Translate this page into:
To study the efficacy of autologous non-cultured nontrypsinized epidermal cell grafting (Jodhpur technique) by using of suction blister membrane in stable vitiligo
*Corresponding author: Dilip Kachhawa, Department of Dermatology, Dr. Sampurnanand Medical College, Jodhpur, Rajasthan, India. 1/3 Bungalow Outside MDM Gate No. 3, Shastri Nagar, Jodhpur 342003. drdilipkachhawa@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh H, Yadav C, Singrodia R, Kachhawa D, Rao P. To study the efficacy of autologous non-cultured nontrypsinized epidermal cell grafting (Jodhpur technique) by using of suction blister membrane in stable vitiligo. J Cutan Aesthet Surg. 2024;17:239-45. doi: 10.25259/jcas_152_22
Abstract
Objectives:
This study aimed to evaluate the efficacy of autologous non-cultured non-trypsinized melanocytekeratinocyte grafting (JT) with suction blister membrane as biological dressing in stable vitiligo patches.
Material and Methods:
The study was conducted at Mathura Das Mathur Hospital (MDM), Jodhpur, on 43 patches of Stable vitiligo. It was a prospective single-arm interventional study. All patients were examined clinically and history and informed consent were taken before starting the procedure.
Results:
About 95% of patches showed >50% repigmentation with 83.72% having good to excellent repigmentation. About 88% of patches showed good color matches with an excellent decline in Dermatology Life Quality Index (DLQI). No serious complication was observed in the present study. The most common complication observed both in the donor and recipient area was pain.
Conclusion:
Our study indicates that combining JT with suction blister epidermal grafting is a comparatively effective technique in terms of good repigmentation (≥75% extent of repigmentation), color match, fewer side effects, good patient satisfaction, and DLQI reduction.
Keywords
Vitiligo
Jodhpur technique
Suction blister
INTRODUCTION
Vitiligo is a common, acquired, discoloration of the skin, characterized by well-circumscribed, and ivory or chalky white macules which are flush to the skin surface. Loss of cutaneous pigmentation occurs due to the loss of melanocytes from the basal layer of the epidermis. Etio-pathogenesis of vitiligo is multifactorial and polygenic consisting of genetic, immunological, and environmental factors.
Although the majority of cases are managed by medical therapies, surgical methods are reserved for lesions that do not respond to medical treatment and are stable. In our study, the Jodhpur technique (JT) of vitiligo surgery is modified by preparing the recipient site with the suction blister technique, thus combining the two techniques to obtain a single efficacious modality with hypothetically superior grafting than JT alone.
Aims and objective
The primary objective is to determine the extent of the mean re-pigmented area by autologous non-cultured nontrypsinized melanocyte and keratinocyte grafting (JT) with suction blister membrane as biological dressing.
The secondary objective is to determine the color matching of the re-pigmented area using clinical photography and von Luschan’s chromatic scale. Patient satisfaction is measured by the Dermatology Life Quality Index (DLQI) and Patient Satisfaction Questionnaire (PSQ).
MATERIAL AND METHODS
Study site and duration
This was a hospital-based prospective single-arm interventional study carried out in the department of dermatology at a tertiary institute over 1 year. This study was approved by the Institutional Ethical Committee before commencement, and informed consent was obtained from all patients to be a part of this study. A total of 43 patches from 13 patients were included by applying the following inclusion and exclusion criteria.
Inclusion criteria
The following criteria were included in the study:
Stable vitiligo for more than 6 months not responding to adequate medical management
Vitiligo area measuring less than A = πr2 (r = 2.5 cm).
Exclusion criteria
The following criteria were excluded from the study:
Age <18 years
Keloidal tendency
Immunocompromised patients
Patients with an unrealistic expectation
Bleeding disorders
Pregnant and lactating females
Study sample
The sample size was calculated at a 95% confidence interval assuming an expected 70% or more efficacy (as per findings of a previous study)1 of each procedure. The sample size was calculated using the formula for sample size for estimation of proportion –
N=Z (z_(1-α/2)^2 P[1-P])/d^2
z_(1-α/2)^2: standard normal variate: 1.96
P: proportion: 70%
d: absolute error taken as 20%
The sample size was calculated to be a minimum of 43 patches.
Materials require
Dermabrader (manual or electric), straight forceps, electric motor, 3-way connectors, 10 cc 20 cc,50 cc syringe, and jeweler’s forceps were used.
Technique
Procedure at the recipient site
Before starting the procedure, aseptic precaution and appropriate local anesthesia was done. For raising blisters, we most commonly use syringes and follow the procedure as described by Gupta and Goel.2 Although a suction pump, suction cups, or a negative pressure cutaneous suction chamber system can also be used.
Disposable syringes of varying sizes ranging from 5, 10, or 20 mL are used according to the size of the lesion. If the area of the patch is larger than the diameter of the syringe, multiple syringes at a distance of 2 cm were used. This syringe was then attached to a 3-way tap with a latex tube, a 50 mL syringe for aspiration of air, and a manometer to measure the negative pressure [Figure 1a-d]. The pressure gradient required to produce suction blisters varies according to the age of the patient, site, temperature at the suction site, atrophy, or laxity of the area due to underlying pathological conditions. Ideally, a negative pressure of 300–500 mmHg is required for blister formation.
A disposable syringe is used after removing the plunger, putting the flat side of the barrel on the vitiligo patch, and fixing it with a micropore. To induce the vacuum pressure, a 50 mL syringe and measured with the help of a manometer.
It took 45 min to 2.5 hours for the development of blisters. The end-point is a single unilocular and non-hemorrhagic blister. Normal saline can be used to extend and increase the size of the blister. This technique was used to merge surrounding blisters, especially in a large patch with multiple blisters. It also helps in preventing the perilesional halo. The blister thus obtained is punctured at the base to remove the fluid, thereby creating a pocket for graft placement.

- (a) Multiple vitiligo patches before surgery on the left hand. (b) Suction apparatus in situ. (c) Post-operative at 16 weeks. (d) Post-operative at 20 weeks.
Procedure at donor site
The donor area was shaved, cleaned with betadine and surgical spirit, and anesthetized with a mixture of 2% lignocaine and normal saline in a 1:1 ratio. This was followed by the application of ointment with 0.1% Mupirocin (T-Bact). This helps in preventing the spillage of the graft.
With the help of either mechanical or electrical dermabrader, dermabrasion was continued until the pinpoint bleeding occurred. The material was entangled in mupirocin ointment and was collected with the help of a spatula or graft spreader. The paste-like material obtained by this procedure contains keratinocytes, melanocytes, and dermis.
The area was dressed with three layers, that is, collagen strips, bactigras (framycetin tulle), and elastocrepe or bandage (from inside to out) after the establishment of hemostasis. Suitable antibiotics and analgesics were prescribed.
Transplantation procedure
Lesional transplant
The donor graft paste is then transferred to a slide and mixed with saline to form a homogenous paste. This paste is then collected with the help of a spatula and spread uniformly onto the base of the blister [Video 1].
Video 1:
Video 1:To demonstrate the process of graft preparation through Jodhpur technique and placement of the graft in the recipient site prepared by blister technique.The roof of the blister was then placed over the graft as a biological dressing. This was followed by normal bandages after dressing with antibiotic-soaked gauze.
Suitable analgesics and antibiotics were prescribed. The dressing was removed after 7 and 14 days from the recipient and donor site, respectively.
Follow-up
The patient was asked to lie down for 30 min after the procedure. First, follow-up was done on the 7th day, during which the dressing was removed and the wound was examined. Follow-up visits were planned at the 4th, 8th, 16th, and 20th weeks for pigment assessment by serial photographs, grading system, and PSQs. We measured the severity of vitiligo by vitiligo disease activity score (VIDA) and vitiligo area scoring index scores.
Extent of repigmentation was assigned as follows
<50% Poor repigmentation
50–74% Fair repigmentation
75–89% Good repigmentation
90–100% Excellent repigmentation.
A note was also made of the color matching of re-pigmented skin as “somewhat lighter than,” “same as,” or “somewhat darker than” normal skin.
RESULTS
The study included 43 patches of stable vitiligo treated with autologous non-cultured non-trypsinized epidermal cell grafting (JT) with a suction blister membrane as a biological dressing.
Among the 13 patients, 9 (69.23%) were female and 4 (30.77) were male and age varies from 18 to 38 years with a mean of 25.2 ± 6.8 years [Table 1].
| Age (years) | Gender | Total | ||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| N | % | n | % | n | % | |
| 18–20 | 2 | 40.00 | 3 | 60.00 | 5 | 38.5 |
| 21–25 | 0 | 0.00 | 3 | 100.00 | 3 | 23.1 |
| 26–30 | 1 | 50.00 | 1 | 50.00 | 2 | 15.4 |
| ≥31 | 1 | 33.33 | 2 | 66.67 | 3 | 23.1 |
| Total | 4 | 30.77 | 9 | 69.23 | 13 | 100.00 |
In our study, the foot (34.88%) was the most common site of vitiligo followed by the hand (25.58%) [Table 2]. The outcome of this procedure was assessed at the end of 5 months for the following parameters-extent of repigmentation, color match, and complications at the donor and recipient areas.
| Site of patch | No. of patches | Percentage |
|---|---|---|
| Abdomen | 9 | 20.93 |
| Back | 2 | 4.65 |
| Lip | 2 | 4.65 |
| Foot | 15 | 34.88 |
| Hand | 11 | 25.58 |
| Mandible | 3 | 6.98 |
| Side neck | 1 | 2.33 |
| Total | 43 | 100.00 |
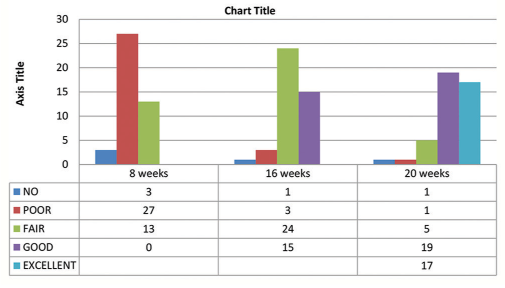
Extent of repigmentation
At 20 weeks, out of 43 patches, 17 patches (39.53%) showed 90–100% (excellent) extent of repigmentation, 19 patches (44.19%) showed 75–89% (good) repigmentation, 5 patches (11.63%) showed 50–74% (fair) repigmentation, and <50% (poor) repigmentation and no repigmentation were seen in 1 patch (2.33%) each [Table 3, Figures 2a-c, 3a and b].
 |
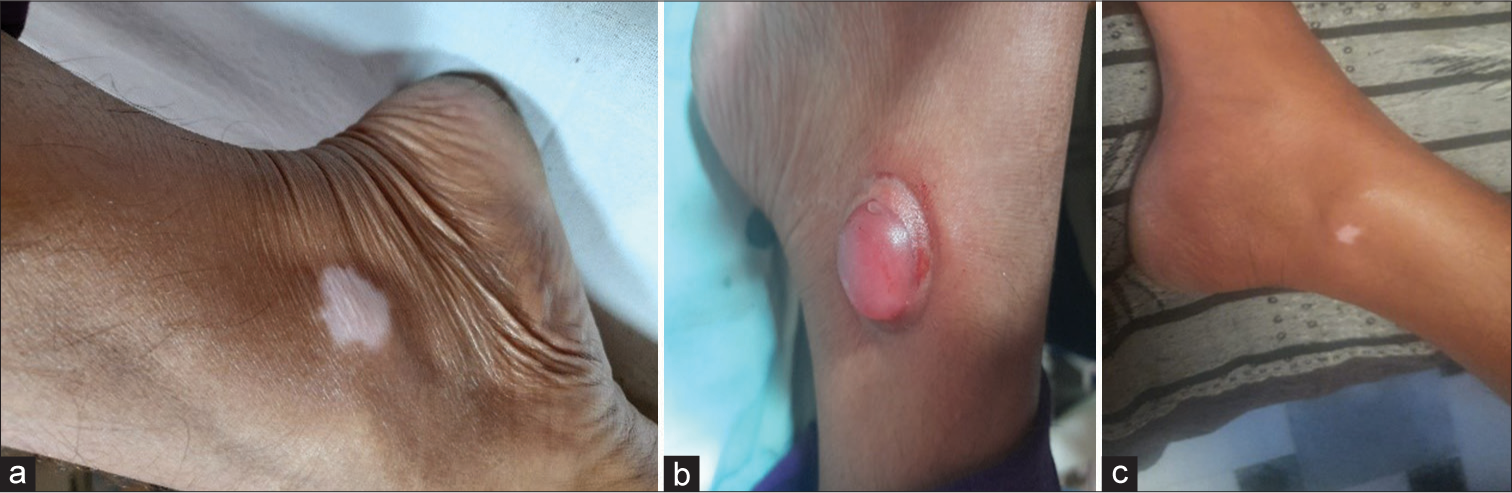
- (a) Vitiligo patch before surgery. (b) Unilocular blister formation. (c) Post-operative at 20 weeks.
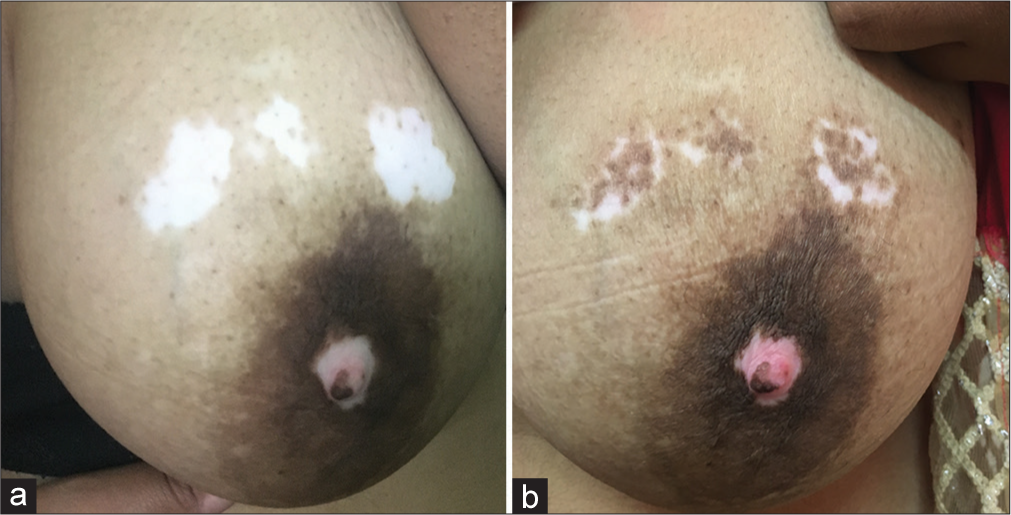
- (a) Before surgery and (b) post-operative at 20 weeks.
Color match
At 20 weeks, out of the 42 patches that showed repigmentation, 38 patches had a color match the same as the surroundings, whereas four patches had a darker color match concerning the surroundings [Table 4].
| Color match of RP with surrounding skin | Total | |
|---|---|---|
| n | % | |
| Follow-up 4 (weeks) | ||
| Same as surrounding skin | 27 | 62.79 |
| Somewhat darker | 6 | 13.95 |
| Not applicable | 10 | 23.26 |
| Follow-up 8 (weeks) | ||
| Same as surrounding skin | 34 | 79.07 |
| Somewhat darker | 7 | 16.28 |
| Not applicable | 2 | 4.65 |
| Follow-up 16 (weeks) | ||
| Same as surrounding skin | 37 | 86.05 |
| Somewhat darker | 5 | 11.63 |
| Not applicable | 1 | 2.33 |
| Follow up 20 (weeks) | ||
| Same as surrounding skin | 38 | 88.37 |
| Somewhat darker | 4 | 9.30 |
| Not applicable | 1 | 2.33 |
RP: Repigmentation.
Among 26 patches of acral vitiligo, 9 (34.62%) patches showed excellent repigmentation, 11 (42.31%) showed good repigmentation, fair in 4 (15.38%) patches, and no repigmentation and poor repigmentation were seen in 1 (3.85%) patch each [Table 5].
| Extent of regimentation | Acral vitiligo | Non-acral vitiligo | ||
|---|---|---|---|---|
| n | % | n | % | |
| No | 1 | 3.85 | 0 | 0.00 |
| Poor | 1 | 3.85 | 0 | 0.00 |
| Fair | 4 | 15.38 | 1 | 5.88 |
| Good | 11 | 42.31 | 8 | 47.05 |
| Excellent | 9 | 34.62 | 8 | 47.05 |
Among 17 patches of non-acral vitiligo, excellent repigmentation, and good repigmentation were seen in 8 (47.05%) patches each, fair in 1 (5.88%) patches, and no repigmentation and poor repigmentation were not seen in any of the patches. The DLQI reduced from a mean value of 18 before surgery to 6.84 after surgery. This finding was statistically significant [Table 6].
| Variables | Pre DLQI (Mean±SD) | Post DLQI (Mean±SD) |
|---|---|---|
| Mean±SD | 18.00±3.46 | 6.84±2.82 |
| Standard error or mean | 0.96 | 0.78 |
| Range | 12–24 | 2–10 |
| Median | 17 | 8 |
| Mean difference | 11.15 | |
| P-value | <0.0001 | |
DLQI: Dermatology life quality index, SD: Standard deviation
Complication at donor and recipient site
Out of 13 patients who underwent the procedure, most patients did not report any post-operative discomfort. Few reported pain which was easily relieved by oral analgesics.
DISCUSSION
Surgical attempts to treat vitiligo began around the 1960s. Since then, many different approaches with many refinements have been successfully reported. These surgical techniques are based on the principle of restoring melanocytes in the recipient vitiligenous areas, obtained from pigmented donor skin. Among the various surgical modalities autologous, non-cultured non-trypsinized, melanocytes plus keratinocyte grafting aka JT is an easy, safe, inexpensive, and effective procedure with a success rate.
In conventional JT, dermabrasion is used for recipient site preparation. It is a quick and effective method with minimal risk of scarring and is more economical. However, it is an instrument that requires proper manipulation, pressure, and control for abrading to the papillary dermis and to obtain uniform de-epithelization for graft uptake. It is dependent on the skill of the surgeon and lacks reproducibility.
Thirteen cases of stable vitiligo of focal, segmental, and generalized types with 43 vitiligo patches constituted the study population with the age of these patients ranging from 18 to 38 years with a mean of 25.2 ± 6.8 years which was comparable to the study done by Mahajan et al.3 in which mean age was 24.4 years and by Gupta and Kumar,4 with a mean age of 27.07 ± 10.32 years.
In the initial study conducted on JT by Kachhawa et al. done on 437 vitiligo patches, more than 75% re-pigmentation (excellent improvement) was seen in 50% of the patches.5
In a recent study conducted by Lamoria et al.,1 he compared follicular unit transplantation (FUT) and autologous non-cultured non-trypsinized epidermal cells grafting JT in stable vitiligo. He concluded that JT is somewhat superior to FUT in producing excellent and good repigmentation. Excellent repigmentation (>75%), at the end of 20 weeks post-surgery, was observed in 70% of lesions in the FUT group and 72% of lesions in the JT group. Good response (extent of repigmentation of 50–75%) was seen in 18% of lesions in the FUT group as compared to 26% in the JT group.
In another study by Verma et al.,6 she compared the JT with suction blister skin grafting (SBSG). She found that JT is superior to SBSG in the extent of repigmentation, color matching, DLQI, and patient satisfaction. Good pigmentation (>75%), at the end of 20 weeks post-surgery, was observed in 95% of patients in JT as compared to 83.75% in SBSG.
In our study out of 43 patches, 17 patches (39.53%) showed 90–100% (excellent) extent of repigmentation, and 19 patches (44.19%) showed 75–89% (good) extent of repigmentation. Thus, 83.72% of patches have >75% repigmentation. This result is comparable with previous studies done on JT.
Suction blisters have been described as both a means to prepare the recipient site and a technique for harvesting donor site tissue.7 This is one of the few studies to explore the role of suction blisters for recipient site preparation. A suction blister acts not only as a biological dressing but also has many added advantages. In another method of recipient site preparation, the epidermal grafts detach in about 1–2 weeks but it was observed that grafts could be attached permanently to the suction blister vitiligo sites. As the site of the splitting is at the dermoepidermal junction, it appears to yield a more favorable microenvironment for subsequent melanocyte grafting. A suction blister also prevents spilling of the grafted material and facilitates cohesive repigmentation. Further, the process of suction blister formation itself has a role in stimulating melanocytes. This observation suggests that the use of suction blisters for the recipient site in epidermal grafting for vitiligo might be better than the other currently available methods.8,9
Other methods for induction of blisters at the recipient site includes cryoblister and phototoxic blisters which are using psoralen and ultraviolet A (PUVA). Cryoblister uses liquid nitrogen which induces a blister after 24 h. It is associated with the side effect of peripheral dyschromia and hypertrophic scarring.10
PUVA blisters have the advantage of being time efficient, with no risk of scarring, and can be used for large areas. There is however a risk of carcinogenesis which cannot be ruled out.11
Our results are almost comparable to the study by van Geel et al.12 using the non-cultured epidermal cellular grafting technique reported more than 75% re-pigmentation in 71% of patients. Pandya et al.13 reported an excellent response in 52.17% of cases with the AMRCS (autologous melanocyte rich cell suspension) technique and in 50% with the MC (melanocyte culture) technique. Mulekar et al.14 used an autologous non-cultured trypsinized cellular grafting technique and reported more than 65% re-pigmentation in 61% of patients. Maleki et al.,15 in their pilot study on suction blister grafting technique, reported complete re-pigmentation in 70% of the cases. Gauthier and Surleve-Bazeille16 observed 70% repigmentation in 63.6% of the patients with vitiligo treated by non-cultured melanocyte transplantation. They had included only patients with focal and segmental vitiligo. Budania et al.17 found excellent (showing 90–100% repigmentation) in 71% of lesions in the non cultured epidermal suspension (NCES) group and 27% of lesions in the Suction blister epidermal grafting (SBEG) group (P = 0•002). Repigmentation ≥75% (good repigmentation) was observed in 89% of lesions in the NCES group and 85% of lesions in the SBEG group (P = 0•61).
Our study indicates that combining JT with a suction blister at the recipient site is a comparatively effective technique in terms of repigmentation, color match, and side effects.
Limitation
The main limitation of the procedure is that it is difficult to treat large areas and the process is time-consuming.
CONCLUSION
JT in itself is a simple, inexpensive, and effective technique. In our study, we modify recipient site preparation using the suction blister technique. This modification helps in evolving the traditional JT and provides better color matching and cohesive repigmentation. This technique is especially useful in treating small and stable lesions.
Authors’ Contributions
Harshvardhan Singh: literature search, clinical study, data acquisition and manuscript preparation. Chinmai Yadav: data analysis, manuscript preparation and editing. Rahul Singrodia: literature search, data acquisition. Dilip Kachhawa: concept, design, manuscript editing and guarantor. Pankaj Rao: manuscript preparation and review, manuscript editing.
Ethical approval
The research/study approved by the Institutional Review Board at Sampurnanand Medical College-, number -SNMC/IEC/2021/1221-1223, dated -10.02.2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Video available on:
Financial support and sponsorship
Nil.
References
- A comparative study between follicular unit transplantation and autologous non-cultured non-trypsinized epidermal cells grafting (Jodhpur technique) in stable vitiligo. J Cutan Aesthet Surg. 2020;13:204-9.
- [CrossRef] [PubMed] [Google Scholar]
- Suction blister epidermal grafting In: Gupta S, Olsson MJ, Kanwar AJ, Ortonne JP, eds. Surgical management of vitiligo (1st ed). Oxford UK: Blackwell; 2007. p. :96-107.
- [CrossRef] [PubMed] [Google Scholar]
- Clinico-epidemiological profile of patients with Vitiligo: A retrospective study from a tertiary care center of North India. Indian Dermatol Online J. 2019;10:38-44.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermal grafting in vitiligo: Influence of age, site of lesion, and type of disease on outcome. J Am Acad Dermatol. 2003;49:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Simplified non-cultured nontrypsinised epidermal cell graft technique followed by psoralen and ultraviolet a light therapy for stable vitiligo. J Cutan Aesthet Surg. 2017;10:81-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tertiary health care-based randomized controlled study to compare autologous, non-cultured, non-trypsinized epidermal cell transplant (jodhpur technique) with split-thickness skin grafting (STSG) in stable vitiligo. J Cutan Aesthet Surg. 2022;15:33-9.
- [CrossRef] [PubMed] [Google Scholar]
- Role of recipient-site preparation techniques and post-operative wound dressing in the surgical management of vitiligo. J Cutan Aesthet Surg. 2015;8:79-87.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of recipient site preparations in epidermal grafting for vitiligo: Suction blister and CO2 laser. J Eur Acad Dermatol Venereol. 2009;23:1448-9.
- [CrossRef] [PubMed] [Google Scholar]
- The use of suction blisters for recipient site in epidermal grafting: The implications for vitiligo. J Eur Acad Dermatol Venereol. 2009;23:241-2.
- [CrossRef] [Google Scholar]
- Treatment of stable vitiligo with autologous epidermal grafting and PUVA. J Am Acad Dermatol. 1995;32:943-8.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of squamous cell and basal cell cancer associated with psoralen and ultraviolet A therapy: A 30-year prospective study. J Am Acad Dermatol. 2012;66:553-62.
- [CrossRef] [PubMed] [Google Scholar]
- A review of non-cultured epidermal cellular grafting in vitiligo. J Cutan Aesthet Surg. 2011;4:17-22.
- [CrossRef] [PubMed] [Google Scholar]
- A study of autologous melanocyte transfer in treatment of stable vitiligo. Indian J Dermatol Venereol Leprol. 2005;71:393-7.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of vitiligo on difficult-to-treat sites using autologous noncultured cellular grafting. Dermatol Surg. 2009;35:66-71.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of suction blister epidermal graft without phototherapy for locally stable and resistant vitiligo. Indian J Dermatol. 2012;57:282-4.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol. 1992;26:191-4.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of two surgical modalities in stable vitiligo: A randomized study. Br J Dermatol. 2012;167:1295-301.
- [CrossRef] [PubMed] [Google Scholar]







