Translate this page into:
Surgical Management of Oral Mucocele: Experience with Marsupialization
Address for correspondence: Prof. Chander Grover, Department of Dermatology and STD, UCMS and GTB Hospital, Dilshad Garden, Delhi-110095, India. E-mail: chandergroverkubba76@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Oral mucoceles are a common and nagging problem. They are proposed to be a result of damage to the minor salivary gland structure, resulting in retention or extravasation of saliva which leads to these cystic lesions. The lesions may often resolve spontaneously but frequently recur, or even epithelialize over long periods of time. This study reports the results of surgical management of oral mucocele by marsupialization. Even though, a complete surgical removal is considered the treatment of choice for oral mucocele, it has associated disadvantages including a longer recovery period and potential for ductal damage, which can lead to scarring, recurrence, and development of further satellite lesions. As the study shows, marsupialization is a simple surgery which ensures faster healing, minimizes postoperative complications, and is associated with a minimal risk of recurrence or development of new lesions. Owing to the satisfactory response to marsupialization, it may be considered as first line therapy in the management of oral mucoceles.
Keywords
Chalazion clamp
cruciate incision
mucocele
A mucocele is a glandular collection, commonly arising from the salivary glands, but it is also reported in other locations such as the lacrimal sac, paranasal sinuses, etc. The oral mucocele is a common lesion, seen in 0.4–0.9% of the general population. It is characterized by a rapid appearance, specific location, history of trauma, bluish color, and cystic consistency.[1] Almost 70% lesions arise in the lower labial mucosa.[2] Though asymptomatic, treatment is often requested due to the size of the lesions. We have been treating these lesions with the simple technique of marsupialization for the past 5 years, with good results.
Data from a total of 13 patients with 17 oral mucoceles treated over the past 5 years were retrospectively analyzed. There were eight males and five females in this group (M:F ratio being 1.6:1). The mean age at presentation was 17.9 years (range 8–30 yrs). Nine patients presented with a single large lesion causing discomfort, whereas four patients had two or more lesions requiring intervention. Of these, two patients had numerous lesions that were visualized better on magnification [Figures 1 and 2]. The lesion of interest was present in the labial mucosa [Figures 1 and 2] (15/17 or 88.2%) or buccal mucosa [Figure 3] (2/17 or 11.8%) cases. The average size of the lesion was 13.2 mm (range 5–25 mm). The majority of the lesions presented as a translucent cystic nodule [Figures 1 and 2] (6/17 or 35%), a bluish translucent cyst [Figure 4] (6/17 or 35%), or whitish papule or tag-like appearance [Figure 2] (5/17 or 29.3%) cases.

- Two relatively large, superficial mucoceles placed centrally over the labial mucosa in a young girl

- A large epithelialized mucocele placed on the left side of the buccal mucosa. Several much smaller lesions in the vicinity are noticed.

- A mucocele in the buccal mucosa

- A large, superficial, bluish-colored mucocele causing a distortion in the lip structure
All the patients were treated with marsupialization. The area was cleaned with povidone iodine, with the patient clenching a piece of sterile gauze between his teeth. Local anesthesia, a combination of 2% lignocaine with adrenaline, was given [Figure 5A]. A chalazion clamp was then used to encircle and hold the mucocele [Figure 5B]. It helped by making the lesions prominent, provided grip over slippery mucosa, and also minimized bleeding. A cruciate incision (two incisions perpendicular to each other) was given over the most prominent part of the lesion [Figure 5C, D]. The incisions were deep enough to reach the cyst cavity, discharging the mucoid contents that were cleaned and emptied. Subsequently, the four triangular flaps of the cyst roof were snipped with a sharp scissors to de-roof the cavity [Figure 5E], making the floor of the cyst a part of the oral mucosa. This formed a continuous surface from the exterior to the interior of the cyst [Figure 5F]. No sutures were applied, and hemostasis was secured with pressure or with a gauze soaked in adrenaline. The chalazion clamp was relieved, and the site was packed for 10–15 min to ensure there was no ongoing bleeding. The patient was prescribed antiseptic gargles for a week and nonsteroidal anti-inflammatory drug for 3–4 days. Softer diet was advised for the first 2–3 days, and patients were reviewed at 1 week to assess resolution and complete healing in all cases [Figure 6A, B]. Recurrence was observed in 2 out of 17 cases (11.7%), at 2–3 weeks, which was treated with a repeat of the same procedure by using a deeper incision, leading to complete resolution.
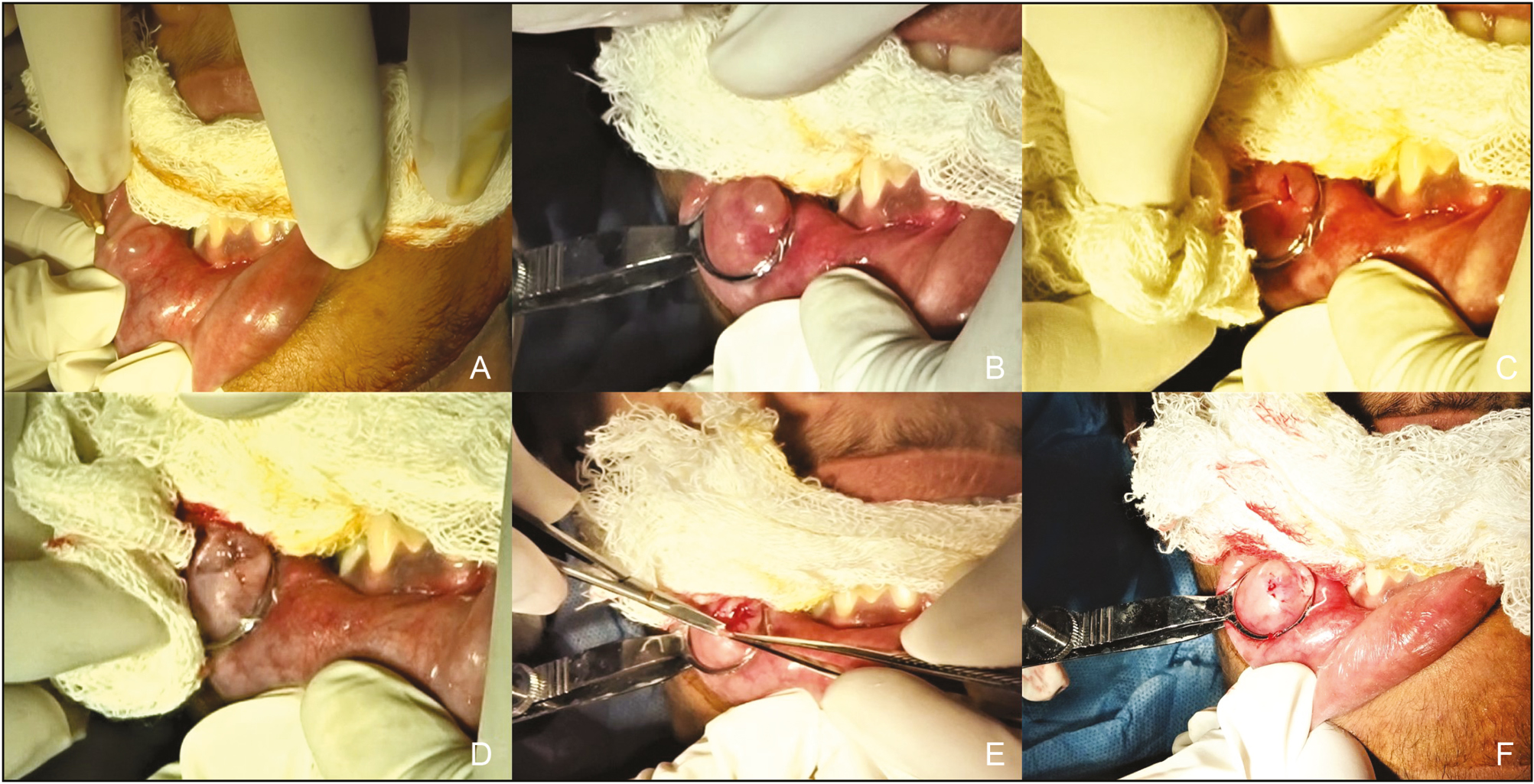
- A-F: Marsupialization of a mucocele. (A) Local anesthesia with 2% lignocaine and adrenaline solution is injected around the lesion. (B) A chalazion clamp is applied to ensnare the lesion, enabling easier grip. (C) The first incision is made over the top of the cyst. Note the gelatinous material being extruded, which is removed. (D) The second incision is made perpendicular to the first one, making a cross. The contents of the mucocele are totally evacuated. (E) The four flaps of the roof of the mucocele are then excised with the help of a scissors. (F) Postremoval of flaps, it can be seen that the floor of the mucocele becomes a part of the floor of the labial mucosa. Only mild bleeding is seen from the edges, which can be easily controlled with pressure.
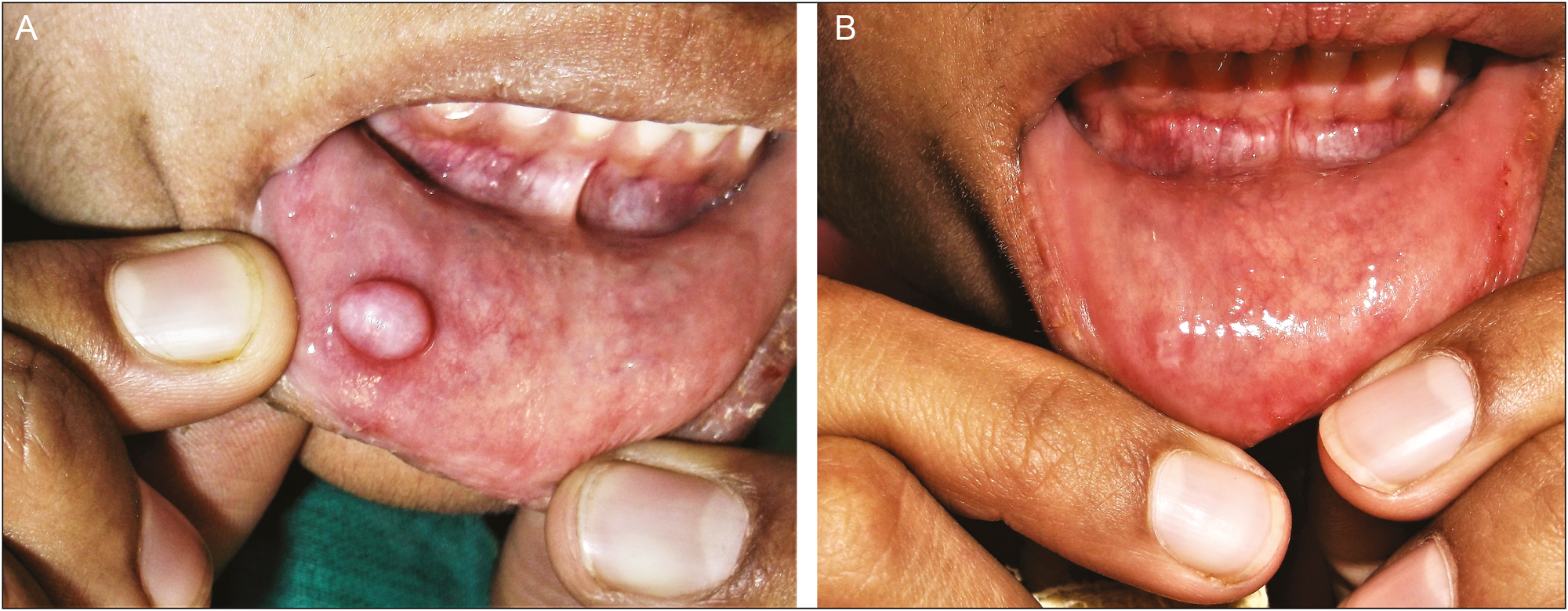
- A, B: Result of marsupialization of a large mucocele. At the end of 1 week, there has been rapid healing with a barely noticeable scar
Oral mucocele is the most common benign lesion of the oral cavity,[3] frequently arising in the 2nd to 3rd decade, though it may occasionally be present at birth. Mucoceles are a result of traumatization (extravasation mucocele) or blockage of the salivary gland duct (retention mucocele).[1] Various acquired causes include trauma (lip/ cheek biting, piercing), mucosal inflammation, immunological reaction, chronic inflammation, infection, and duct obstruction due to sialolith or dense mucosa. Multiple lesions are generally a result of oral mucosal inflammation associated with Sjogren’s syndrome, sarcoidosis, HIV, lichen planus, lichenoid drug reaction, and chronic graft-versus-host disease. Some reports have implicated the use of tartar-control toothpastes, or even neoplasia. Advanced or larger lesions may be associated with granuloma or pseudo-capsule formation.
Clinically, the most common site of presentation is the lower lip, as was seen in our series.[3] The lesions are usually asymptomatic, with most of our patients presenting only with an awareness of a swelling or mild discomfort. Color variation depends on the size and surface proximity of the lesion. Superficial lesions tend to be bluish, whereas deeper lesions may have a mucosal color. The same was corroborated in our findings. Patients with white, keratotic papules were the ones with a longer standing history.
Mucoceles may resolve spontaneously, and this history was given by a majority of our patients, who, however, experienced a recurrence after varying periods. Superficial mucoceles are likely to recur periodically, with new lesions developing over time. This history is especially useful for ruling out differential diagnoses such as fibroma, lipoma, sialolith, phlebolith, salivary gland neoplasms, etc. Diagnosis can also be confirmed by simple aspiration or fine needle aspiration cytology (FNAC).
Various treatment modalities described in the literature include intralesional steroids (betamethasone or dexamethasone), sclerotherapy, ablation, or surgical removal.[5] Ablative therapy with laser or cryosurgery is useful for multiple lesions.[4] However, surgical removal is the most definitive and most commonly used treatment. We opted for conservative surgery, that is, marsupialization as compared with surgical excision (treatment of choice but with a longer downtime and more scarring),[5] or micro-marsupialization (involves retained sutures in the oral cavity for a week).[6] Marsupialization is useful for cysts where single draining may not be effective; at the same time, complete removal of surrounding structures is not desirable. It is well described for Gartner’s duct cyst, Bartholin’s cyst, pancreatic cysts, pilonidal cysts, dacryocystorhinostomy, or endoscopy. However, literature on oral mucoceles is limited. In oral mucoceles, suturing of edges is also not required as lesions are often small, and pressure hemostasis is achievable. Other advantages include lesser chances of recurrence, faster healing as not much epithelialization is required,[7] lesser risk of secondary infection as lesser raw surface is exposed, and the ability to deal with larger lesions without much collateral damage.[8]
Postoperative advice is similar to other mucosal surgeries, such as a soft- or liquid-based, bland diet and strict avoidance of hot beverages and tobacco. However, the extent of dietary modification required was quite minimal, with most patients resuming a normal diet by the 3rd to 4th day. For patients with multiple lesions, preventive advice includes avoidance of trauma, habits that irritate minor salivary glands (sucking, chewing on lips or tongue etc.), restoration of damaged teeth or orthodontic appliances, wearing mouthguards during contact sports, treating mucosal disease, and managing xerostomia. Potential complications include bleeding, damage to peripheral nerves, injury to Wharton’s duct, stenosis, obstructive sialadenitis, saliva leakage, injury to lingual nerve, temporary/ permanent paresthesia, postoperative hematoma, infection, or wound dehiscence. Fortunately, these are associated with more extensive surgery and did not occur in any of our cases.
To conclude, marsupialization is an effective surgical treatment for oral mucoceles requiring treatment. It is associated with lesser downtime, minimal adverse effects, and higher treatment success rates.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form/forms, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Oral mucocele in infant with an unusual presentation. BMJ Case Rep. 2020;13:e234669.
- [Google Scholar]
- Benign tumours and tumour-like lesions in the oral cavity: A retrospective analysis. Postepy Dermatol Alergol. 2019;36:744-51.
- [Google Scholar]
- Nonsurgical management of oral mucocele by intralesional corticosteroid therapy. Int J Dent. 2016;2016:2896748. doi: 10.1155/2016/2896748
- [Google Scholar]
- Treatment of mucus retention phenomena in children by the micro-marsupialization technique: Case reports. Pediatr Dent. 2000;22:155-8.
- [Google Scholar]
- Treatment of ranula—excision of the sublingual gland versus marsupialization. Auris Nasus Larynx. 2003;30:311-4.
- [Google Scholar]
- Marsupialization for treatment of oral ranula: A second look at the procedure. Journal of Oral and Maxillofacial Surgery. 1992;50:1274-9.
- [Google Scholar]






