Translate this page into:
Surgical management of xanthelasma palpebrarum: Reducing angular defect through extended excision technique
*Corresponding author: Siddharth Mani, Department of Dermatology, Indian Naval Hospital Ship Sanjivani, Kochi, Kerala, India. smani5931@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mani S, Khandare M, Chaitanya YV, Neema S, Ranjan E, Raut A, et al. Surgical management of xanthelasma palpebrarum: Reducing angular defect through extended excision technique. J Cutan Aesthet Surg. doi: 10.25259/JCAS_66_2024
Abstract
Objectives
Xanthelasma palpebrarum (XP) is a common type of cutaneous xanthoma, typically presenting as yellowish papules or plaques around the eyes. Often associated with dyslipidemia, XP may indicate underlying conditions such as non-alcoholic fatty liver disease and hypothyroidism. Various surgical techniques are employed to remove XP, but simple excision can lead to angular deformities, particularly in cases involving the upper eyelid crease. This study aimed to quantify angular deformities resulting from XP excision and propose a surgical method to minimize these defects.
Material and Methods
Conducted between March 2023 and December 2023, the study included 30 patients diagnosed with a Grade I XP. Patients were divided into two groups: Group A underwent simple lesional excision, while Group B had excisions extended to the lateral canthus. Selection and description of participants were based on specific criteria: Aged over 18 years, having Grade I XP touching the upper lid crease, and no previous treatments. Exclusion criteria included active pregnancy, skin infections, bleeding disorders, keloid history, recurrent herpes, preference for non-surgical treatment, Grade II-IV XP, and inability to follow-up for at least 6 months. The study included 30 patients (26 females and four males) with an age range of 26–54 years. Pre-operative evaluations included detailed eye examinations and biochemical tests. Surgeries were performed under local anesthesia, using 6-0 polypropylene sutures, with a 7–10-day post-operative follow-up for suture removal. Group B’s excisions were tapered to match the lesion’s width. Angular defects were measured postoperatively.
Results
All patients achieved complete lesion clearance with no recurrence after 6 months. Group A showed an average angular deformity of 143.9°, while Group B had minimal to no deformity. Complications were higher in Group B, but angular deformities were significantly reduced.
Conclusion
Extending the excision to the lateral canthus effectively minimizes angular deformities in XP surgeries. Proper surgical technique and comprehensive pre-operative assessments, including pinch tests, are crucial to avoid complications and recurrences.
Keywords
Angular defect
Extended excision
Xanthelasma palpebrarum
INTRODUCTION
Xanthelasmas are the most common type of cutaneous xanthomas and are usually localized in the periorbital area, wherein we use the term xanthelasma palpebrarum (XP). Clinically, they present as yellowish papules to plaque and are a source of esthetic concern for the patient. The exact prevalence is not known in the Indian context. The entity is associated with dyslipidemia; hence, it is advisable to get the lipid profile checked for any patient presenting with it. XP has been shown to be associated with both non-alcoholic fatty liver disease and hypothyroidism; hence, a liver and thyroid function test should also be done.1,2
Lee et al. classified XP into four grades according to lesion extension: Grade I, lesions on upper eyelids only; Grade II, lesions extend to medial canthal area; Grade III, lesions on the medial side of both upper and lower eyelids; and Grade IV, diffuse lesions that involve medial and lateral of both upper and lower eyelids.3
Persistent and atypical XP must be distinguished from necrobiotic xanthogranuloma, as the latter is associated with monoclonal gammopathy and other hematological malignancies.4
Several therapeutic methods have been described in the literature thus far, including surgical excision, laser therapy, chemical peeling, cryotherapy, radiofrequency ablation, plasma sublimation, and dermabrasion. Each modality has its advantages and disadvantages. Surgical management is the most used modality and different surgical techniques have been mentioned for the same. These include but are not limited to a simple excision, uncapping, microsurgical inverted peeling, skin graft, modified blepharoplasty, incision incorporating turnover flap, switch flap, or hinged flap.5
Simple excision is the most commonly used technique described in the literature. Most patients with xanthelasma are middle aged, having lateral hooding and ptotic appearance of the upper eyelid. Simple excision of the XP that is present on the medial side and is touching the upper lid crease leads to an angular defect and lateral hooding of the lid. Herein, we report angular deformity associated with simple excision of the lesion and a new surgical method to minimize this angulation and lateral hooding.
Aims and objective
The study aims to find out the degree of angular defect associated with surgical excision of XP involving the upper lid crease of the medial side and to devise a method to decrease this angular defect.
MATERIAL AND METHODS
The study was conducted between March 2023 and December 2023 at a tertiary care center in Southern India. A formal ethical committee approval and informed consent from patients was taken. All patients over the age of 18 years presenting with Grade I XP touching the upper lid crease were included in the study. Patients with a history of concurrent or past treatment, pregnant women, active skin infections at the site of lesion, bleeding disorders, history of keloid or hypertrophic scar formation, patients who were unwilling for surgery, Grade II/III/IV xanthelasma, and those who were not willing or available for a follow-up period of at least 6 months were excluded from the study. Biochemical investigations, including blood sugar, lipid profiles, liver function tests, and thyroid profiles, were carried out for all the patients.
The patient’s eyes were examined in great detail, including blinking rate, evidence of ptosis, seventh cranial nerve function, and all the eyeball movements. All the patients were informed about the two procedures and the disadvantages associated with each. After taking the informed consent, patients were divided into two groups. Patients in Group A underwent simple lesional excision, and in Group B, patients underwent excision of the upper lid till the level of lateral canthus, including the XP lesion [Figure 1a-c]. All the patients underwent a pre-operative pinch test to rule out the possibility of ectropion [Figure 2]. The surgeries were done under local anesthesia (2% lidocaine with 1:100,000 epinephrine). The patients waited for 10 minutes post-LA before the incision was given to minimize the intraoperative bleeding.6 6-0 Polypropylene sutures were used in interrupted fashion in all the cases, and the suture removal was done after 7 days in group A and 10 days in group B. A single dermatologist along-with the assistance of an ophthalmologist for few cases accomplished the surgeries. Serial pre-operative and post-operative photographs were taken for all the patients and angular defect was measured in both the set of patients with the help of a protractor. The patients were analyzed after 4 weeks for angular defect and after 24 weeks for any recurrence.

- (a) A simple elliptical excision with the black border shows the marking of incision line. (b) Elliptical excision extending till lateral canthus with width being similar to maximum width of xanthelasma with the black border showing the marking for incision line. (c) Group B-Patient with excision extending till the level of lateral canthus. Tip of xanthelasma is marked with a yellow line and the end point at the level of lateral canthus is marked with a blue line. Note the constant width of the excision which is similar to the maximum width of xanthelasma.

- Pre-operative pinch test to rule out possibility of post-surgery ectropion.
RESULTS
A total of 30 patients were included in the study. Ten patients had lesions on both the eyelids making it a total of 40 XP lesions. A total of 20 lesions were excised under group A and 20 lesions were removed in group B. Out of 30 patients, 26 were female and 4four were male. The age ranged between 26 and 54 years with the mean being 40.9 (± 7.57) years. The mean duration of lesion was 1.3 years (range 6 months–3 years). Out of 30 patients, five patients had deranged lipid profiles. None of the patients had altered thyroid or liver function test profiles. In all the cases, the xanthelasma deposit was above the orbicularis muscle and no infiltration into deeper layers was seen. No muscle resection or flaps was required during the surgical procedure. In both groups, patients achieved complete clearance of the lesion with no recurrence observed in the 6-month follow-up period.
In group A, the average angular deformity was 143.9° and the range was between 136° and 158° [Figure 3a-c]. A more acute angle meant a greater alteration in contour. In group B, out of 20 XP lesions that were removed, only one patient showed an angular deformity of 150° while the other 19 had no angular deformity [Figure 4a-c]. The possible explanation for the deformity in this group was the greater width of xanthelasma that prompted the surgeon to cut the remaining lid in a width that was smaller than the lesional width leading to minor angular deformity.

- (a) Angular deformity of 141° is shown by yellow line and lateral hooding is shown by red arrow. (b) Angular deformity of 137.5° is shown by the yellow line and lateral hooding is shown by the red arrow. (c) Angular deformity of 138° degree post simple excision is shown by the orange line.
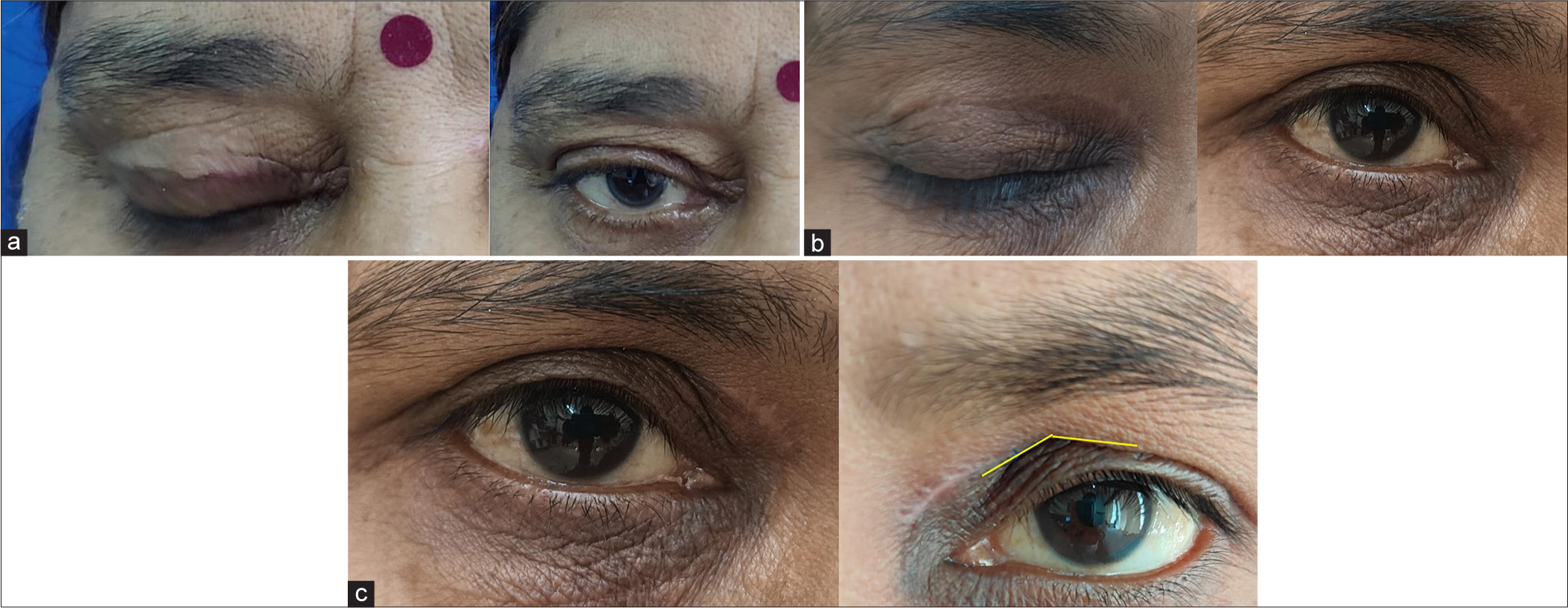
- (a) No angular deformity when the lid is removed till lateral canthus, (b) no angular deformity when the lid is removed till lateral canthus, and (c) post-operative image of same patient who underwent simple excision in the left eye with angular defect of 137° shown by yellow line and no angular deformity in the right eye in which excision extended till lateral canthus.
The adverse effects associated with each group are mentioned in Table 1.
| Adverse effect | Group A (20 XP lesions) |
Group B (20 XP lesions) |
|---|---|---|
| Pain duration | Average duration -3 days with a maximum of 5 days |
Average duration -7 days with a maximum of 10 days |
| Swelling | 4 lesions (eyelids) | 16 lesions (eyelids) |
| Contusion | 1 lesion (eyelids) | 8 lesions (eyelids) |
| Healing time | 7–10 days | 10–14 days |
| Lateral hooding | 10 lesions (eyelids) | None |
| Angular defect | All lesions | One |
| Hypertrophic scar | Nil | Nil |
| Hyper/hypopigmentation | Nil | Nil |
| Ectropion | Nil | Nil |
XP: Xanthelasma palpebrarum
DISCUSSION
Surgery has traditionally been the standard treatment for XP, particularly for lesions that extend into the deep dermis.5 The surgical approach to XP is based on treating it as localized benign deposition of fatty tissue, ensuring surgically free borders, and removal of the entire lesion. The specific surgical technique depends on the lesion’s size, its location on the eyelid, and the skin’s laxity. The pinch test is used to determine the excess skin in the upper eyelids, guiding the decision to perform simple excision, blepharoplasty, lateral canthopexy, skin flap, or graft.
Smaller lesions (Grade I) can be safely managed with simple excision, with or without blepharoplasty and primary closure, typically resulting in minimal pigmentary changes or scarring, for Grade II lesions, excision with medial myocutaneous flap or skin graft suffices. In advanced cases, such as grade III, involving the medial side of both upper and lower eyelids, and grade IV, with diffuse lesions involving both medial and lateral sides of the upper and lower eyelids, uncapping surgery, local flaps, and skin grafts are appropriate.7 However, excising larger XP lesions can increase the risk of complications such as eyelid retraction, ectropion, and altered pigmentation, necessitating reconstruction with a skin graft or flap to prevent these issues. Out of all the surgical procedures, the most common surgical method is full-thickness skin excision.8 Since we only included Grade I lesions, we did not face any requirement for flaps or grafts.
The combined complication and recurrence rates are reported to be 0.5%.9 However, the recurrence rate is variable in surgical modalities, ranging between 0 and 37%.7,10,11 Recurrence associated with surgical modalities is seen in the following scenarios:
(b) Involvement of deeper layers, specially infiltration of muscle
(c) Wrong choice of surgery as simple excision in Grade II or III lesions
(d) Underlying uncontrolled hypercholesterolemia.
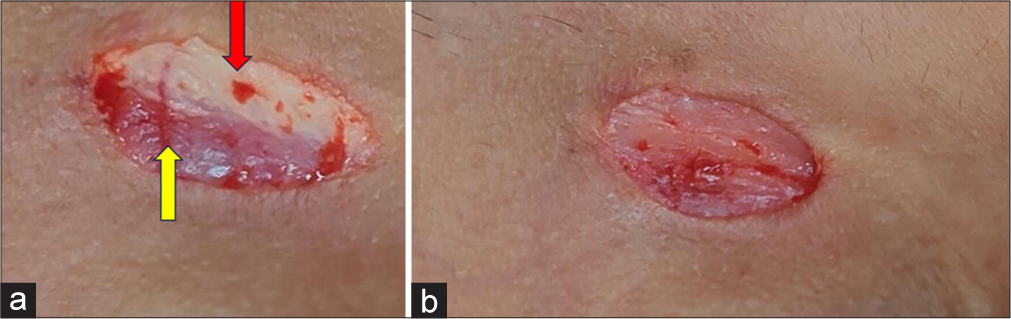
- (a) Incomplete excision of xanthelasma with the xanthelasma palpebrarum component (red arrow) lying on top of orbicularis oculi muscle (yellow arrow). If the lesion is closed at this stage there is a high chance of recurrence. (b) Complete excision of xanthelasma that reduces the chance of recurrence.
We did not notice any recurrence in the 6-month follow-up period in either group of patients.
While many studies have been done on various surgical modalities, ours is the first study wherein we have measured the angular defect associated with simple excision of a Grade I XP lesion that involves the upper lid crease. We also noticed that, Grade I lesions which were away from the lid crease, did not lead to any such angular defect [Figure 5]. The average angular defect associated with simple excision was 143.9°.
Choi et al. also reported similar angular defects without calculating the real values of deformity.4 They suggested a complicated procedure to attenuate this deformity in which, after the complete removal of tissue, the orbicularis oculi musculocutaneous flap was extensively elevated across the entire upper eyelid, prioritizing the lateral flap first. The medial and lateral flaps were separated by the excision line of the lesion, diverging from the traditional blepharoplasty incision line. If excessive tension occurred after advancing the lateral flap to repair the defect, the medial flap was then elevated. The procedure, though successful, holds good for rarer grade II and III lesions.
We also observed that even with simple excision of the Grade I XP lesion not involving the upper lid crease, there was no angular deformity or lateral hooding [Figure 6].
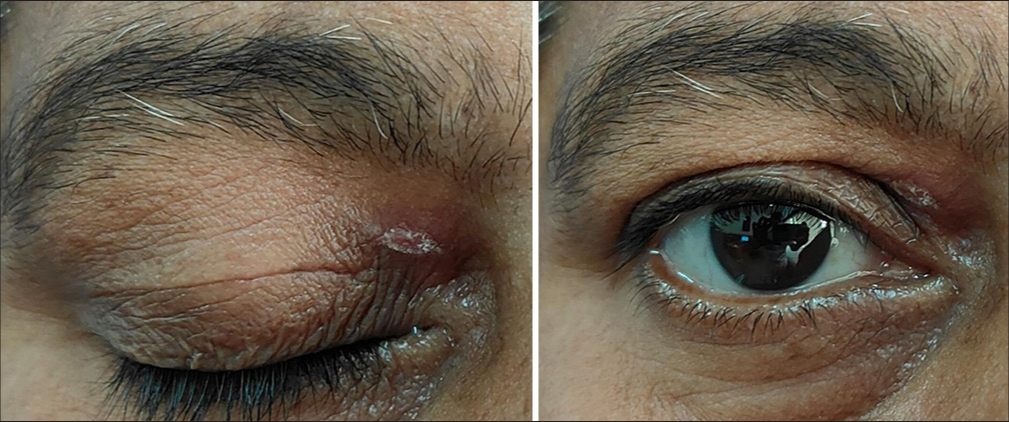
- When the xanthelasma does not touch the upper lid crease, no angular defect is formed even with simple excision.
For a more common Grade I lesion, we suggest an extension of the excisional margin till the lateral canthus of the eye and the width of the excision are the same as the maximum width of xanthelasma. The incision is tapered at both medial and lateral ends. Although most authors use continuous sutures, we achieved good results with interrupted sutures. The importance of the pinch test cannot be emphasized more before the procedure. We conducted a pinch test at three sites: At the maximum width of xanthelasma, center of excision (Usually 10 mm above the upper lid in most cases), and at the lateral border. The pinch test is usually done in a sitting position but we conducted it in the supine position to eliminate the effect of gravity, however small that be.
In terms of adverse effects, the downtime was more in patients of Group B. Swelling and contusion were also more commonly associated with the extension of incision till lateral canthus. However, the angular deformity was greatly reduced to absent in group B patients.
Drawbacks
The procedure wherein we have extended the excision till the level of lateral canthus holds good only for Grade I lesions. In cases where deeper layers are involved and lesions extend beyond the medial canthus, other procedures such as Myo cutaneous flaps and grafts, need to be utilized. The patients need to be followed up for a longer duration to rule out any possibility of recurrence.
CONCLUSION
The result of this study shows that simple excision of Grade I XP involving upper lid crease can lead to lateral hooding and angular defect. A simple way to reduce or eliminate this defect is to extend the excision till the level of lateral canthus. If the surgical excision is done properly without leaving any remnants of fat, the chance of recurrence is almost negligible. A pinch test is a must before removing any portion of the lid to avoid permanent defects such as ectropion.
Authors’ contributions
Dr(s) Siddharth Mani, Manish Khandare, YVK Chaitanya, Aradhana Raut, Shekhar Neema, Gopalsingh Rameshsingh Rajput and Eeshan Ranjan had full access to all of the data in the study and take responsibility for the integrity and accuracy of the data. Study concept and design: Dr Siddharth Mani. Acquisition, analysis, and interpretation of data: Dr(s) Siddharth Mani, Manish Khandare, YVK Chaitanya, Aradhana Raut, Shekhar Neema, Gopalsingh Rameshsingh Rajput and Eeshan Ranjan. Drafting of the manuscript: Dr(s) Siddharth Mani, Manish Khandare, YVK Chaitanya, Aradhana Raut, Shekhar Neema, Gopalsingh Rameshsingh Rajput and Eeshan Ranjan. Critical revision of the manuscript for important intellectual content: Dr(s) Siddharth Mani, Manish Khandare, YVK Chaitanya, Aradhana Raut, Shekhar Neema, Gopalsingh Rameshsingh Rajput and Eeshan Ranjan.
Ethical approval
The research/study approved by the Institutional Review Board at INHS Sanjivani, number 17/23, dated 02nd January 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Risk of non-alcoholic fatty liver disease in xanthelasma palpebrarum. J Inflamm Res. 2021;14:1891-9.
- [CrossRef] [PubMed] [Google Scholar]
- Skin manifestations of hypothyroidism-a clinical study. IOSR J Dent Med Sci. 2013;7:58-60.
- [CrossRef] [Google Scholar]
- Outcomes of surgical management of xanthelasma palpebrarum. Arch Plast Surg. 2013;40:380-6.
- [CrossRef] [PubMed] [Google Scholar]
- A modified surgical method combined with blepharoplasty design for treatment of xanthelasma palpebrarum. Biomed Res Int. 2020;1:4803168.
- [CrossRef] [PubMed] [Google Scholar]
- Necrobiotic xanthogranuloma. J Cutan Aesthet Surg. 2012;5:43-5.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of xanthelasma by excision with secondary intention healing. Clin Exp Dermatol. 1996;21:273-5.
- [CrossRef] [PubMed] [Google Scholar]
- Operative treatment of large periocular xanthelasma. Orbit. 2009;28:16-9.
- [CrossRef] [PubMed] [Google Scholar]
- Xanthelasma palpebrarum: An oculoplastic viewpoint of optimal treatment. Adv Ophthalmol Optom. 2021;6:341-56.
- [CrossRef] [Google Scholar]
- A practical review of the management of xanthelasma palpebrarum. PRS Global Open. 2023;11:e4982.
- [CrossRef] [PubMed] [Google Scholar]
- A new operative method for treatment of xanthelasma or xanthoma palpebrarum: Microsurgical inverted peeling. Plast Reconstr Surg. 1998;102:1171-4.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of large xanthelasma palpebrarums with full-thickness skin grafts obtained by blepharoplasty. J Cutan Med Surg. 2013;17:197-200.
- [CrossRef] [PubMed] [Google Scholar]






