Translate this page into:
The Safety of Large-Amount Liposuction: A Retrospective Analysis of 28 Cases
Address for correspondence: Dr. Taghreed Alhumsi, Plastic Surgery Division, Surgery Department, King Saud University Medical City (KSUMC), King Saud University, Riyadh, Saudi Arabia. E-mail: drtag20@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Aim:
Our study aims to assess the safety of large amounts of liposuction in a new light.
Materials and Methods:
This is a retrospective review of patients who underwent large-volume liposuction from August 2020 to April 2021. Patient demographics, liposuction areas, the amount of infiltrate and aspirate, the surface area of liposuction areas, anesthesia duration, pain score after surgery, preoperative and 4-h postoperative hemoglobin, and basic metabolic panel (sodium, potassium, creatinine, urea) were measured.
Results:
Out of the 28 patients, 26 (92.85%) were females. The mean age was 37.1 years old. The mean preoperative hemoglobin was 13.73 g/dL. The average anesthesia time was 220.39 min. The average amount of liposuction infiltrated was 7.55 L, and the average amount of liposuction aspirate was 6.83 L. The mean hemoglobin 4 h postoperatively was 13.7 g/dL.
Conclusions:
With proper patient selection and a comprehensive physical exam with preoperative blood workup performed in an accredited facility with a highly experienced plastic surgeon and anesthesiologist, mega liposuction can be safely performed as a day surgery procedure.
Keywords
Body contouring
esthetic surgery
large-volume liposuction
lipoplasty
liposuction
Large-volume liposuction is safe with proper patient selection, and strict attention to the standard guidelines can ensure a satisfactory outcome and reduce the risk of morbidity and mortality

INTRODUCTION
Liposuction, also referred to as lipoplasty, is a surgical procedure that removes excess fat in specific body areas.[1] Liposuction is considered the most common procedure performed in esthetic surgery.[2] The safety of liposuction has evolved with time. Proper patient selection, perioperative monitoring, fluid management, and deep vein thrombosis prophylaxis have made the procedure safe, with less than 1.5% of complications.[23] As with many other surgical procedures, liposuction generally has minor complications, but some are life-threatening, representing 0.02% of total complications.[2] One of the most common minor complications includes seroma, hemoglobin drop, and contour irregulates, whereas the most significant complications are deep vein thrombosis and pulmonary embolism. The development of new anesthesia techniques, like the tumescent formula, made a breakthrough in esthetic surgery, enabling surgeons to safely aspirate considerable amounts of fat with decreased postoperative complications.[1]
According to the American Society of Plastic Surgery (ASPS), large-volume liposuction is defined as an aspirate volume greater than 5 L; according to the ASPS recommendations, there is no cutoff point in the liposuction amount. However, the 5-L aspirate amount was made as a clear point, which, if exceeded, leads to an increasing percentage of complications.[3] According to the literature, many surgeons have exceeded the 5-L cutoff point with no significant complications. It could be beneficial because of fat’s metabolic effect on the body.[456] With adequately selected candidates and an accredited facility with highly experienced anesthesiologists and plastic surgeons, large-volume liposuction can be safe and effective.[789] To the best of the author’s knowledge, this is the first research conducted in Saudi Arabia aimed at assessing the safety of large amounts of liposuction and postoperative outcomes.
MATERIALS AND METHODS
This retrospective chart review study was conducted after approval by the institutional review board. Inclusion criteria were all patients who underwent liposuction greater than 5 L from August 2020 to April 2021, with a body mass index (BMI) of less than or equal to 30 (kg/m2) without comorbidities such as cardiac, respiratory, or metabolic disease to avoid the confounding effect of these diseases. Our exclusion criteria were patients with comorbidities, those who had undergone less than 5 L of liposuction procedures, and those with a BMI of more than 30 (kg/m2).
Patients’ charts were reviewed for preoperative clinical history and postoperative outcomes. The data obtained include age, gender, BMI, area of liposuction, amount of liposuction infiltrate and aspirate, preoperative and postoperative hemoglobin, type of anesthesia, anesthesia time, postoperative pain score from 0 to 10, postoperative complications, and body surface area liposuction done.
RESULTS
Participants
Out of the 28 patients, 26 (92.85%) were females and two (7.15%) were males. Their ages ranged from 22 to 49 years old (the mean was 37.1 years old). Most of the included patients were under 40 years old (57.14%). The two male patients were 26 and 41 years old. Participants’ BMI ranged from 24 to 30 kg/m2 (mean = 28.90 kg/m2). The participants’ body surface area of liposuction ranged from 18% to 54% (with a mean of 39.8%). All the included patients had no chronic medical conditions. All patients had their hemoglobin checked preoperatively, and it was in the range of 11.8–16.2 g/dL (mean = 13.73 g/dL). All the included patient-related data are presented in Table 1.
| Case | Age | Sex | BMI (kg/m2) | Site of liposuction | AT (min) | Liposuction infiltrate (L) | Liposuction aspirate (L) | Preoperative hemoglobin (g/dL) | Postoperative hemoglobin (g/dL) | Body surface area (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | F | 29.4 | Abdomen/back/flank/arms | 180 | 8 | 6.3 | 12 | 10.3 | 54 |
| 2 | 35 | F | 30 | Abdomen/back/flank | 120 | 7 | 6 | 12.8 | 10.6 | 36 |
| 3 | 31 | F | 29.3 | Liposuction thigh | 120 | 8 | 7.4 | 13.3 | 11.2 | 18 |
| 4 | 38 | F | 28.5 | Abdomen/back/flank | 300 | 4.25 | 5.1 | 13.6 | 9.5 | 36 |
| 5 | 30 | F | 28.4 | Abdomen/back/flank | 180 | 7 | 6.4 | 14 | 11.4 | 36 |
| 6 | 49 | F | 25.56 | Abdomen/back/flank | 180 | 7 | 5.4 | 14.7 | 11.6 | 36 |
| 7 | 46 | F | 29 | Abdomen/chest/flank | 180 | 6 | 7.5 | 15 | 13.7 | 36 |
| 8 | 26 | M | 30 | Abdomen/chest/back/flank | 180 | 8 | 8.4 | 16.2 | 14.3 | 36 |
| 9 | 40 | F | 29.5 | Abdomen/back/flank/arms | 260 | 8 | 6.3 | 11.8 | 10.3 | 54 |
| 10 | 41 | F | 26 | Abdomen/back/flank | 210 | 7 | 6.6 | 12.5 | 10.9 | 36 |
| 11 | 36 | F | 27.1 | Abdomen/back/flank/arms | 240 | 8 | 6.5 | 12.5 | 10.2 | 54 |
| 12 | 44 | F | 30 | Abdomen/back/flank | 310 | 7 | 5.7 | 13.8 | 10.8 | 36 |
| 13 | 22 | F | 25.53 | Abdomen/back/flank | 202 | 7 | 6.7 | 14 | 11.2 | 36 |
| 14 | 35 | F | 30 | Abdomen/back/flank | 270 | 7 | 6.7 | 14 | 11.3 | 36 |
| 15 | 49 | F | 30 | Abdomen/back/flank/arms | 240 | 8 | 6 | 15 | 13.5 | 54 |
| 16 | 41 | M | 30 | Abdomen/back | 160 | 7 | 9.5 | 16 | 13.3 | 36 |
| 17 | 36 | F | 26.7 | Abdomen/back/flank | 190 | 7 | 5.6 | 12.6 | 11.4 | 36 |
| 18 | 40 | F | 30 | Abdomen/back/flank | 201 | 8 | 8.3 | 13.2 | 11.5 | 36 |
| 19 | 34 | F | 30 | Abdomen/back/flank | 210 | 6 | 6 | 13.3 | 10.4 | 36 |
| 20 | 34 | F | 24 | Abdomen/back/flank | 241 | 8.5 | 6.35 | 13.3 | 8.4 | 36 |
| 21 | 34 | F | 28.9 | Abdomen/back/flank | 286 | 8 | 8.1 | 13.7 | 10.6 | 36 |
| 22 | 40 | F | 29.9 | Abdomen/back/flank | 207 | 8.3 | 7.5 | 13.9 | 12.2 | 36 |
| 23 | 43 | F | 29 | Abdomen/back/flank | 206 | 12.5 | 8.3 | 14.6 | 10.7 | 36 |
| 24 | 37 | F | 29 | Abdomen/back/arms/flank | 203 | 8 | 6.5 | 14.8 | 10.7 | 54 |
| 25 | 34 | F | 25 | Abdomen/back/flank/arms | 240 | 7 | 6 | 15.1 | 11.4 | 54 |
| 26 | 32 | F | 27.5 | Abdomen/back/arms | 195 | 7 | 6.9 | 12.4 | 11 | 54 |
| 27 | 32 | F | 26.4 | Abdomen/back | 390 | 9 | 7.3 | 13 | 10 | 36 |
| 28 | 40 | F | 30 | Abdomen/back/flank | 270 | 8 | 8.1 | 13.5 | 12 | 36 |
AT = anesthesia time, BMI = body mass index
Intraoperative measures
All the patients were administered general anesthesia (100%) in our series, and the average anesthesia time was 221.17 min. Regarding the liposuction site, most of the patients had liposuction of the abdomen, back, and flanks (67.85%), followed by the abdomen, back, flanks, and arms (17.85%). This corresponded to the participants’ body surface area of liposuction ranging from 18% to 54% (mean = 39.8%). The amount of tumescent fluid infused ranged from 4.25 to 12.5 L (a mean of 7.55 L). On the other hand, the average liposuction aspirate was 6.83 L (ranging from 5.1 to 9.5 L) [Figure 1].
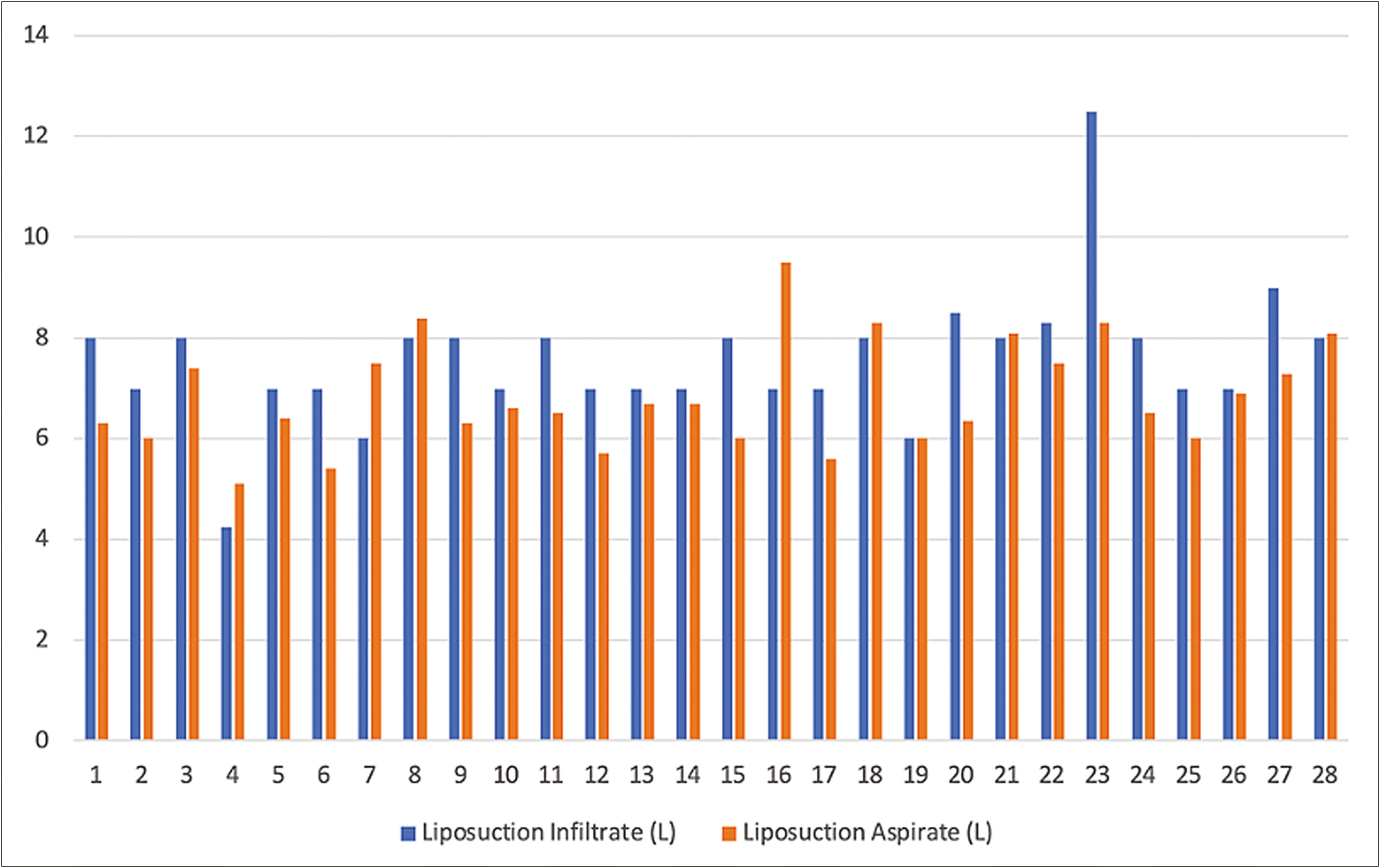
- The liposuction infiltrate and aspirate in liters of each patient
The average anesthesia time was 220.39 min (ranging from 120 to 390 min).
Postoperative measures
Postoperatively, all patients’ hemoglobin was checked 4 h after surgery, ranging from 11.8 to 16.2 g/dL (mean = 13.7 g/dL) [Figure 2].
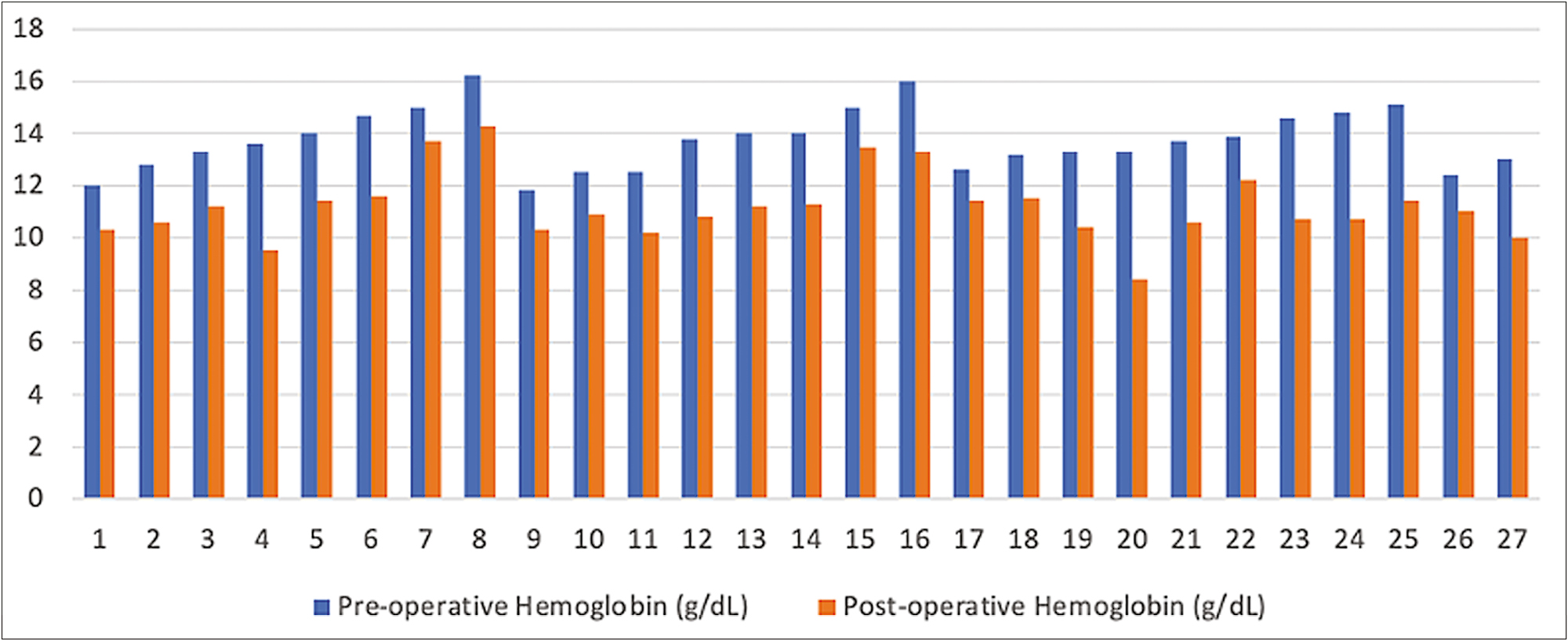
- The preoperative and postoperative hemoglobin of the included patients
All patients were assessed for pain. The pain score 4 h postsurgery ranged from 0 to 4 out of 10 (mean = 1.96). Regarding electrolyte measurements, all values were normal preoperatively and postoperatively. None of the included patients had any postoperative complications.
DISCUSSION
Liposuction, introduced as a surgical intervention for contouring distinct body parts, has grown in popularity as a total body sculpting intervention.[1] It has become popular among the general population and surgeons as a safe, noninvasive, and simple procedure for body contouring or sculpting procedure.[10] A study conducted in Egypt by Saleh et al. determined how far large-volume liposuction is considered effective and safe. They included 60 female patients. The mean amount of infiltrate was 3 L, with an average aspirate amount of 6 L.[1] A systematic review and meta-analysis included 3583 patients with an average aspirate amount of 7.7 L, with the highest reported aspirate amount of 25 L.[11]
consequently, in our article, we have conducted a chart review of patients who underwent large-volume liposuction, removing up to 9.5 L of fat, with an average amount of 7.55 L infiltrated and an average aspirated amount of 6.83 L. Our results and those of several other published articles have pointed to the same average amount of infiltration and aspiration.[7121314] Liposuction can be done using a local, regional, or general anesthetic. There has not been any evidence that one anesthetic approach is better than another. The type of anesthetic used is determined by the location and extent of liposuction and the patient’s preferences.[15] The anesthetic approach depends on the areas being operated on, such as the arms, thighs, abdomen, or buttocks, and the amount of liposuction accomplished. Because liposuction is done under general anesthesia as a daycare procedure, it is critical that patients’ psychomotor and cognitive functions recover quickly, allowing them to be discharged sooner.[16] When dealing with a large amount of liposuction or if the patient desires, the most recommended type of anesthesia is general anesthesia.[17] A recent study conducted by cuenca-Pardo reported a patient who underwent a large amount of liposuction and was complicated by sudden death due to fat embolism with an anesthesia time of 198 min.[18] In our series, all the patients who underwent surgery were under general anesthesia (100%) with an average anesthesia time of 221.17 min. None of the included patients had any postoperative complications.
In a study conducted by Kaoutzanis et al., the recommended guideline for large-volume liposuction fluid resuscitation is to use maintenance fluid, subcutaneous wetting solution, and 0.25 cc of intravenous crystalloid per cc of aspirate removed after 5 L.[19] However, these recommendations do not take the place of competent clinical judgment. Good communication between the surgeon and the anesthesiologist is essential in providing the patient with the best possible care and safety. All of our patients recovered well and were discharged home on the same day as day cases with no significant anesthesia-related complications.
Because the local anesthetic provides pre-emptive analgesia in tumescent liposuction, the need for analgesics during the procedure and afterward is limited.[16] Our results can explain this as the mean pain score postoperatively was 1.96 out of 10 (ranged from 0 to 4). In addition, the length of analgesia obtained from tumescent lidocaine can be increased by many hours by adding epinephrine to it. Nonsteroidal anti-inflammatory drugs were administered for postoperative pain treatment among our patients.
According to the published literature, the possibility of complications postliposuction ranges from 0% to 10%, with variations in the reported data between different disciplines, making a clear assessment of the risk profile of cosmetic surgery liposuction difficult.[17] The use of tumescent liposuction has become the standard gold technique of liposuction. In 2016, a survey of 127,961 participants who had liposuction in the United States revealed a 0.9% rate of complications.[1220] No death has occurred because of tumescent liposuction in ambulatory centers.[21] Among our data, we had no complications or adverse effects from large-volume liposuction. However, according to a recently conducted systematic review and meta-analysis by Kanapathy et al., significant complications in large-volume liposuction were 3.35%, of which blood loss requiring transfusion was the most common (2.89%). Of those patients that received a blood transfusion, 83.33% received an autologous blood transfusion.[12] In another study conducted in Egypt, among 60 female patients who had large amounts of liposuction in different body areas, no blood transfusion was needed postoperatively for any of their cases.[1] On 120 consecutive patients, Alegría Perén et al. completed a large amount of 8 L of liposuction and more for entire body contouring without the requirement of a transfusion of blood.[22] These two findings agree with ours, as in none of the included cases, a blood transfusion was required after surgery, with the minimum hemoglobin being 11.8 g/dL, with a mean of 13.7 g/dL. We believe that the minimized blood loss, which is established due to the time allowed for the tumescent solution prior to liposuction, along with increasing the amount of infiltrating, is a key to fewer complications regardless of the aspirate amount.
During the 4-month postsurgery period, a large amount of liposuction leads to considerable pulse rate and blood pressure reductions.[1523,24] This is due to the drop in hemoglobin postoperatively, which causes metabolic changes and salutary physiological adjustments secondary to enhanced insulin sensitivity and loss of weight. The insulin level in the blood has formerly been implicated as a significant influence on blood pressure and can predict subsequent heart dysfunction.[242526] None of the included patients had hemoglobin drop immediately postoperatively, and there was no change in electrolytes. All patients were followed up to 6 months postoperatively, and they were in stable condition; therefore, the hemoglobin level test was not repeated. According to our results, hemoglobin drop showed to be unrelated to the amount of aspirate. It was more crucial to choose suitable patients. However, this finding is explained because our patient population had no chronic medical conditions. Patients known to have comorbidities were well documented in the literature to have a higher risk of complications and morbidity.[25]
Limitations
To the best of the author’s knowledge, this is the first research of its kind conducted in Saudi Arabia. The main limitation faced is that this is a single-center retrospective chart review. Hence, we recommend prospective studies with a broader spectrum of a sample size to analyze all the variables in compliance with the estimate of liposuction. Inclusion criteria may include patients with comorbidities such as controlled diabetes and hypertension in the future. In addition, to determine the most appropriate pain protocol and management, we recommend conducting future studies to assess the pain score at different intervals, such as 12 and 24 h after surgery. Also, an accurate estimation of intravenous fluid used.
In conclusion, this single-center retrospective study of patients who underwent a large amount of liposuction showed that proper patient selection and strict attention to the standards and guidelines ensure a satisfactory outcome and reduce the risk of morbidity.
Financial support and sponsorship
Nil.
conflicts of interest
There are no conflicts of interest.
Acknowledgement
This work was supported by the college of Medicine Research center, Deanship of Scientific Research.
References
- Safety and benefits of large-volume liposuction: A single center experience. Int Arch Med. 2009;2:4.
- [Google Scholar]
- Optimizing patient outcomes and safety with liposuction. Aesthet Surg J. 2019;39:66-82.
- [Google Scholar]
- 2015. American Society of Plastic Surgeons. Available from: https://www.plasticsurgery.org/news/press-releases/how-much-liposuction-is-safe-the-answer-varies-by-body-weight#:~:text=There’s%20a%20long%20history%20of,a%20higher%20risk%20of%20complications.
- Influence of large-volume liposuction on metabolic and cardiovascular health: A systematic review. Ann Plast Surg. 2017;79:623-30.
- [Google Scholar]
- Safe total corporal contouring with large-volume liposuction for the obese patient. Aesthet Plast Surg. 2006;30:574-88.
- [Google Scholar]
- Large-volume liposuction: A review of 631 consecutive cases over 12 years. Plast Reconstr Surg. 2001;108:1753-63. discussion 1764-7
- [Google Scholar]
- Major and lethal complications of liposuction: A review of 72 cases in Germany between 1998 and 2002. Plast Reconstr Surg. 2008;121:396e-403e.
- [Google Scholar]
- Evaluation of the J-plasma electrosurgical device combined with nebulized collagen for burn healing in rodents. Plasma Med. 2018;8:365-77.
- [Google Scholar]
- Safety and benefits of large-volume liposuction: A single center experience. Int Arch Med. 2009;2:4.
- [Google Scholar]
- Unfavourable outcomes of liposuction and their management. Indian J Plast Surg. 2013;46:377-92.
- [Google Scholar]
- Safety of large volume liposuction in aesthetic surgery: A systematic review and meta-analysis. Aesthet Surg J. 2021;41:1040-53.
- [Google Scholar]
- The role of subcutaneous infiltration in suction-assisted lipoplasty: A review. Plast Reconstr Surg. 1997;99:514-9. discussion 520-6
- [Google Scholar]
- Large-volume liposuction: A review of 631 consecutive cases over 12 years. Plast Reconstr Surg. 2001;108:1753. discussion 1764
- [Google Scholar]
- cosmetic liposuction: Preoperative risk factors, major complication rates, and safety of combined procedures. Aesthet Surg J. 2017;37:680-94.
- [Google Scholar]
- Safety of aesthetic surgery in the overweight patient: Analysis of 127,961 patients. Aesthet Surg J. 2016;36:718-29.
- [Google Scholar]
- Large-volume circumferential liposuction with tumescent technique: A sure and viable procedure. Plast Reconstr Surg. 1999;104:1887-99.
- [Google Scholar]
- Total corporal contouring with mega-liposuction (120 consecutive cases) Aesth Plast Surg. 1999;23:93-100.
- [Google Scholar]
- Improvements in cardiovascular risk profile with large-volume liposuction: A pilot study. Plast Reconstr Surg. 2001;108:510-9. discussion 520-1
- [Google Scholar]
- [Liposuction does not heal diabetes and improve arterial risk factors] Duodecim. 2004;120:2480. author reply 2481
- [Google Scholar]
- Persistent elevation of plasma insulin levels is associated with increased cardiovascular risk in children and young adults. The Bogalusa Heart Study. circulation. 1996;93:54-9.
- [Google Scholar]
- The interrelationship between impaired glucose tolerance and other risk factors for cardiovascular disease: Is it a predictor for cardiovascular disease? J clin Epidemiol. 1994;47:485-93.
- [Google Scholar]





