Translate this page into:
To Compare the Efficacy and Safety of Autologous Non-cultured Non-trypsinized Keratinocyte and Melanocyte Grafting (Jodhpur Technique) with Autologous Platelet-Rich Fibrin Matrix (PRFM) in the Treatment of Chronic Non-healing Ulcer
Address for correspondence: Dr. Dilip Kachhawa, Bunglow No. 3, Outside Gate No. 1, MDM Hospital, Jodhpur, Rajasthan, India. E-mail: drdilipkachhawa@hotmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background:
Chronic non-healing ulcers (NHUs) are often associated with some underlying pathology which prevents timely healing thus increasing the patients morbidity and healthcare expenses. Autologous non-cultured non-trypsinized keratinocyte and melanocyte grafting also known as Jodhpur technique (JT), an epidermal graft and autologous platelet-rich fibrin matrix (PRFM) are newer modalities with promising results.
Aims:
To compare the efficacy and safety of JT and autologous PRFM in the treatment of chronic NHU. Design: A prospective hospital based interventional study conducted on 50 patients of chronic NHU attending the dermatology outdoor of a tertiary level government hospital.
Materials and Methods:
After taking clearance from the institutional ethical committee, the patients were enrolled into 2 groups of 25 each. JT was done on group A and autologous PRFM on group B and their efficacy and safety compared.
Statistical Analysis:
Chi square test was used to analyze categorical variables summarized as number and percentage while continuous variables were analyzed using student t-test for intergroup comparison.
Results:
In Group A, the mean time to ulcer healing was 6.17 ± 2.17 weeks while 6.43 ± 2.33 weeks in Group B. No side effects were found in either group.
Conclusion:
Both the techniques fair equally in terms of wound healing time and safety but required multiple sittings in group B and a single session in group A.
Keywords
Autologous non-cultured non-trypsinized keratinocyte and melanocyte grafting
autologous platelet-rich fibrin matrix
Jodhpur technique
non-healing ulcer
INTRODUCTION
Wound healing is a well-organized, sequential, and timed repair process; any failure in this process or the failure of this process to attain full anatomical and functional integrity results in non-healing ulcer (NHU).[1] These are usually spontaneous or traumatic, unresponsive to initial therapy and appropriate care, and do not proceed toward healing in a defined period of time with an underlying local or systemic etiology.[23] In an Indian epidemiological study, the prevalence of chronic ulcer was found to be 4.5/1000 population.[4] Underlying causes include varicose veins, diabetes, trauma, vasculitis, iatrogenic, etc. Various complications associated with NHU are infections, chronic pain, discharge, limitation of movement, and decreased quality of life; at the same time, these are also a cause for embarrassment and frustration to the patient. Frequent visits to hospital for treatment entail huge costs on the patient and society.
Proper and timely management is key to reducing the complications. Conventional modalities include surgical debridement, dressings, antiseptics, etc. Most of the techniques have a common shortcoming in the form of failure to provide growth factors which are essential for wound healing.[5] Punch grafting, split thickness skin graft, and follicular unit transplant are some of the surgical modalities tried in NHUs each with variable results. Epidermal grafting is a newer approach for the treatment of NHU and it acts like a bioengineered skin in which basal keratinocytes retain their structure and proliferative activity. Autologous non-cultured non-trypsinized keratinocyte and melanocyte grafting also known as Jodhpur technique (JT)[6] is a type of epidermal graft, which has been successfully tried in the treatment of vitiligo, and few studies have shown its efficacy in NHUs.
Platelet concentrates are the recent addition in the armamentarium of treatments available, which directly act by release of growth factors in the wound bed. Autologous platelet-rich fibrin matrix (PRFM) is next generation platelet concentrate which acts by mimicking the natural wound healing environment.
Objectives
The aim of this article is to compare the efficacy and safety of autologous non-cultured non-trypsinized keratinocyte and melanocyte grafting (JT) with autologous PRFM in the treatment of chronic NHU.
MATERIALS AND METHODS
A hospital-based prospective interventional study was carried out in the Dermatology Department of Dr S. N. Medical College, Jodhpur, Rajasthan, India. Ethical clearance was taken from the Institutional Ethical Committee. Fifty patients with NHU of various etiologies were enrolled for the study after taking written informed consent and divided into two treatment groups, i.e., A and B each consisting of 25 patients. Autologous non-cultured non-trypsinized keratinocyte and melanocyte grafting (Jodhpur technique) was performed on group A and group B patients. Autologous PRFM was done.
Inclusion criteria include chronic ulcer of more than 6 weeks’ duration and patients with controlled blood sugar. Exclusion criteria were kept as follows: ulcer less than 6 weeks’ duration, actively infected ulcer, diabetic patients with uncontrolled blood sugar, malignancy, and patients with HIV-AIDS. Detailed history was elicited from the patient and recorded in a case-recording proforma. The patient was then subjected to general, systemic, and local ulcer examination. Local examination included size, shape, surface, number, site, edge, floor, base, discharge, surrounding skin, tenderness, temperature, and regional lymph node examination of all ulcers. Observations were made regarding subjective complaints of pain, fever, discomfort, discharge, etc.
Relevant investigations were done including complete blood count, blood sugar, HbA1c, viral markers such as HIV and HbsAg, liver function test, blood urea, creatinine, etc. The patients were started on tablet cefixime 200 mg twice daily for 5–7 days and analgesics. Diabetes patients received insulin injections or oral hypoglycemic drugs according to blood sugar levels. In other cases, etiologically directed treatment was carried out. Dirty ulcers were first subjected to debridement to make them suitable for surgery.
Wound area was calculated using the formula for an ellipse: Length × width × 0.7854. An ellipse for calculating wound measurement has been used in randomized controlled trials in wound healing literature.[78] Volume was calculated using the formula: (length × width × 0.7854) × depth.[8] Area, volume measurements, and photographic assessments were done at weekly follow-up.
Jodhpur technique
At first, both the recipient and donor sites were anesthetized using 2% lignocaine and then dermabrasion was done at 4000–5000 rpm using a micromotor. The recipient site is to be prepared first. Marginal dermabrasion was done at the ulcer with pinpoint bleeding being the end point.
Lateral area of thigh was selected as a donor area in all the cases, and after applying 2% mupirocin ointment, dermabrasion was done till pinpoint bleeding. The epidermal particles fragmented during dermabrasion gets entangled in ointment, and a paste-like material was obtained. With the help of a graft spreader, this paste was spread evenly over the recipient ulcer site.
The recipient site was then dressed using non-absorbable dressing followed by secondary gauze dressing and left for 7 days. Routine care of the ulcer site was advised to all patients. Weekly assessment was done without any intervention, followed by re-dressing.
Autologous PRFM
Taking strict aseptic precautions, 10 mL of venous blood was drawn using a 10 cc syringe and transferred to a sterile centrifugation tube without any anticoagulant. At a setting of 3000 rpm, centrifugation was done for 10 min. Following this, three distinct layers were formed, namely, platelet-poor plasma (PPP) which is the uppermost straw-colored layer, followed by mesh-like middle fraction, the PRFM, and the lowermost red-colored layer composed of red blood cells. After discarding PPP, a pair of sterile forceps was used to separate PRFM from the lowermost layer and transfer it onto a sterile gauze. The matrix was then compressed between two gauze pieces gently and applied on to the clean wound, followed by application of a non-absorbable dressing and a secondary gauze dressing. Adequate rest was ensured during the treatment course. At the end of every week, the dressing was removed, ulcer healing assessed and fresh PRFM was applied followed by dressing. The procedure was repeated weekly for five sessions.
RESULTS
Fifty patients were enrolled in the study and distributed into two groups of 25 each, group 1 treated with JT and group 2 treated with PRFM. In both the groups, majority of patients were in the age group of 40–50 years with mean age being 48±11 years. Thirty-four (68%) patients were males and 16 (32%) were females.
Overall, the most common cause of ulcer was found to be traumatic in about 16 (32%) patients, followed by other causes such as burn, animal or snake bite, etc. in about 14 (28%), varicose veins in 9 (18%), diabetes in 6 (12%) patients, followed by leprosy 3 (6%) and infectious cause in the remaining 2 (4%) patients.
With regard to the duration of ulcer, in group A, 12 (48%) patients had ulcers of 1.5–2.5 months duration, 9 (36%) between 2.5 and 4 months, and 4 (16%) of more than 4 months duration. In group B, 17 (68%) patients had ulcers of 1.5–2.5 months duration, followed by 7 (28%) had ulcers of 2.5–4 months duration and 1 (4%) had ulcer of more than 4 months duration.
In group A, the most common site of ulcer was lower leg in 13 (52%) patients, followed by foot in 5 (20%), sole in 3 (12%), 2 (8%) in upper leg, and 1 (4%) in upper limb and abdomen each. In group B, the most common site of ulcer was lower leg in 18 (72%) patients, followed by abdomen in 3 (12%), upper limb in 2 (8%), and 1 (4%) each on sole and upper leg.
In group A, 10 (40%) patients complained of pain at presentation and 16 (64%) patients complained of discharge from the ulcer, whereas in group B, 9 (36%) patients complained of pain and 10 (40%) complained of discharge from the ulcer at presentation.
In group A, 7 (28%) patients had diabetes mellitus and 6 (24%) had hypertension, whereas in group B, 6 (24%) patients had diabetes and 4 (16%) patients had hypertension. In both study groups, 23 (92%) patients had complete healing and 2 (8%) patients had partial healing.
Out of the 46 patients showing complete ulcer healing, maximum patients [29 (63.04%)] showed ulcer healing in 4–8 weeks; in 13 (28.26%) patients, healing was seen in less than 4 weeks and remaining 4 (8.69%) showed healing in 8–12 weeks.
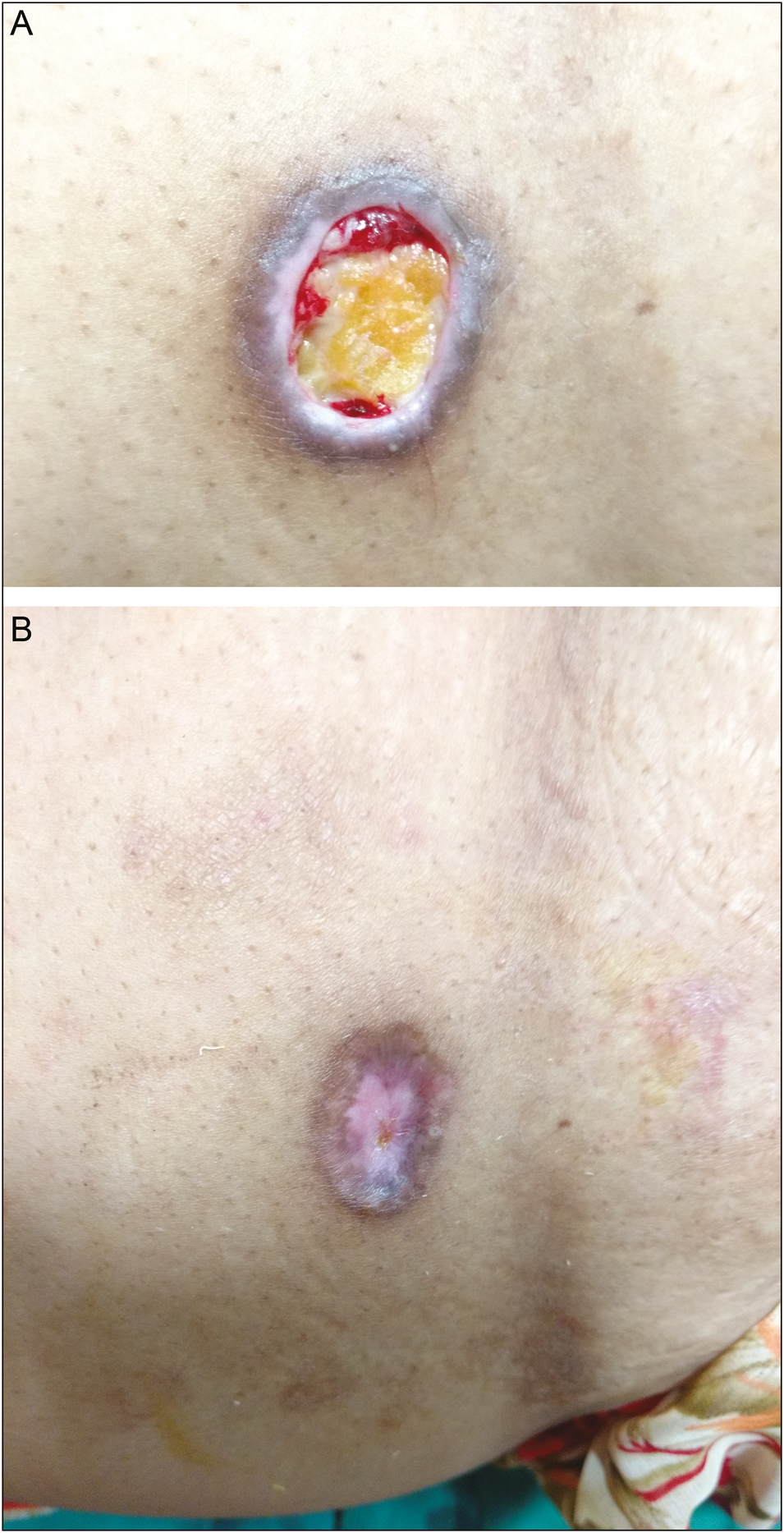
In group A, a maximum of 15 (65.22%) patients showed healing in 4–8 weeks, followed by 6 (26.08%) in less than 4 weeks and 2 (8.69%) took 8–12 weeks to heal [Figures 1A, B and 2A, B].

- A: Ulcer before JT. B: Ulcer at 12 weeks after JT

- A: Ulcer before JT. B: Ulcer at 12 weeks after JT
While in group B, 14 (60.87%) patients had healing in 4–8 weeks, followed by 7 (30.43%) in less than 4 weeks and 2 (8.69%) patients took 8–12 weeks to heal [Figures 3A, B and 4A, B].
- A: Ulcer before autologous PRFM application. B: Ulcer at 12 weeks after autologous PRFM application
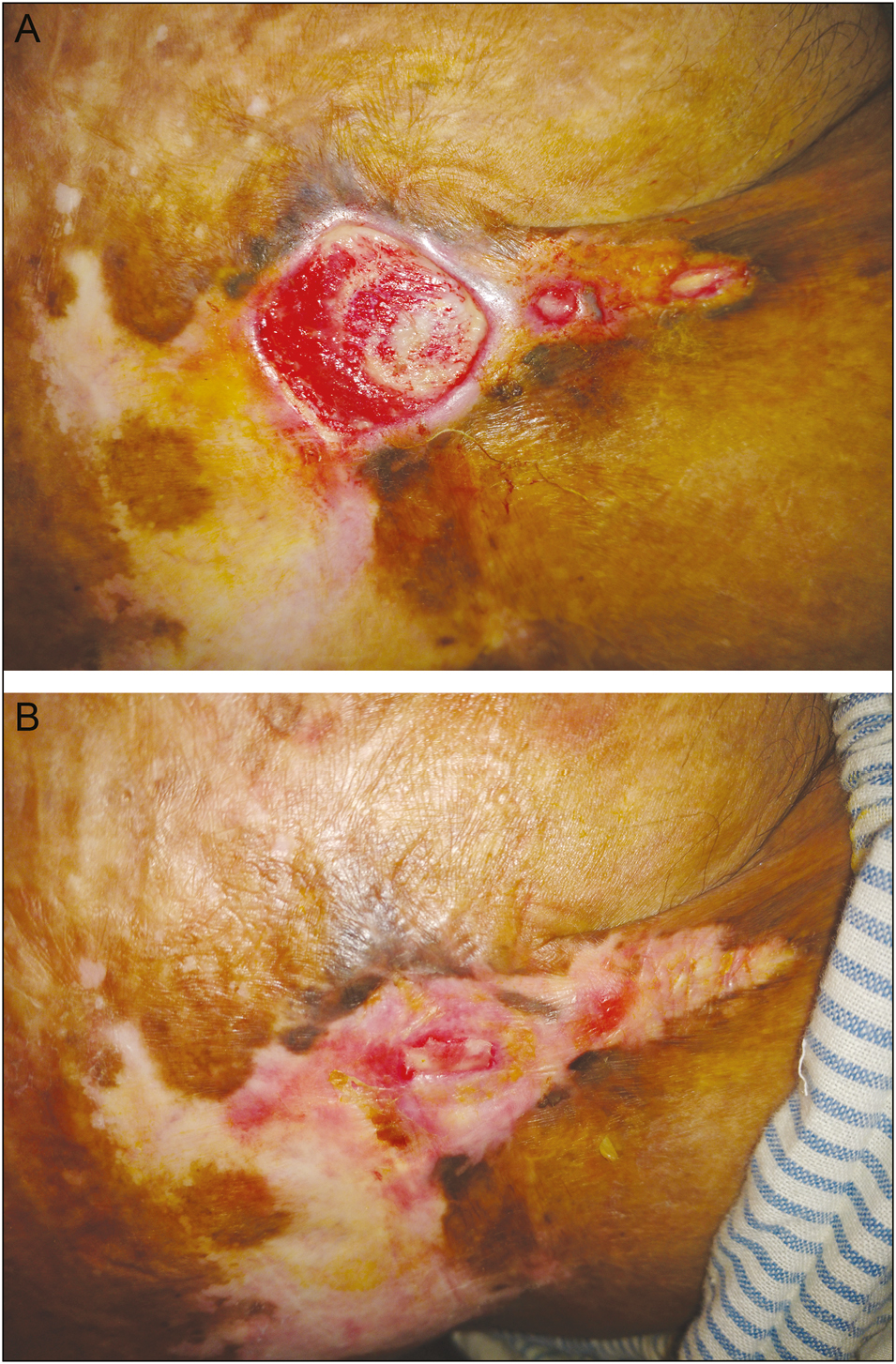
- A: Ulcer prior to autologous PRFM. B: Ulcer at 12 weeks after autologous PRFM application
Overall, the mean time to ulcer healing was 6.27± 2.24 weeks. In group A, the mean time to ulcer healing was 6.17± 2.17 weeks, whereas it was 6.43± 2.33 weeks in group B. The differences in healing time were not found to be statistically significant.
At presentation, the mean area of ulcer was 10.23±11.34 cm2 in the JT group and 10.95±9.08 cm2 in the PRFM group, which decreased to 1.13±3.97 cm2 at the end of 12 weeks in the JT group and to 0.43±1.51 cm2 at the end of 12 weeks in the PRFM group. P-value was found to be more than 0.05; thus the change in the area of the ulcer between the two groups was not found to be statistically significant [Figure 5].
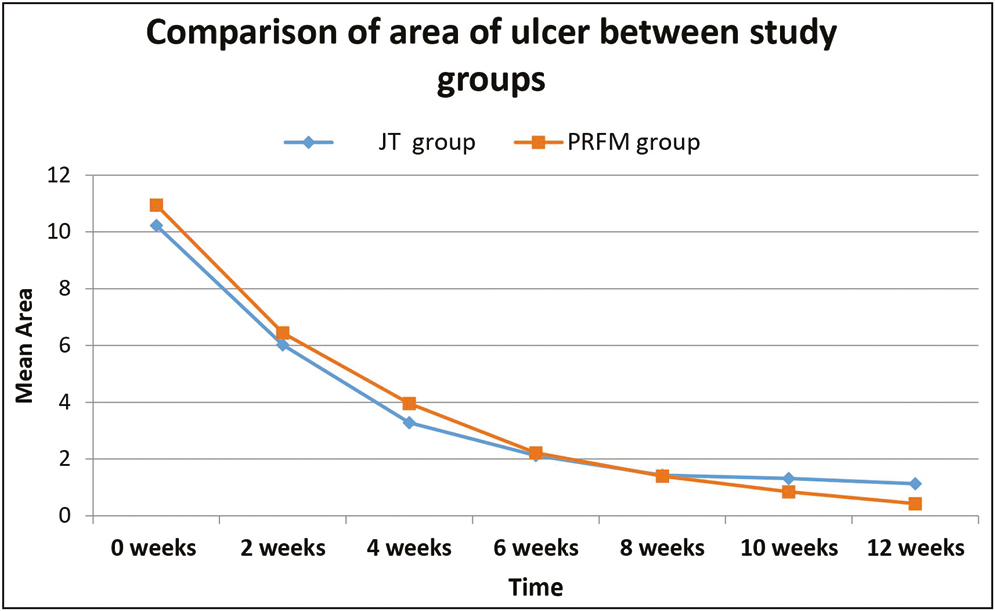
- Graph showing comparison of mean reduction in the area of the ulcer between the two techniques
At presentation, the mean volume of ulcer was 4.31±4.96 cm3 in the JT group and 5.96±4.49 cm3 in the PRFM group, which decreased to 0.19±0.94 cm3 at the end of 12 weeks in the JT group whereas it became 0 at the end of 8 weeks in the PRFM group. P-value was found to be more than 0.05; thus, the change in the volume of the ulcer between the two groups was not found to be statistically significant [Figure 6].
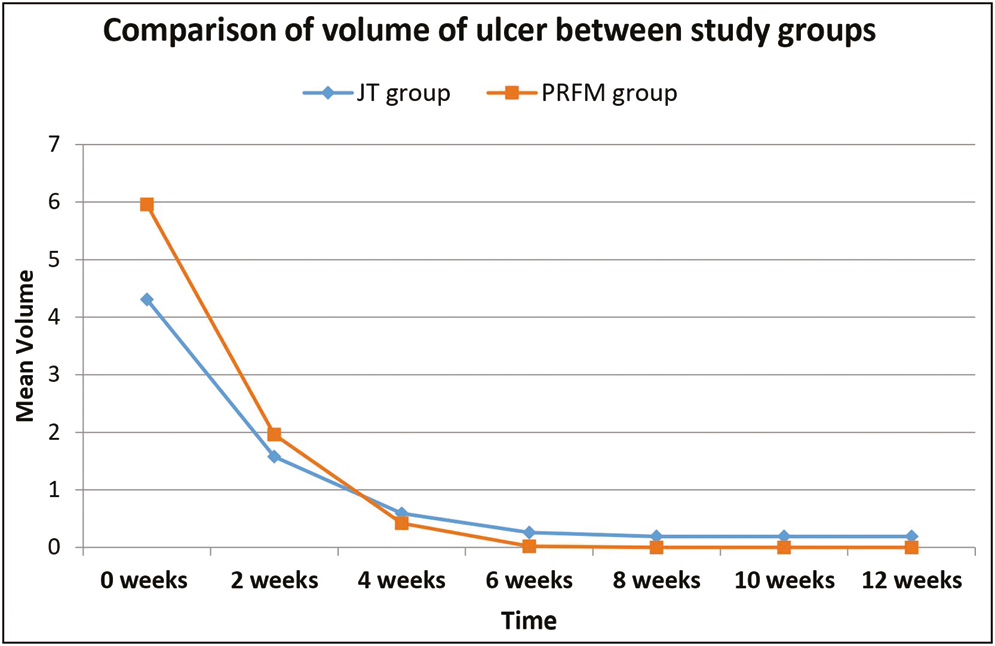
- Graph showing comparison of mean reduction in the volume of the ulcer between the two techniques
DISCUSSION
Ulcer is defined as a break in the continuity of the covering skin or mucus membrane, which may follow molecular death of the surface epithelium or its traumatic removal. Chronic ulcers are characterized by chronic inflammation where active inflammation, destruction of tissue, and attempts at healing are proceeding simultaneously.
Autologous PRFM
PRFM, a membrane-based preparation of PRP,[9] was first developed by Choukroun et al.[10] used in oral and maxillofacial surgery. During centrifugation, the matrix is formed by a natural polymerization process, and at the ultrastructural level, the matrix shows dense highly cross-linked fibrin matrix,[11] which is strong, flexible, and elastic and supports platelets, cytokines, and cellular migration that occurs.
A study by Yazawa et al.[12] showed that when incorporated into the fibrin, the mean concentration of growth factors in the platelet concentrates was highly increased and the fibrin scaffold is responsible for a natural, slow, and sustained release of growth factors and matrix glycoproteins during initial 7 or more days,[13] which is critical for wound healing. Thus, PRFM produces guided tissue regeneration[14] by localizing platelets and growth factors and fostering a physiologic tissue response in the treated area.
Jodhpur technique
A novel type of epidermal grafting, autologous non-cultured non-trypsinized keratinocyte and melanocyte grafting (JT), was first used in vitiligo patches by Dilip Kachhawa and Kalla[6] to give cosmetically acceptable results.
In epidermal graft, basal keratinocytes retain their structural and proliferative activity. Keratinocyte activation and epithelial–mesenchymal interaction between the grafted epidermis and recipient dermis[15] result in the production of growth factors such as transforming growth factor-alpha, vascular endothelial growth factor, and granulocyte colony-stimulating factor and some prohealing cytokines by the keratinocytes.[16] These growth factors initiate keratinocyte migration and epithelialization from the edges of the wound,[17] resulting in accelerated wound healing.
In JT, melanocytes and keratinocytes present in the grafted material are entrapped in the healing tissue of recipient site during the healing phase, and it is these growth factors and cytokines released during wound healing that help in proliferation and migration of keratinocyte and melanocytes..[18] This technique is being done for the first time in non-healing ulcer. Major advantage of this technique is that only the epidermal layer is taken for grafting without damaging the dermal layer, resulting in excellent healing of the donor area.
Hence, graft taken from a small donor area could heal a much larger recipient area and at the same time also give matching with the surrounding skin with respect to regularity of the surface and better color match. This technique can be done on any site, irrespective of whether it is fixed or mobile.
In our study, the mean percentage reduction in area and volume of the ulcer in the PRFM group was found to be 63.8% and 92.9%, respectively, at the end of second week. In a similar study conducted by Nagaraju et al.,[19] the mean percentage improvement in the area was 93.52%, and volume was 97.74% at the end of the second sitting. However, the sample size taken in the study was very small.
At the end of 6 weeks, mean percentage reduction in the area and volume of the ulcer in the PRFM group was found to be 79.72% and 99.6%, respectively, whereas in a study conducted by Prachi et al., the average percentage reduction was 95.84% and 98.18%.[20]
In the JT group, a maximum of 15 (65.22%) patients showed healing in 4–8 weeks, followed by 6 (26.08%) in less than 4 weeks, 2 (8.69%) took 8–12 weeks to heal, and 2 ulcers had partial healing, whereas in a study by Shukla et al.,[21] using autologous epidermal cell suspension transplantation, 9 out of 15 patients healed completely within 20 weeks, 6 had partial healing, 2 had delayed healing (by 32 and 48 weeks), and therapy failed in 1 patient.
In our study, the mean time to ulcer healing was 6.17± 2.17 weeks in the JT group, which is similar to a single case report with this technique which showed 100% healing of the ulcer at the end of 6 weeks.[22]
In group A, the mean time to ulcer healing was 6.17± 2.17 weeks, whereas it was 6.43± 2.33 weeks in group B. The differences in healing time were not found to be statistically significant. No side effects were noted in either group.
CONCLUSION
Both the techniques were found to be equally efficacious and safe in the treatment of chronic NHU. However, JT had some advantages over the other techniques; the PRFM group required multiple sittings at weekly intervals whereas the JT was done only once, thus improving the compliance. In JT, the graft obtained is in the form of a paste, thus it has better stay at the ulcer site and less chances of displacement when compared with autologous PRFM. Small sample size and absence of similar comparative studies are the notable limitations of the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 1994;2:165-70.
- [Google Scholar]
- Efficacy and safety of autologous platelet rich plasma for the treatment of vascular ulcers in primary care: Phase III study. BMC Fam Pract. 2014;15:211.
- [Google Scholar]
- Advanced wound care therapies for non-healing diabetic, venous, and arterial ulcers: A systematic review VA-ESP Project #09-009;.
- [Google Scholar]
- Wound healing research: A perspective from India. Int J Low Extrem Wounds. 2005;4:7-8.
- [Google Scholar]
- Autologous platelet-rich plasma enhances healing of chronic wounds. Wounds. 2009;21:280-5.
- [Google Scholar]
- Keratinocyte-melanocyte graft technique followed by PUVA therapy for stable vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:622-4.
- [Google Scholar]
- Healing of diabetic neuropathic foot ulcers receiving standard treatment. A meta-analysis. Diabetes Care. 1999;22:692-5.
- [Google Scholar]
- Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: A multicenter randomized controlled trial. Diabetes Care. 2008;31:631-6.
- [Google Scholar]
- Autologous platelet-rich fibrin matrix as cell therapy in the healing of chronic lower-extremity ulcers. Wound Repair Regen. 2008;16:749-56.
- [Google Scholar]
- An opportunity in perio-implantology (in French): The PRF. Implantodontie. 2001;42:55-62.
- [Google Scholar]
- A recently developed bifacial platelet-rich fibrin matrix. Eur Cell Mater. 2010;20:13-23.
- [Google Scholar]
- Basic studies on the clinical applications of platelet-rich plasma. Cell Transplant. 2003;12:509-18.
- [Google Scholar]
- Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e45-50.
- [Google Scholar]
- Safety, efficacy, and utility of platelet-rich fibrin matrix in facial plastic surgery. Arch Facial Plast Surg. 2011;13:247-51.
- [Google Scholar]
- Epithelial-mesenchymal interactions in wounds: Treatment of palmoplantar wounds by nonpalmoplantar pure epidermal sheet grafts. Arch Dermatol. 137:621-8.
- [Google Scholar]
- Epidermal micrografts produced via an automated and minimally invasive tool form at the dermal/epidermal junction and contain proliferative cells that secrete wound healing growth factors. Adv Skin Wound Care. 2015;28:397-405.
- [Google Scholar]
- Initial experience with a new epidermal harvesting system: Overview of epidermal grafting and case series. Surg Technol Int. 2014;25:55-61.
- [Google Scholar]
- Epidermal sheet grafts for repigments of vitiligo and piebaldism with review of surgical techniques. Acta Dermatol Venereol. 1997;77:463-6.
- [Google Scholar]
- Autologous platelet-rich fibrin matrix in non-healing trophic ulcers in patients with Hansen’s disease. J Cutan Aesthet Surg. 2017;10:3-7. 10.4103/JCAS.JCAS_17_16
- [Google Scholar]
- Efficacy of autologous platelet rich fibrin matrix in the management of non-healing ulcers. Int J Res Dermatol. 2019;5:686-90.
- [Google Scholar]
- Effect of autologous epidermal cell suspension transplantation in chronic non-healing wounds: A pilot study. Can J Surg. 2010;53:6-10.
- [Google Scholar]






