Translate this page into:
Successful treatment of ulcers of bullous morphea with platelet-rich fibrin therapy
*Corresponding author: Payal Chauhan, Department of Dermatology, AIIMS Vijaypur, Jammu and Kashmir, India. chauhanpayal89@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dhiman A, Chauhan P, Daroach M. Successful treatment of ulcers of bullous morphea with platelet-rich fibrin therapy. J Cutan Aesthet Surg. doi: 10.25259/jcas_25_24
Dear Editor,
Bullous morphea, a rare variant of morphea, first described in 1896 by Morrow.1,2 The frequency of bullous morphea is estimated to be approximately 7.5% of all cases of scleroderma. Traditional treatment approaches for morphea-related ulcers include phototherapy, topical and systemic corticosteroids, immunosuppressants like methotrexate, antimalarials, salazopyrin, and colchicine.3 However, ulcers in morphea can be particularly challenging to treat. Herein, we present a case in which ulcers are treated with platelet-rich fibrin (PRF) therapy along with hydroxychloroquine.
A 69-year-old female presented with excruciating bilateral foot ulcers which were preceded by thickening and blistering of skin from the past 2 years. On examination, there were erythematous, shiny indurated plaques, with overlying painful ulcers of varying sizes over dorsum of both feet [Figure 1]. Dermoscopic examination showed white fibrotic beams, yellow structureless areas, linear branching, and dotted vessels [Figure 2a]. Histopathological analysis revealed closely packed collagen bundles and dilated lymphatics in the dermis, consistent with bullous morphea [Figure 2b]. The patient was started on methotrexate and pentoxifylline as an initial treatment modality for 6 months, but with minimal improvement. Consequently, hydroxychloroquine and topical steroids were introduced. Continued progression of size of ulcer prompted us to look for alternative treatment; PRF therapy was added to the existing treatment. The procedure involved collection of 5 mL of whole blood a plain vacutainer for preparation which was promptly centrifuged at 3000 revolutions per minute for a duration of 10 min, PRF matrix was derived, and ulcer base was covered with it [Figure 3a] and dressed with non-adherent dressing. After 5 days, dressing was removed and wound/ulcer was covered with sterile paraffin gauze dressing daily. The procedure was repeated monthly for 4 months. There was considerable improvement after 3rd session [Figure 3b] and almost complete healing of ulcer at end of 4 months [Figure 3c].

- Erythematous shiny indurated plaques with overlying ulcers of varying sizes over the dorsum of both feet.
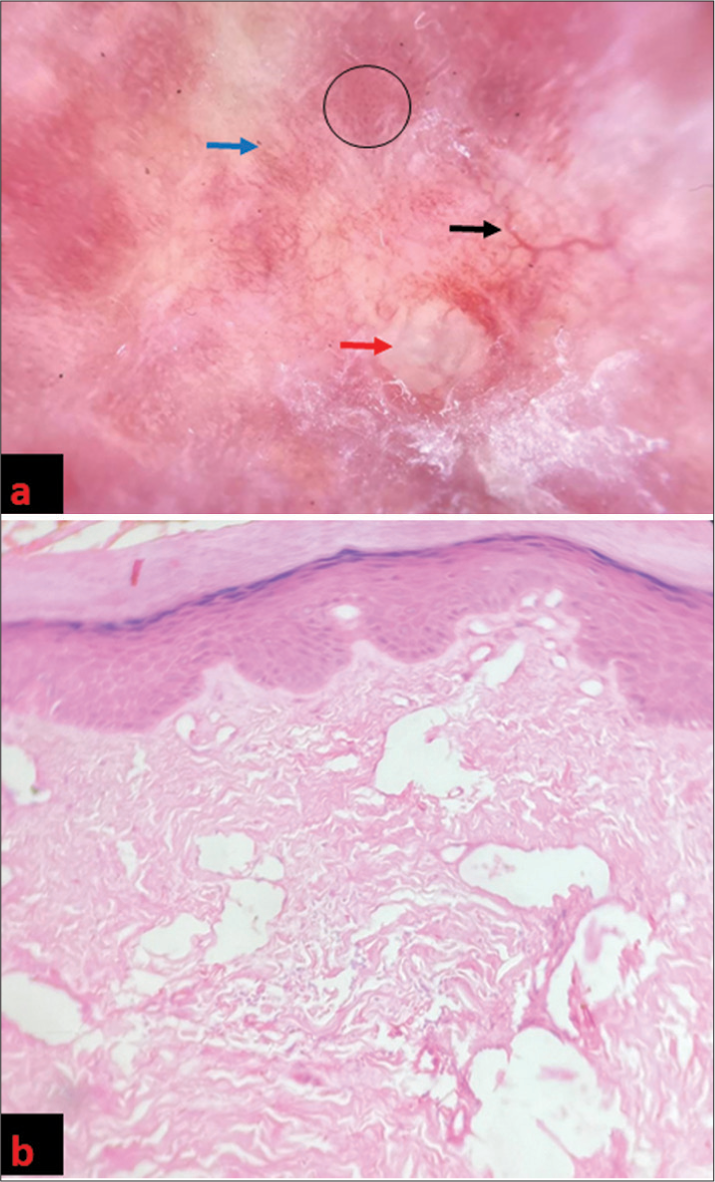
- (a) Dermoscopy (DermLite DL4; 3Gen; San Juan Capistrano, California, USA, noncontact polarized mode, ×10 magnification, images capture with DermLite adapter for iPhone 12 pro max) demonstrated white fibrotic beams (blue arrow), yellow structureless areas (red arrow), linear branching (black arrow), and dotted vessels (black circle). (b) Histopathologic examination (HPE) showed closely packed collagen bundles and dilated lymphatics in the dermis at ×20.

- (a) Ulcer base over medial aspect of left foot covered with platelet-rich fibrin (black arrow). (b) Ulcer size reduced after 3rd session. (c) Almost complete healing of ulcer after 4th session at 4 months.
The exact etiology remains unclear, but proposed causes are lymphatic obstruction, vascular dilation, trauma, and infiltrating cells within fibrotic areas, perivascular inflammation with an eosinophil granule component such as major basic protein, or vascular changes such as arteritis and phlebosclerosis.3
Treatment of such cases remains challenging. In this case, PRF therapy was administered to the patient along with hydroxychloroquine. The patient experienced a reduction in ulcer size, as well as a reduction in pain and burning sensation. Ulcers in our case started improving after the second session. Choukroun et al. first described PRF for the use in oral and maxillofacial surgery, which is enriched with growth factors, including vascular endothelial growth factor, transforming growth factor β1, and insulin-like growth factor, as well as cytokines such as interleukin-1β, interleukin-6β, and tumor necrosis factor-α which can be used for promoting wound healing.4-6 Prescribed protocol suggested weekly PRF dressing as for a maximum of five sessions as growth factors were released over approximately 1 week in a controlled manner, but travel distance to hospital has led to a modification of the plan to monthly sessions. Despite this, positive outcomes were achieved with no adverse effects.
Topical esmolol hydrochloride gel and becaplermin gel (recombinant human platelet-derived growth factor [PDGF] subunit B) can be used as topical agents in such cases.7,8 Other dressing that can be done in ulcers are hydrogels, foams, hydrocolloid, alginate and film dressings, and recombinant human (rh)-PDGF dressing.9
In this case, PRF therapy led to a notable improvement in the patient’s condition. After four PRF sessions, there was a nearly complete resolution of some lesions, along with a decrease in ulcer size.
This response highlights the potential of PRF therapy which is a simple, feasible, and inexpensive innovative approach for the treatment of difficult-to-manage morphea ulcers. The limitations of this report include not being able to conduct weekly follow-ups with the patient. Additional studies are necessary to validate the results observed in this case.
CONCLUSION
Ulcers in bullous morphea remain a challenging condition to treat, especially when ulcers are present. Conventional therapies may yield limited results, necessitating alternative approaches. The presented case underscores the potential efficacy of PRF even after monthly sessions in promoting wound healing and tissue regeneration through the release of growth factors and cytokines.
Authors’ contributions
Manju Daroach and Avita Dhiman had full access to all of the data in the study and took responsibility for the integrity and accuracy of the data. Study concept and design: Manju Daroach, Avita Dhiman, Payal Chauhan. Acquisition, analysis, and interpretation of data: Avita Dhiman, Manju Daroach. Drafting of the manuscript: Avita Dhiman, Payal Chauhan, Manju Daroach. Critical revision of the manuscript for important intellectual content: Manju Daroach, Payal Chauhan.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A case of symmetrical morphea attended with the formation of bullae and extensive ulceration. J Cutan GenitoUrin Dis. 1896;14:419-27.
- [Google Scholar]
- Bullous morphea: Description of a new case and discussion of etiologic and pathogenic factors in bulla formation. Actas Dermosifiliogr. 2017;108:75-6.
- [CrossRef] [PubMed] [Google Scholar]
- Bullous morphoea: A retrospective study. Clin Exp Dermatol. 2017;42:532-5.
- [CrossRef] [PubMed] [Google Scholar]
- Platelet-Rich fibrin: A second generation platelet concentrate and a new friend of oral and maxillofacial surgeons. Ann Maxillofac Surg. 2011;1:53-7.
- [CrossRef] [PubMed] [Google Scholar]
- Role of platelet-derived growth factor in wound healing. J Cell Biochem. 1991;45:319-26.
- [CrossRef] [Google Scholar]
- Topical esmolol hydrochloride as a novel treatment modality for diabetic foot ulcers: A phase 3 randomized clinical trial. JAMA Netw Open. 2023;6:e2311509.
- [CrossRef] [PubMed] [Google Scholar]
- Becaplermin gel in the treatment of diabetic neuropathic foot ulcers. Clin Interv Aging. 2008;3:233-40.
- [CrossRef] [PubMed] [Google Scholar]
- Selection of appropriate wound dressing for various wounds. Front Bioeng Biotechnol. 2020;8:182.
- [CrossRef] [PubMed] [Google Scholar]






