Translate this page into:
Tangential Excision of Rhinophyma with the Disposable Razor Blade: Simple and Cost Efficient with Aesthetically Good Results
Address for correspondence: Dr. Marcus Kiehlmann, Department of Plastic and Aesthetic Surgery, Reconstructive and Hand Surgery, AGAPLESION Markus Hospital Frankfurt, Wilhelm-Epstein-Straße 4, 60431 Frankfurt am Main, Germany. E-mail: marcus.kiehlmann@fdk.info
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Medical therapies for rhinophyma have been described but these only delay progression. Therefore, surgery is the method of choice. Plenty of modalities have been described including cold-knife surgery, electrosurgery, hydrosurgery, laser-assisted treatments, and dermabrasion.
Settings and Design:
In this two-center study, patients’ charts and photodocumentation were analyzed retrospectively.
Materials and Methods:
Surgery was performed under general anesthesia with an additional local anesthesia of the affected areas of the nose. We removed the hypertrophic tissue in thin layers with a sterile disposable razor blade under constant visual control of the underlying cartilage and adnexal structures. A dressing with Mepithel and gauzes was applied. Patients presented weekly to monitor the wounds. Follow-up was 1 year.
Results:
From 2016 to 2019, nine male patients with rhinophyma underwent surgical therapy at AGAPLESION Markus Hospital, Frankfurt am Main, Germany and at the Department of Plastic, Reconstructive and Aesthetic Surgery, Innsbruck Medical University, Austria. The mean age of the patients was 66 years. Mean time to complete re-epithelization equaled 31.5 days. No recurrences were noted within the follow-up period of 1 year. Patients’ satisfaction was very high. Only one patient had hypertrophic scars at the wing of the nose and another one developed a superficial fistula without connection to the nasal cavity.
Conclusion:
To the best of our knowledge, this is the first case series describing the use of a disposable razor blade for rhinophyma treatment supporting its efficiency described in previous anecdotal publications. We can highly recommend the technique, as it is cost-efficient and simple and provides excellent aesthetic results.
Keywords
Razor blade
rhinophyma
tangential excision
Rhinophyma is a benign disease that afflicts mostly males in their 50th–70th decade. Surgical therapy in rhinophyma includes various techniques and devices. We would like to report on our experience with the tangential excision with a disposable razor blade. Nine patients were treated within 3 years. The use of a disposable razor blade in the surgical treatment of rhinophyma is inexpensive, easy, and yields excellent aesthetic results.

INTRODUCTION
Rhinophyma is a benign disease that commonly affects males who are in the fifth to seventh decade of life. The noninfiltrative disease is limited to the skin tissue and preserves the underlying bone and cartilage. Its exact pathogenesis is still unclear. When examining the tissue-histopathology, two types can be described: a hypertrophic sebaceous form and a fibrous form with telangiectasias. Mostly patients consult a doctor due to functional airway obstruction or aesthetic issues related to the hypertrophic tissue. Surgery to remove the proliferating tissue is recommended, not only to re-define the shape of the nose but also as there have been reports of incidental basal cell carcinomas up to 10%.[1]
The first attempts to treat this disfiguring tumor of the nose were carried out in 1845.[2] From then on several techniques have developed including electrosurgery, laser therapy, water-assisted debridement, dermabrasion, and excision by scalpel. In our study, we report on our results with the removal of the rhinophymatous tissue by using a disposable razor blade.
SUBJECTS AND METHODS
Inclusion criteria
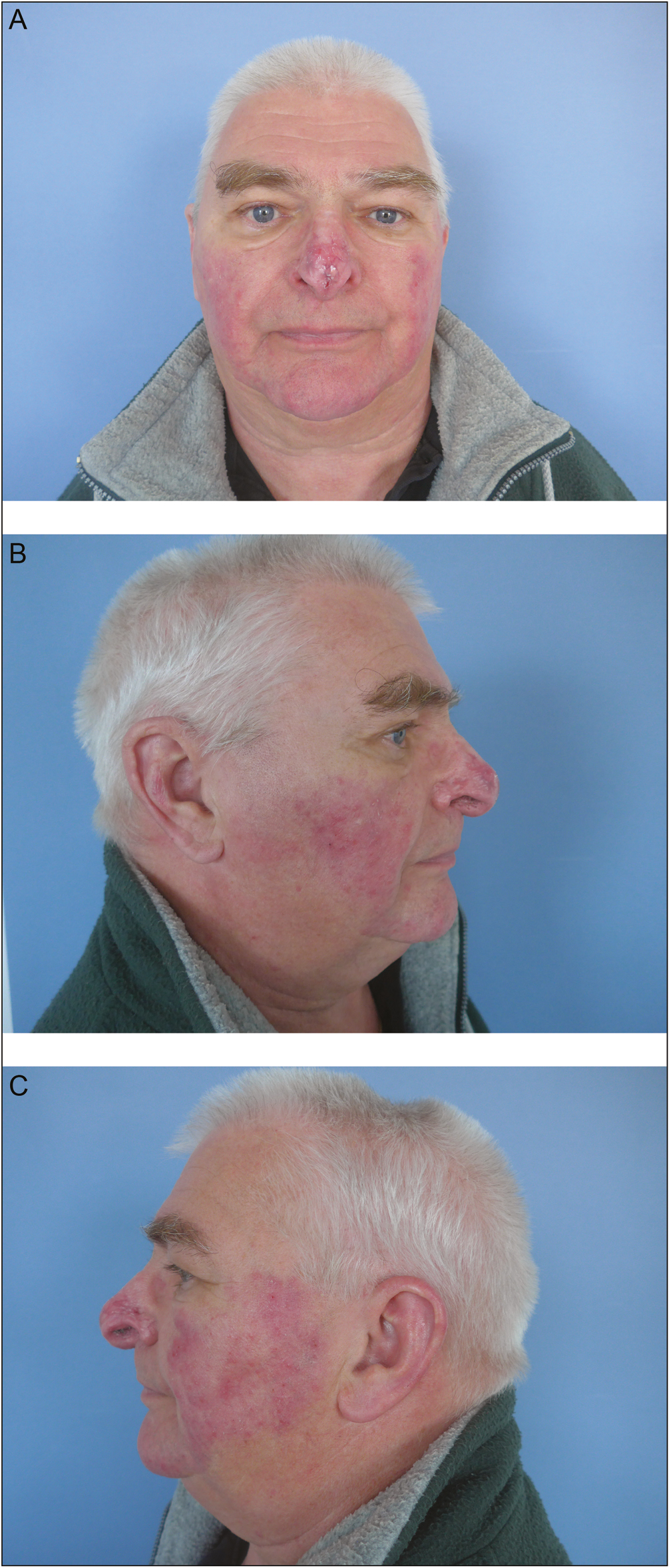
All patients treated for rhinophyma between 2016 and 2019 at the Department of Plastic and Aesthetic Surgery, Reconstructive and Hand Surgery at AGAPLESION Markus Hospital, Frankfurt am Main, Germany and at the Department of Plastic, Reconstructive and Aesthetic Surgery at Innsbruck Medical University, Austria were identified and patient charts, including photodocumentation were analyzed retrospectively. Only patients that were treated using a disposable razor blade were included in the study. All patients have given their written informed consent. Approval by the ethics commission was not required as the treatment of rhinophyma with the disposable razor blade is an already described surgical method among other modalities. Figure 1A and B shows a typical rhinophyma patient, who presented to our clinic and sought medical advice.

- (A) Frontal view preoperatively. (B) Lateral right view preoperatively
Surgical technique
Surgery was performed under general anesthesia. In addition, a local block of the infraorbital nerve as well as local infiltration of the affected area of the nose with Xylonest 1% with adrenaline was administered analogously to the wide-awake approach in hand surgery. A sterile disposable razor blade was used to perform the tangential excision of the hypertrophic tissue [Figure 2A–C]. The razor blade was sterilized using low thermal methods such as plasma sterilization or gamma radiation as common steam sterilization puts damage to the plastic material. The rhinophymatous tissue was removed in thin layers under constant visual control to preserve the underlying cartilage and adnexal structures. We put much importance on the complete removal of all tumorous tissue to prevent recurrences and on re-defining the anatomic and aesthetic subunits of the nose. At the delicate areas of the nasal wings we stabilized the tissue by putting a fingertip in the nostril. We obtained specimen for histopathological examination. Punctual hemostasis was done by bipolar cautery in selected areas. We applied a dressing consisting of one layer of Mepithel and gauzes. The dressing was not removed within the first week. Postoperative care included weekly presentations at our clinic to monitor the wounds and to change the dressing. Follow-up was 1 year.

- (A) Intraoperative view and lateral right view before excision. (B) Intraoperative view with disposable razor blade. (C) Intraoperative view and lateral left after tangential excision
RESULTS
From 2016 to 2019, nine patients underwent surgical treatment of rhinophyma at AGAPLESION Markus Hospital and Innsbruck University Hospital. The median age was 66 years (range 46–86 years). All patients were male. Median time of surgery equaled 31 min (range 8–48 min). The overall intraoperative blood loss was low, approximately 5–10 mL. During the shaving procedure, there was more bleeding, but it was well manageable with punctual hemostasis using electrocautery. All patients were treated in a single session. The histopathological examination of the specimens showed typical rhinophymatous tissue in all cases and no evidence of malignant formation. Rhinophyma is considered the last stage of chronic acne rosacea. Time to complete re-epithelialization equaled 31.5 days on average (range 8–42 days) [Figures 3 and 4A–C]. Within the follow-up period of 1 year no recurrence was noted [Figure 5A–C]. In two patients we observed postoperative complications. One patient developed a hypertrophic scarring but refused a surgical correction as he was satisfied with the result and in another patient a small superficial fistula was observed, which was corrected in an outpatient setting under local anesthesia. In general, all patients showed high satisfaction with the cosmetic result.

- One month postoperative, frontal view
- (A) Two months postoperative, frontal view. (B) Two months postoperative, lateral right view. (C) Two months postoperative, lateral left view
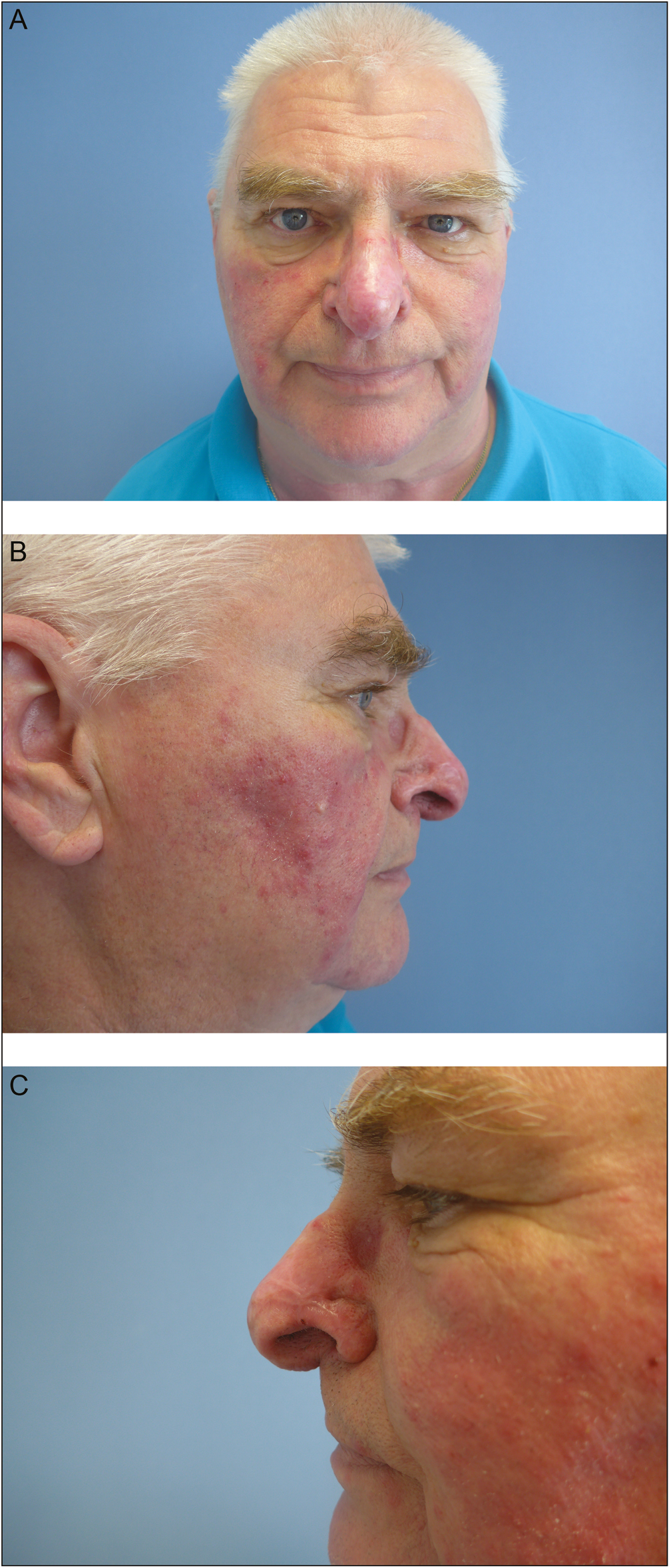
- (A) One-year postoperative, frontal view. (B) One-year postoperative, lateral right view. (C) One-year postoperative, lateral left view
DISCUSSION
Pharmacological treatments are not completely successful, as they only delay progression.[3] Conclusively, surgical treatment is the method of choice. There are plenty of techniques to physically destruct the tumorous tissue. Therapies by scalpel excision, dermabrasion, cryosurgery, laser surgery, electrosurgery/electrocautery, and water-assisted debridement have been described in the past years and decades. As Sadick et al.[3] stated in their review, the first attempts in surgical resection of rhinophyma were made in 1845 by Dieffenbach.[2] He described an excision by cross or elliptoid cuts in a vertical and horizontal direction and primary wound closure.[3] A common problem of the cold excision is poor control over hemostasis. Therefore, electrocautery is mostly needed in all treatment modalities to control bleeding and to make it easier to judge the depth of the tissue removal.
A study by Lazzeri et al.[4] with 76 included patients, of which 45 were treated with tangential excision compared to 22 patients that underwent laser therapy found that both methods create satisfying results. In the questionnaire, patients were given after the procedure, rates of high satisfaction were 85% in the group where tangential excision was performed compared to 84.1% in the carbon dioxide laser group.[4] A total of 18 male patients treated with carbon dioxide laser also showed good cosmetic results with very low blood loss (average 3.3 mL) in the study of Ali and Streitmann.[5] In their hands, the CO2 laser is a safe and effective method with few complications. In 1 patient a nasocutaneous fistula was reported that was managed conservatively and closed spontaneously 1 month later. However, the time to re-epitheliazation lasted at least 28 days and an average time of 40.1 days. The costs for laser surgery are yet high and more time-consuming. In a comparison between CO2 laser and electrosurgery it was found that laser surgery took twice as long as electrosurgery and that the initial cost of instrumentation of laser is 15 to 20 times higher than those of electrosurgery.[6]
In 2006, a new method was described, namely the treatment of rhinophyma with the Versajet hydrosurgery system (Smith and Nephew, UK). This system has been used before in the treatment of chronic wounds and burns. The surgeon performs the procedure with a handpiece where a thin stream of sterile saline creates a suction effect. The device is based on the Venturi effect. It is described as precise method to remove the tumorous tissue while preserving sufficient tissue for re-epithelialization and avoiding damage to the cartilaginous structures of the nose. Re-epithelization was complete by 4 weeks and after a follow-up of 1 year no recurrence was reported. There were no postoperative complications in the 6 patients treated with Versajet in this study.[7] However, the costs of the device and the handpieces are very high.[78]
The technique of using a disposable razor blade was first described by Fishman et al.[9] They reported that it was excellent for refining the shape and recontouring the nose. Moreover, Morandi et al.[10] from our group also described the tangential debridement with the razor blade in a case of a 55-year-old female patient in a case report with excellent postoperative results. The use of a disposable sterile razor blade and tangential excision is an easy to perform method with a device that is inexpensive and available in every setting. Our study supports the aesthetically pleasant results and easy handling that were already described in previous case reports in a larger series. The technique allows for precise tangential debridement preserving the underlying cartilage. The depth of the tissue can be precisely assessed, especially in the delicate areas of the alar wings and alar rim. It is an almost bloodless method––only punctual hemostasis with a bipolar diathermy is needed. Prior to surgery Xylonest 1% with adrenaline was injected in the tissue of the nose tip to reduce intraoperative bleeding. Analogous to its use in the wide-awake approach in hand surgery procedures we did not observe any necrosis of soft or skin tissue in the areas where adrenaline was injected. Time of surgery is very short with a mean of 31.5 min in our study. This is a definite advantage compared to more time-consuming therapies such as laser surgery. There is no or minimal damage to healthy tissue and heat damage is avoided completely as compared to electrosurgery. Removal of affected rhinophyma tissue is extensive and destruction of affected tissue is comprehensive, as we did not note any recurrence in 1 year of follow-up and, in addition, patient satisfaction is very high. Concerning the economic aspects, the costs of using a disposable razor blade are very low compared to the handpieces of the Versajet hydrosurgery system or a laser device, or the Ellman device. The procedure can be done in local anesthesia to lower the overall costs; however, in our experience, our German patients seem to prefer general anesthesia in surgical procedures in the facial region. In conclusion, we can highly recommend the excision of rhinophyma with a disposable razor blade.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Die operative Chirurgie. Vol 1. Leipzig, Germany: Brockhaus; 1845. p. :373.
- Rhinophyma: Diagnosis and treatment options for a disfiguring tumor of the nose. Ann Plast Surg. 2008;61:114-20.
- [Google Scholar]
- Surgical correction of rhinophyma: Comparison of two methods in a 15-year-long experience. J Craniomaxillofac Surg. 2013;41:429-36.
- [Google Scholar]
- Excision of rhinophyma with the carbon dioxide laser: A ten-year experience. Ann Otol Rhinol Laryngol. 1997;106:952-5.
- [Google Scholar]
- Comparison of CO2 laser and electrosurgery in the treatment of rhinophyma. J Am Acad Dermatol. 1988;18:363-8.
- [Google Scholar]
- Treatment of rhinophyma with the Versajet hydrosurgery system. J Plast Reconstr Aesthet Surg. 2008;61:330-3.
- [Google Scholar]
- “A close shave”: use of a disposable razor blade in the management of rhinophyma. BMJ Case Rep. 2008;2008:bcr0620080006. 10.1136/bcr.06.2008.0006. Epub 2008 Nov 20
- [Google Scholar]
- An old problem with a new solution: Cost-effective, easy correction of rhinophyma using a disposable razor. Arch Plast Surg. 2018;45:490-2.
- [Google Scholar]





