Translate this page into:
Successful hair transplant outcomes in cicatricial alopecia
*Corresponding author: Mukta Sharma, Department of Dermatology, AK Clinics, Ludhiana, Punjab, India. mukta1454@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma M, Dua A, Dua K, Bhardwaj B. Successful hair transplant outcomes in cicatricial alopecia. J Cutan Aesthet Surg. doi: 10.25259/JCAS_87_2024
Dear Editor,
Cicatricial alopecia (CA), or scarring alopecia, represents a rare and challenging group of conditions characterized by irreversible hair follicle destruction and subsequent hair loss. The condition can result from inflammatory, infectious, or traumatic processes and often leads to psychosocial distress due to its disfiguring nature.1 This letter highlights our case series of seven patients who underwent hair transplantation, achieving promising results despite the inherent challenges of CA.
Patients included in our series presented with diverse etiologies of CA, including lichen planopilaris, post-surgical scars from cleft lip repair, and post-traumatic alopecia. All patients underwent comprehensive disease stabilization protocols using a combination of systemic and topical immunomodulatory therapies. The disease inactivity was confirmed through clinical and histopathological evaluations, with stabilization periods ranging from 6 months to 2 years before surgical intervention.
We employed follicular unit extraction (FUE) as the surgical method of choice, as it allows for precise graft harvesting and implantation with minimal scarring, a critical factor in already compromised scalp or facial tissues. In cases with extensive scarring, test patches of 100–150 grafts were implanted to evaluate graft survival. Positive results in test areas, with graft survival rates exceeding 80%, justified proceeding with full-scale transplantation.
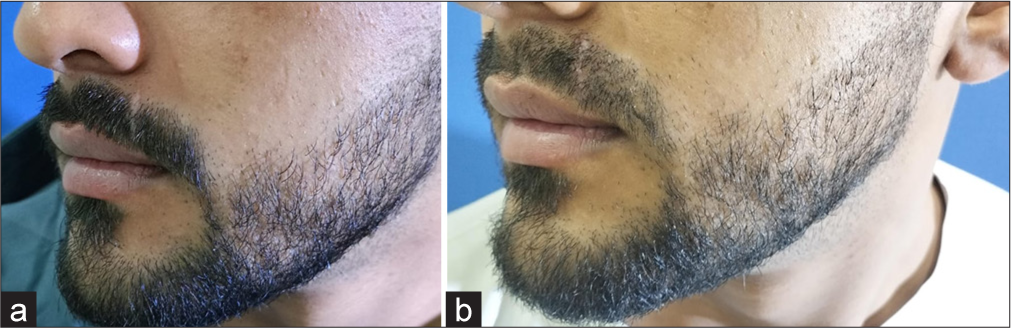
The outcomes were highly encouraging. A 36-year-old female with lichen planopilaris achieved 70% scalp coverage after two sessions involving 2,500 grafts [Figure 1]. Similarly, a 45-year-old male undergoing beard reconstruction attained 75% graft survival 6 months post-surgery [Figure 2]. Other patients [Figures 3-5], including those with post-traumatic and post-surgical scarring [Figures 6 and 7], demonstrated graft survival rates between 65% and 86%. Importantly, all patients reported high satisfaction with the cosmetic results, a testament to the meticulous planning and technique employed.
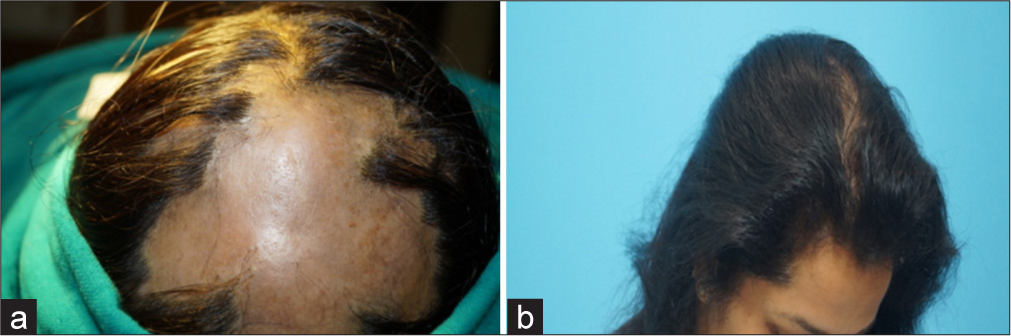
- (a) The patient presented with a large area of hair loss. (b) Final results a year later of the last session.

- (a) Pre-operative photographs before undergoing beard transplantation. (b) 1 year after the surgery.
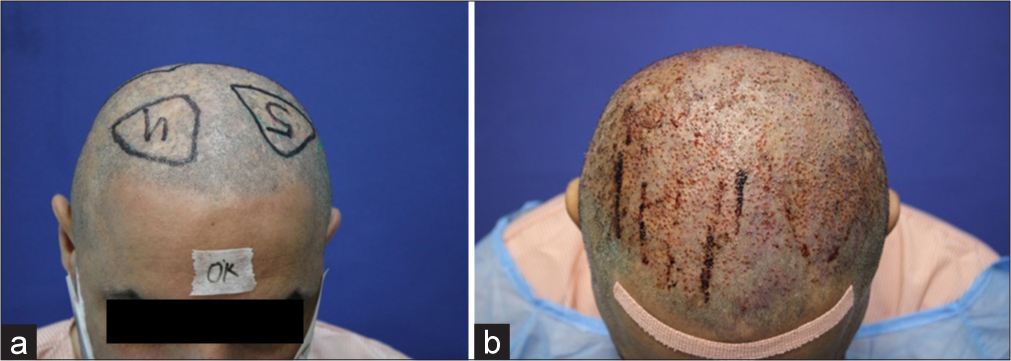
- (a) Pre-operative pictures. (b) Immediate post-operative pictures.

- (a) Pre-operative photographs during the time of presentation. (b) Eight months after surgery.

- (a) Pre-operative pictures of the patient showing scarring alopecia. (b) Results after 1 year.

- (a) Pre-operative pictures showing traumatic scarring alopecia. (b) 8 months after surgery.
- (a) Pre-operative picture. (b) 1 week post-surgery.
This case series underscores several critical considerations for successful outcomes in CA. Stabilization of disease activity remains paramount, as active inflammation compromises graft survival. Histopathological assessments to confirm disease inactivity, as seen in our series, align with recommendations from leading studies.2 The unpredictable vascularity in scarred tissues necessitates careful density modulation, with recipient site densities limited to 15–20 grafts/cm2 in poorly perfused areas. In our cases, densities were adjusted based on individual assessments, ensuring adequate coverage while minimizing ischemic complications [Table 1].
| Case no. | Age/Sex | Condition | Donor area | No. of grafts (test grafts and total number of grafts implanted) |
Technique | Growth (%) | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | 36/F | Lichen plano pilaris | Scalp | 100 (test), 2500 | FUE | 80 (test), 70 | Satisfactory coverage with high satisfaction |
| 2 | 45/M | Post-surgical beard alopecia | Scalp | 2400 | FUE | 75 | Aesthetic improvement, high satisfaction |
| 3 | 42/M | Cicatricial alopecia (since childhood) | Beard and scalp | 2200 | FUE | 70 | Significant coverage, ongoing improvement |
| 4 | 32/M | Follicular lichen planus | Scalp | 150 (test), 2200 | FUE | 80 (test), 86 | Full scalp coverage, high satisfaction |
| 5 | 47/F | Lichen plano pilaris (Burnt-out) | Scalp | 100 (test), 1410 | FUE | 80 | Good cosmetic result, patient satisfied |
| 6 | 29/M | Post-operative upper lip scar | Scalp | 210 | FUE | 65 | Moderate improvement in scar area |
| 7 | 25/M | Post-traumatic scar (moustache and scalp) | Scalp | 250 | FUE | - | Planned for future assessment |
FUE: Follicular unit extraction, F: Female, M: Male.
Despite these challenges, hair transplantation for CA offers renewed hope for patients, as supported by recent literature reporting graft survival rates of 60–85%.3 Advanced surgical techniques such as FUE, combined with thorough pre-operative planning, are pivotal for achieving satisfactory outcomes. Moreover, staged procedures, as utilized in our series, mitigate the risks of ischemia and ensure optimal healing between sessions.4
In conclusion, hair transplantation in CA, while technically demanding, can yield successful results with proper stabilization, surgical precision, and patient counseling. The outcomes of our series contribute valuable insights into managing this challenging condition and highlight the transformative impact of such interventions on patient quality of life.
Acknowledgments:
We thank the patients for their consent to share these experiences. There are no conflicts of interest or funding disclosures.
Authors’ contributions:
Mukta Sharma: Wrote the manuscript and reviewed literature. Aman Dua, Kapil Dua, Bhawna Bhardwaj: Involved in concept, manuscript editing, guidance, conducting the cases and approval of the final version of the manuscript.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Cicatricial alopecia: Clinico-pathological findings and treatment. Clin Dermatol. 2001;19:211-25.
- [CrossRef] [PubMed] [Google Scholar]
- The assessment of Hair transplantation outcomes in cicatricial alopecia. Int J Trichology. 2020;12:164-7.
- [CrossRef] [PubMed] [Google Scholar]
- The surgical treatment of cicatricial alopecia. Dermatol Ther. 2008;21:295-311.
- [CrossRef] [PubMed] [Google Scholar]
- Hair transplantation in the cicatricial alopecias. Hair Ther Transplant. 2013;3:109.
- [Google Scholar]





