Translate this page into:
Thread Lifting of the Jawline: A Pilot Study for Quantitative Evaluation
Address for correspondence: Dr. Alberto Diaspro, Rigeneralab Centre for Regenerative Medicine, Corso Unione Sovietica 159/a, 10134, Turin, Italy. E-mail: info@albertodiaspro.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Introduction:
The facial aging process produces changes that are characteristic of the superficial and deep fat framework and skin layers. Subdermal suspension with threads enables the sagging tissues to be lifted by means of a minimally invasive, closed procedure without surgical dissection. This observational study has been carried out on the basis of standardized tridimensional photographic analysis and measurement, aimed at determining objective, repetitive, and reliable evaluation of the soft tissue suspension technique.
Materials and Methods:
Eight participants were enrolled in this pilot study presenting with mild to moderate ptosis of the jawline tissues. Patient photographs were taken before (t0), immediately after threads implantation (t1), and at the following visit (t2). Each image captured before thread insertion was registered by the software and surface linear lengths in between the mentioned points were calculated.
Results:
The result showed an overall average improvement in the “tragus-to-marionette distance” (C-A) and the “tragus-to-jowl distance” after a mean follow-up time of 8.16 months (t0-t2). All analyzed parameters improved significantly (P < 0.05) at t1 and at t2 with respect to t0.
Conclusions:
This pilot study suggest that facial tissue suspension by means of poli-lactic/poli-caprolactone threads is safe and effective in treating skin flaws that affect mild-to-moderate ptosis of the jawline up to 8 months.
Keywords
Jawline
quantitative evaluation
threads
INTRODUCTION
The facial aging process produces changes that are characteristic of the superficial and deep fat framework and skin layers.
The breakdown of collagen and elastic fibers takes place, causing a noticeable weakening in prominent facial regions such as the cheeks, mandibular line, and neck; the dermatochalasis of facial and neck soft tissues accounts for the distinctive signs of facial aging.[1]
The introduction of a subdermal suspension with threads enables the sagging tissues to be lifted by means of a minimally invasive, closed procedure.[2] Its effectiveness is related to the focal nature of soft tissue ptosis, a procedure by which facial layers are mobilized without surgical dissection.
The limited morbidity and short downtime of these nonsurgical procedures resulted in practitioners and patients seeking less invasive modalities to achieve face tissue suspension, which guarantees acceptable longevity.
To the best of the authors’ knowledge, published reports about the efficacy and longevity of thread lifting are merely based on nonstandardized photographic assessment and self-related questionnaires addressed to patients, even during long follow-up periods of large patient groups and after a statistical evaluation of the results.[345] The resulting treatment indications and patient selection recommendations are, therefore, quite broad.[67]
This observational study has been carried out on the basis of the routine assumption that cosmetic procedures are very subjective and, beyond the mere judgment of patients and clinicians, is thus strongly recommended to bridge the gap in facial aging treatment.
The authors of this article aim at determining, by standardized tridimensional photographic analysis and measurement, the outcome of thread lifting of the jawline as this is the first study providing an objective, repetitive, and reliable evaluation of the soft tissue suspension technique.
MATERIALS AND METHODS
Patient population
Between January 2017 and July 2018, eight participants were enrolled in this study: six women and two men. Men were aged between 49 and 58 years (mean age 53.5 years), whereas women were aged between 48 and 68 years (mean age 57.5 years).
Participants were asked to maintain the same skin care regimen throughout the study and four weeks before baseline, as well as to adhere to study procedures and attend all sessions within the timeline of the study.
The study protocol followed the ethical guidelines of the Declaration of Helsinki, and the informed consent form (ICF) for the treatment was acquired from all patients.
Exclusion criteria included any treatment in the one year before baseline, including
facial soft tissue filler,
ultrasound technology and/or radiofrequency on the face or neck, and
botulinum toxin A injections in the lower face or neck
for the next year after thread insertion.
Technique
The enrolled participants were treated with bidirectionally barbed suspension threads, made by a copolymer of 70% poli-L-lactic acid (PLLA) and 30% poli-caprolactone (PCL) [Figure 1].
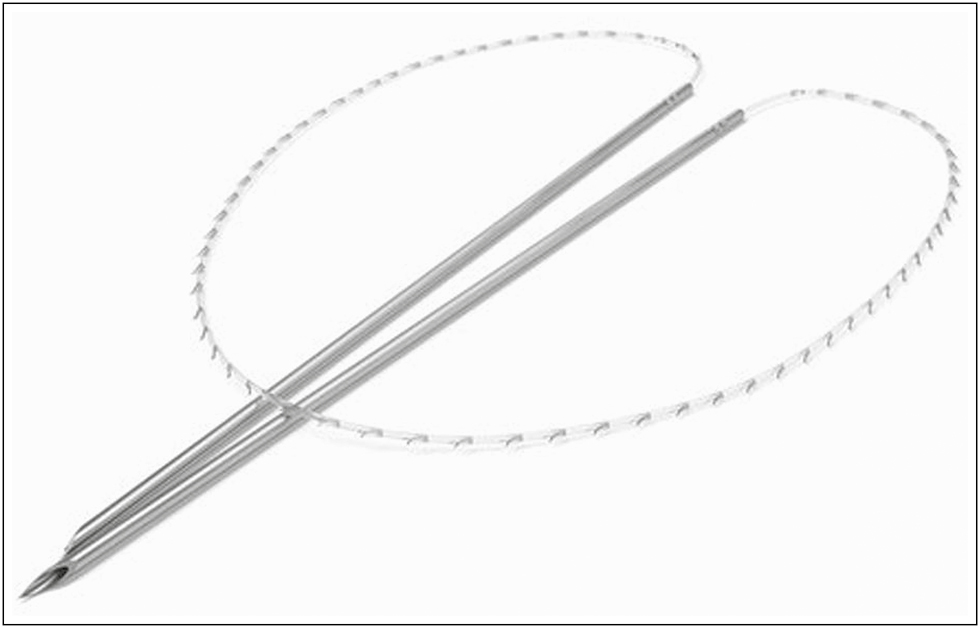
- The implanted Aptos Light Lift Thread 2G suspension thread with monodirectional barbs, made by a copolymer of 70% poli-L-lactic acid (PLLA) and 30% poli-caprolactone (PCL)
After proper disinfection with iodopovidone 10% in water was carried out, local anesthesia of the skin of the mandibular line was administered by subcutaneously injecting a solution of lidocaine 2% with epinephrine 1:100000 by an 80-mm blunt tip 23G cannula from an insertion point open by an 18G 40 mm needle in the pre-tragal area down to the jowls. After a 15-min expectation to obtain proper vasoconstriction of the superficial vessels of the jawline, a thread fixed on a couple of 10-cm needles was inserted into the pre-tragus at the Articularis (Ar) point, named as point C in the current study; the first needle was then pushed horizontally into the subcutaneous fat of the parotid-masseteric region toward the marionette line origin.
The exit point of this needle could be outlined below the Cheilon (Ch), named as point A in the current study; it is not recommended to insert the thread precisely at this landmark, as the underlying modiolus is noticeably a fixed structure.
The second needle was, therefore, pushed downward along the inferior border of the mandible in the same subcutaneous layer, toward the area of the mandibular ligament, topographically identified as the marionette line.
The ideal exit point lies at the lowest border of the jowl, named as point B in the current study. In current literature, this point refers to any anatomical landmark related to description of the jowl, as its formation is the result of an aging process and facial tissue ptosis, which is characterized by a lot of interobserver difference.
The following reference points were, therefore, taken as described [Figure 2]:
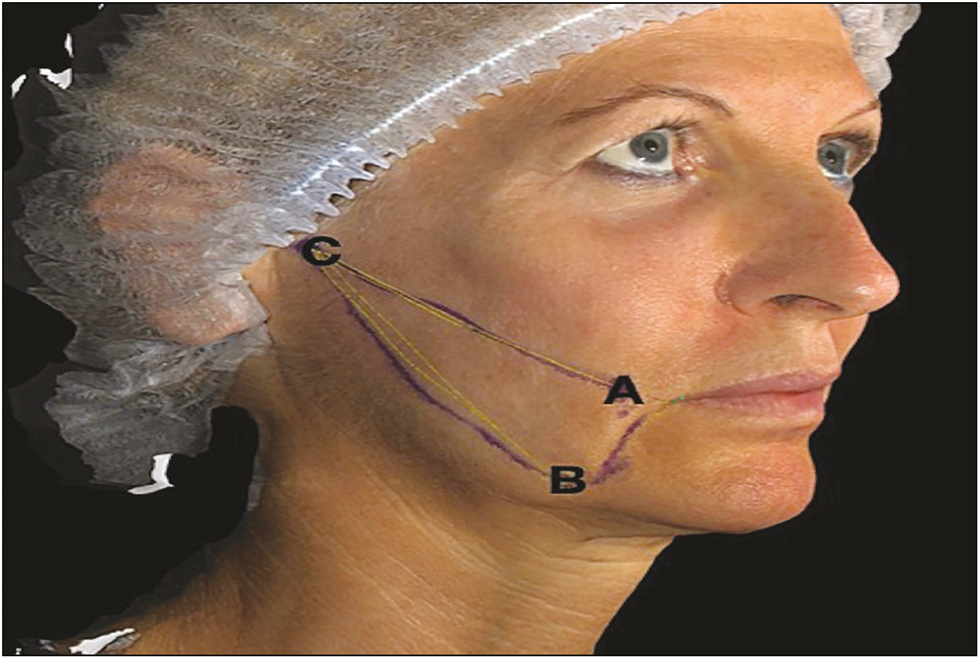
- Reference points
exit point at the marionette line origin (point A),
exit point at the bottom of the jowl (point B), and
entry point in front of the tragus (point C).
Once the thread was inserted into this V-shaped pattern, the tissues were gently spread along its length and fixed by the monodirectional barbs in the planned position, to reshape the jawline, to properly contour the jowls, and to restore the fullness at the gonial angle.
Image capture and analysis
Patient photographs were taken by using Vectra H1® (Canfield Scientific, Inc, Parsippany, New Jersey) before (t0), immediately after threads implantation (t1), and at the following visit (t2). All patients consented to the reproduction of recognizable photographs.
The system consisted of six cameras positioned in a triangulated configuration with respect to the subject, and each image was composed of high-resolution tridimensional surface geometry.
Each image captured before thread insertion was registered by the software, aligning the vertical vector in the midline of the face and the horizontal one with respect to the Frankfurt line.
The postoperative image was registered to the preoperative image by anthropometric surface landmarks that were least likely to move during thread insertion: bilateral lateral canthon (point Ex, Exocanthon), bilateral nostril (point Al, Alare), and bilateral point tragal notch (point Ar, Articularis).
These landmarks initialized the orientation of the superimposed images and registered them to each other. The surface linear lengths in between the mentioned points C-A and C-B were calculated by the “Vectra Analysis Module” dedicated software [see Table 1] on the patient images at t0 (pretreatment), t1(immediate post-treatment), and t2 at the next examination, and the changes were recorded, respectively, on the period ∂t0-t1 and ∂t0-t2.
| Pt | C-A t0 | C-A t1 | ∂t0-t1 | C-A t2 | ∂t0-t2 | C-B t0 | C-B t1 | ∂t0-t1 | C-B t2 | ∂t0-t2 | Follow-up t0-t2 (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 76.72 | 72.07 | 4.65 | 73.7 | 3.02 | 88.82 | 81.17 | 7.65 | 84.77 | 4.05 | 7 |
| 2 | 82.57 | 78.78 | 3.79 | 80.7 | 1.87 | 81.06 | 77.6 | 3.46 | 78.17 | 2.89 | 10 |
| 3 | 72.37 | 67.06 | 5.31 | 69.13 | 3.24 | 78.56 | 67.16 | 11.4 | 68.63 | 9.93 | 8 |
| 4 | 75.84 | 71.97 | 3.87 | 73.79 | 2.05 | 87.25 | 86.47 | 0.78 | 85.51 | 1.74 | 12 |
| 5 | 88.52 | 86.96 | 1.56 | 84.42 | 1.10 | 98.16 | 93.45 | 4.71 | 95.77 | 2.39 | 3 |
| 6 | 97.92 | 90.71 | 7.21 | 94.03 | 3.89 | 110.49 | 103.03 | 7.46 | 106.37 | 4.12 | 9 |
| 7 | 75.57 | 72.39 | 3.18 | lost | 87.04 | 83.5 | 3.54 | lost | lost | ||
| 8 | 76.48 | 72.12 | 4.36 | lost | 83.45 | 78.12 | 5.33 | lost | lost |
Statistical analysis
The outcome to be evaluated was linear change of the suspended tissue along the jawline in the postoperative image relative to the preoperative image.
A comparison was made between the immediate (t0-t1) and the late (t0-t2) postoperative period.
Statistical analysis was performed by using GraphPad PRISM© Software. D’Agostino-Pearson normality test was performed to verify data distribution. Friedman test for repeated measures was performed to compare results at different time points. The level of significance for statistical analysis was set at P < 0.05.
RESULTS
In total, six out of the eight patients completed the study, with two dropping out during follow-up. Considering the 2 who dropped out, the mean age of the examined population is 58.8 years.
Descriptive statistics are shown in [Tables 2–5]. All analyzed parameters improved significantly (P < 0.05) at t1 and at t2 with respect to t0.
| Table Analyzed | Data 1 |
|---|---|
| Friedman test | |
| P value | 0.0081 |
| Exact or approximate P value? | Exact |
| P value summary | ** |
| Are means signif. different? (P < 0.05) | Yes |
| Number of groups | 3 |
| Friedman statistic | 9 |
| Data summary | |
| Number of treatments (columns) | 3 |
| Number of subjects (rows) | 6 |
| Number of families | 1 | ||||
| Number of comparisons per family | 3 | ||||
| Alpha | 0.05 | ||||
| Dunn's multiple-comparisons test | Rank sum diff, | Significant? | Summary | ||
| ca t0 vs. ca t1 | 0 | No | ns | ||
| ca t0 vs. ca t2 | 9 | Yes | * | ||
| ca t1 vs. ca t2 | 9 | Yes | * | ||
| Test details | Rank sum 1 | Rank sum 2 | Rank sum diff, | n1 | n2 |
| ca t0 vs. ca t1 | 15 | 15 | 0 | 6 | 6 |
| ca t0 vs. ca t2 | 15 | 6 | 9 | 6 | 6 |
| ca t1 vs. ca t2 | 15 | 6 | 9 | 6 | 6 |
| Table Analyzed | Data 1 |
|---|---|
| Friedman test | |
| P value | 0.0001 |
| Exact or approximate P value? | Exact |
| P value summary | *** |
| Are means signif. different? (P < 0.05) | Yes |
| Number of groups | 3 |
| Friedman statistic | 12 |
| Data summary | |
| Number of treatments (columns) | 3 |
| Number of subjects (rows) | 6 |
| Number of families | 1 | ||||
| Number of comparisons per family | 3 | ||||
| Alpha | 0.05 | ||||
| Dunn's multiple-comparisons test | Rank sum diff, | Significant? | Summary | ||
| cb t0 vs. cb t1 | 6 | No | ns | ||
| cb t0 vs. cb t2 | 12 | Yes | ** | ||
| cb t1 vs. cb t2 | 6 | No | ns | ||
| Test details | Rank sum 1 | Rank sum 2 | Rank sum diff, | n1 | n2 |
| cb t0 vs. cb t1 | 18 | 12 | 6 | 6 | 6 |
| cb t0 vs. cb t2 | 18 | 6 | 12 | 6 | 6 |
| cb t1 vs. cb t2 | 12 | 6 | 6 | 6 | 6 |
All the mentioned surface linear lengths were measurement retrieved by the Vectra H1 (Canfield Scientific, Inc, Parsippany, New Jersey) 3D software on patient images.
The result showed an overall average improvement of 4.24 mm in the “tragus-to-marionette distance” (C-A) immediately (t0-t1) after the thread implantation, to a mean value of 3.03 mm at the end of the 8.16 months of follow-up (t0-t2) time. [Figures 3–8]
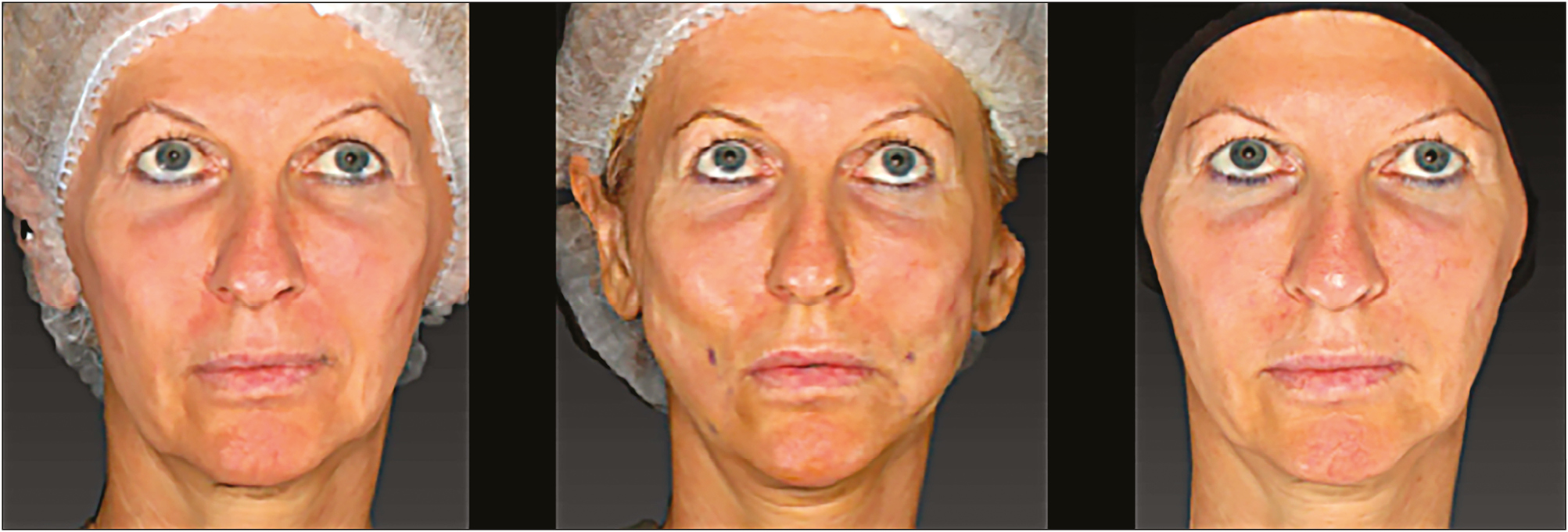
- Patient 1. Frontal view: pretreatment t0 (left), post-treatment t1 (center), and 8 months post-treatment t2 (right)

- Patient 1. Oblique view, right: pretreatment t0 (left), post-treatment t1 (center), and 8 months post-treatment t2 (right)

- Patient 1. Oblique view, left: pretreatment t0 (left), post-treatment t1 (center), and 8 months post-treatment t2 (right)

- Patient 2. Frontal view: pretreatment t0 (left), post-treatment t1 (center), and 8 months post-treatment t2 (right)

- Patient 2. Oblique view, right: pretreatment t0 (left), post-treatment t1 (center), and 8 months post-treatment t2 (right)

- Patient 2. Oblique view, left: pretreatment t0 (left), post-treatment t1 (center), and 8 months post-treatment t2 (right)
Regarding the “tragus-to-jowl distance” (C-B), the mean immediate (t0-t1) improvement recorded was 5.54 mm, which was maintained at 4.18 mm after a mean follow-up time of 8.16 months (t0-t2), ranging from 3 to 12 months. [Figures 3–8]
No adverse event was reported either during thread insertion or later, except for a slightly painful sensation at the pre-tragus point, where threads were inserted, which shows spontaneous resolution in all the cases.
Patient discomfort was considered mild, mainly related to thread perception, and presented with spontaneous resolution in all the treated cases.
DISCUSSION
Since the earliest reports of facial surgical rejuvenation by Miller and Kolle, more durable and less invasive means of rejuvenating the face have been sought.[89]
Between the 1980s and the 1990s, approaches to skin laxity and facial tissues ptosis through direct excision raised the peak of maximal invasivity. After Mitz and Peyronie defined the superficial musculoaponeurotic system (SMAS), rejuvenation methods evolved from skin-only rhytidectomy to a range of soft tissue repositioning and SMAS lift adaptations.[1011]
The first author who mentioned the concept of barbed sutures related to aesthetic applications of tissue suspension was the Georgian author Marlen Sulamanidze in the late 1980s; since the late 1990s, thread lifting developed as a minimally invasive technique relying on anti-ptosis threads and sutures.[112,13]
The face has a layered structure made of skin, subcutaneous and deep fat, the SMAS, and voluntary muscles, which overlie a bony framework, and all these evolve with age.
The effectiveness of thread lifting is related to the known focal nature of soft tissues ptosis, as it is widely accepted that with aging some areas of the face sag more than others. This outlines the differences against a youthful face, where the smooth transition between different facial regions provides for the harmony of areas of concavity and convexity within the subject’s frame.[1415]
Neglect of the fundamental principles of the topographic anatomy of facial aging and lack of the knowledge of the vectors that must be applied to achieve optimum tissue elevation prevent an improvement in treatment outcomes. Instead, all procedures should consider that this is not just a matter of “pulling the sheet over an unmodified mattress.”[1617]
In the aging face, the jawline loses projection and definition due to gravitational ptosis and also because of the action of the Platysma muscle, which acts as a major depressor in this region; these come along with jowl fat hypertrophy and loosening of the masseteric cutaneous ligaments. The definition between the face and the neck becomes obscured given that these changes lead to an irregular jawline contour, which is almost sinusoidal in its appearance.
Gravity, therefore, plays a key role in lower face aging, and thread lifting techniques have been conceived to deal with it. These must be addressed to treat moderate cutaneous ptosis requiring a relatively modest degree of suspension.[1819202122]
Superficial tissue suspension for the aging face allows one to take advantage of the residual fullness of the subcutaneous fat to achieve jawline skin repositioning along a vector that is postero-superiorly oriented. The sliding movement of the skin and subcutaneous fat due to gravity is, therefore, inverted and the tissues spread along the jawline to gently rejuvenate it.
Indeed, in case of severe tissue aging, traditional surgical lifting may be more suitable as it allows to actually reposition the full thickness of facial skin and deep volumes.[1123]
Further, the way the thread works histologically is not to be forgotten when dealing with longevity of results: A microscopic examination on implanted threads showed that they are covered with a solid fibrous membrane, which is especially pronounced around the barbs and confirms the stability and persistence of good clinical results.[18]
In this prospective study, the authors quantitate the long-term linear changes (up to 8 months) along the mandibular border by employing the thread lifting technique mentioned in this article. The reported outcomes have been further validated by statistical analysis.
Patients seem to prefer minimally invasive procedures and have been willing to accept a more modest degree of aesthetic improvement in return for decreased morbidity and more rapid healing; however, disregarding this limitation will certainly lead to an early relapse of ptosis and to poor outcomes.[14]
Regardless of the learning curve point at which the practitioner currently stands, it is mandatory to state that from a technical point of view “thread face-lifting” should be seen as a temporary rejuvenating procedure until patient aging requires further approaches.
Although the morphologic changes that occur with aging have been extensively and objectively characterized with conventional imaging techniques[2425] little or no parameters exist nowadays that suggest how much to define the jawline with respect to desirable outcomes and the assessment of facial aesthetic outcomes largely remains a subjective evaluation without an objective means of measurements.
The introduction of tridimensional stereophotogrammetry, as a method to make reliable measurements on photographs by using the coordinates captured simultaneously by two or more configured cameras from different angles, allows one to objectively compare the outcomes and their longevity.
The data calculated from a collection of points obtained along a three-axis-coordinates system allow one to obtain, once elaborated by the dedicated software, reliable measurements along with tridimensional images of outcomes and their comparison with the facial aesthetics before treatment.[1011]
Cosmetic procedures are very subjective and, beyond the mere judgment of patients and clinicians, it is thus strongly recommended to bridge this gap when dealing with facial aging treatment.[26]
The aim of this pilot study is to quantitatively investigate and to validate the effectiveness in lifting sagging tissue for the correction of mild-to-moderate ptosis of the jawline in a small group of eight patients, by taking 3D images before and after thread insertion and by assessing and comparing, through a dedicated tool, linear changes over time.
Neither side effects nor complications were recorded: The presented operative protocol can, therefore, be considered as safe and reliable.
Our results showed that it is possible to achieve tissue repositioning, which may last up to 8 months, as per the recorded follow-up period.
This study, however, has at least some limitations that require consideration. The mean age of the study population is quite advanced (58.8 years, without considering two drop-offs); however, in daily practice, this rejuvenating technique is usually addressed to younger patients.
The outcomes have been assessed on the jawline in terms of a range of linear lengths; nevertheless, bidimensional measurements are a limited expression of the clinical outcomes. In this context, this has been chosen merely to help the reader correlate it with the jawline rejuvenation through its superficial reshaping via the sliding movement of the skin and subcutaneous fat. Further investigations on facial tissue volume assessment are, therefore, desirable.
As this is a pilot study, the limited number of treated subjects urges the authors to consider the presented outcomes as preliminary, although statistically validated, since it was not possible to carry out an age-related analysis.
Further, the follow-up duration is somewhat limited, with respect to PLLA-PCA thread longevity, which is claimed to be between 12 and 18 months; the authors agree with the latter claim and consider that the mentioned follow-up variability (3 to 12 months) is coherent with a pilot study, and it is reliable as the presented statistical evaluation.
Indeed, investigations with a longer follow-up are strongly advised.
To the best of our knowledge, this is the first objective, standardized photographic analysis of facial suspension through barbed, resorbable threads.
This clinical study and the statistical evaluation have been carried out to overcome the subjectivity of cosmetic procedure assessment in evaluating thread lifting, thus providing detailed and reliable results up to 8 months. Since the authors strongly believe that this kind of evidence has to be incorporated into clinical practice, even starting out from pilot studies such as the one presented here up to high-quality studies, evidence based medicine is essential to our mission of providing better answers for our patients.
CONCLUSIONS
The results of this pilot study suggest that facial tissue suspension by means of poli-lactic/poli-caprolactone threads is safe and effective in treating skin flaws that affect mild-to-moderate ptosis of the jawline up to 8 months.
Their action in suspending facial tissues is immediate, effective, and reliably long-lived, with regard to the follow-up duration presented in our patient series.
Longer follow-up, larger patient groups, and studies on different facial areas are, indeed, needed to objectively assess the effectiveness of treating facial ptosis and of valuing the role of thread-lifting techniques in major facial rejuvenating procedures since the preliminary results experienced in this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In their form/forms, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in this journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Dr. Diaspro is a consultant for Aptos LLC, and Dr. Luni is a consultant for Aptos LLC.
No grants, equipment, or drugs were received for this article.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Thread-lift sutures: Still in the lift? A systematic review of the literature. Plast Reconstr Surg. 2018;141:341e-7e.
- [Google Scholar]
- The emerging technique of the antiptosis subdermal suspension thread. Dermatol Surg. 2004;30:41-4; discussion 44.
- [Google Scholar]
- Barbed polypropylene sutures for midface elevation. Arch Facial Plast Surg. 2005;7:55.
- [Google Scholar]
- Outcomes in thread lift for face and neck: A study performed with silhouette soft and promo happy lift double needle, innovative and classic techniques. J Cosmet Dermatol. 2019;18:84-93.
- [Google Scholar]
- Subcutaneous section of the facial muscles to eradicate expression lines. Am J Surg. 1907;21:235.
- [Google Scholar]
- Thread-lift for facial rejuvenation: Assessment of long-term results. Arch Facial Plast Surg. 2009;11:178-83.
- [Google Scholar]
- Evaluation of facial volume changes after rejuvenation surgery using a 3-dimensional camera. Aesthet Surg J. 2016;36:379-87.
- [Google Scholar]
- A novel extended deep plane facelift technique for jawline rejuvenation and volumization. Aesthet Surg J. 2019;39:1265-81.
- [Google Scholar]
- APTOS suture lifting methods: 10 years of experience. Clin Plast Surg. 2009;36:281-306, viii.
- [Google Scholar]
- Silhouette sutures for treatment of facial aging: Facial rejuvenation, remodeling, and facial tissue support. Clin Plast Surg. 2008;35:481-6, v.
- [Google Scholar]
- Barbed sutures for aesthetic facial plastic surgery: Indications and techniques. Clin Plast Surg. 2008;35:451-61.
- [Google Scholar]
- Evaluation of a novel technique for wound closure using a barbed suture. Plast Reconstr Surg. 2007;120:349-50; author reply 350.
- [Google Scholar]
- A novel option of uninterrupted closure of surgical wounds. J Cutan Aesthet Surg. 2009;2:81-7.
- [Google Scholar]
- Pathomorphological criteria of use efficiency of resorbable and permanent implants in aesthetic medicine and cosmetic dermatology. J Cosmet Dermatol. 2018;17:731-5.
- [Google Scholar]
- Age- and gravity-related changes in facial morphology: 3-dimensional analysis of facial morphology in mother-daughter pairs. J Oral Maxillofac Surg. 2008;66:1410-6.
- [Google Scholar]
- The role of gravity in periorbital and midfacial aging. Aesthet Surg J. 2014;34:809-22.
- [Google Scholar]
- The dynamic rotation of langer’s lines on facial expression. J Plast Reconstr Aesthet Surg. 2007;60:393-9.
- [Google Scholar]
- The efficacy of polycaprolactone threads in Zygomatic and mandibular lifting: Consecutive study from a single Practitioner’s experience. Int J Clin Expl Dermatol.
- [Google Scholar]
- Quantifying soft tissue loss in facial aging: a study in women using magnetic resonance imaging. Dermatol Surg. 2013;39:1895-902.
- [Google Scholar]
- Quantifying soft tissue loss in the aging male face using magnetic resonance imaging. Dermatol Surg. 2014;40:786-93.
- [Google Scholar]
- Why evidence-based medicine matters to aesthetic surgery. Aesthet Surg J. 2012;32:117-9.
- [Google Scholar]






