety reducing the threshold for pain tolerance
A randomized controlled trial (RCT) assessing efficacy of LA with hyaluronidase in scalp nerve blocks showed lower pain scores in these patients at 2, 4, 6 and 8h postoperatively. Intraoperatively this cohort had lower heart rates and blood pressure compared to those with LA without hyaluronidase.[5] This was also evident in an RCT assessing pain scores in carpal tunnel decompression.[6]
Studies comparing LA infiltration with hyaluronidase highlight its use results in immediate onset compared to a mean of 1 min 28s in LA without.[7] Furthermore, the area anaesthetized was increased by a mean factor of 2.45 and volunteers reported less discomfort during the infiltration. The rapid diffusion of the infiltrated bolus we illustrate in this technique results in a smooth contour, this, combined with the good biocompatibility of hyluronidase and rare incidence of allergic reaction (<0.1% of the cases) is optimal for uniform SSG harvest under LA.[8] Haemostatic control is provided by the use of LA with adrenaline.
Per ampoule of 1500 units, hyaluronidase costs £13.6 ($17.23).[9] This is comparable to the LA (1% xylocaine with adrenaline 1:200000) of £9.66 ($12.23) per vial[10] and sodium bicarbonate price of £11.41 ($14.45) per vial.[11]
We dilute 1 vial of hyaluronidase with 10 mL of LA mixture; however, the literature describes diluted concentration of 15 units/mL[12] increasing longevity and cost effectiveness.
CONCLUSION
The technique described is a fast and reproducible technique to:
Anaesthetize an SSG donor site in a single pass, of a single needle.
Distribute the anesthetic uniformly across the donor site, optimizing uniform graft harvest.
Maintain haemostatic control of the entire donor area without additional risk or time.
Compliance with ethical standards
This article does not contain any studies with human or animals performed by any of the authors. Informed consent was obtained from the individual participant.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Operative techniques for the minimization of skin graft donor-site pain in flap surgery. Plast Reconstr Surg. 2007;119:1393-4.
- [Google Scholar]
- Use of continuous local anesthetic infusion in the management of postoperative split-thickness skin graft donor site pain. J Burn Care Res. 2013;34:e257-62.
- [Google Scholar]
- Ophthalmic regional blocks: Management, challenges, and solutions. Local Reg Anesth. 2015;8:57-70.
- [Google Scholar]
- Safety and efficacy of addition of hyaluronidase to a mixture of lidocaine and bupivacaine in scalp nerves block in elective craniotomy operations; comparative study. BMC Anesthesiol. 2018;18:129.
- [Google Scholar]
- Pain levels after local anaesthetic with or without hyaluronidase in carpal tunnel release: A randomised controlled trial. Adv Orthop. 2015;2015:784329.
- [Google Scholar]
- Adjunctive use of hyaluronidase in local anaesthesia. Br J Plast Surg. 1986;39:554-8.
- [Google Scholar]
- Hyaluronidase: A review of approved formulations, indications and off-label use in chronic pain management. Expert Opin Biol Ther. 2010;10:127-31.
- [Google Scholar]
- [cited 2020 Mar 8]. Available from: https://bnf.nice.org.uk/medicinal-forms/hyaluronidase.html
- [cited 2020 Mar 8]. Available from: https://bnf.nice.org.uk/medicinal-forms/lidocaine-with-adrenaline.html
- [cited 2020 Mar 9]. Available from: https://bnf.nice.org.uk/medicinal-forms/sodium-bicarbonate.html
- Hyaluronidase reduces local anaesthetic volumes for sub-Tenon’s anaesthesia. Br J Anaesth [Internet]. 2007;99:717-20. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0007091217346998
- [Google Scholar]






