Translate this page into:
Treatment of Acne Keloidalis Nuchae by Simply Combining Two Conventionally Available Modalities: Ablation with Carbon Dioxide Laser and Intralesional Triamcinolone Acetonide
Address for correspondence: Dr. Yogesh M. Bhingradia, Department of Dermatology, Shivani Skin Care and Cosmetic Clinic, Surat 395006, Gujarat, India. E-mail: yogeshbhingradia@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Acne keloidalis nuchae is a chronic inflammatory condition affecting the occipital area or nape of the neck characterized by fibrotic papules, firm pustules, and nodules that coalesce into keloid like mass or plaques. It was first described by Kaposi in 1969. It is also known as lichen keloidalis nuchae, dermatitis papillaris capillitia, and folliculitis nuchae scleroticans. If not treated in the early stages of the disease it tends to be refractory to conventional methods like topical, intralesional steroids with antibiotics or retinoids. Surgical interventions remain the only choice in such cases. Various surgical modalities including surgical excision with primary or secondary closure, split-thickness skin grafts, and laser-assisted treatments have been tried. Most surgical methods have longer downtime with a higher chance of relapse. We studied the results of a combined treatment option carbon dioxide laser ablation followed by intralesional triamcinolone injection in the same sitting. This outpatient procedure has shown good results with no relapse and less downtime.
Keywords
Acne keloidalis nuchae
carbon dioxide laser
intralesional triamcinolone
INTRODUCTION
Acne keloidalis nuchae (AKN) is characterized by the presence of millimetric follicular papules, which are firm to touch and can be scabby, umbilicated, or pustular, with hair within them. The papules–pustules can give rise to plaques with a keloidal appearance and nodules that can present purulent secretion. It is a chronic inflammatory condition characterized by fibrotic papules and nodules of the nape of the neck over the occiput with the incidence of 0.45%–9%. Male to female ratio is 20:1 with a predisposition in dark-skinned individuals with curly or kinky hair.[12] It starts with the formation of inflamed papules with marked erythema. Over time, continued inflammation causes pronounced fibrosis and keloid formation with the coalescence of the papules into large plaques and nodules on the occipital scalp and posterior neck.[34]
Treatment for early stages of AKN mostly involves preventive measures for disease progression like avoidance of mechanical irritation from clothing and moist compresses and antimicrobial cleansers to prevent secondary infection.[5] Topical, intralesional, or systemic steroids in combination with retinoids and/or antibiotics to decrease inflammation are traditionally been used in treatment.[67] If the disease progresses to a late stage or the patient presents at a late stage some form of surgical intervention is warranted. Options include recent advances like light and laser therapies, electrosurgery and radiation therapy,[8] and surgical excision with primary or secondary closure or split-thickness skin grafts.[9] All modalities have their limitations; surgical excision requires long healing periods, and other minimally invasive methods provide suboptimal outcomes with either recurrence or no effect. In this case series, we have demonstrated the treatment of AKN with the carbon dioxide (CO2) laser in combination with intralesional steroids with rewarding results and minimum healing time.
MATERIALS AND METHODS
A case series was carried out on seven male patients who came to our out patient department with recalcitrant AKN lesions with an average duration of disease of 11.5 years. All our patients were male patients with an average age of 32.8 years.
All our patients had tried most medical line of management including oral isotretinoin, topical retinoid, and also intralesional steroid injections with suboptimal results [Table 1].
| Patient no. | Age | Gender | Duration | Size of largest lesion | Previous treatment | CO2-ablative number of sittings + ILS | Complains |
|---|---|---|---|---|---|---|---|
| 1 | 32 | Male | 11 years | 8 mm | ILS, isotretinoin, LN2 | 2 | Pain |
| 2 | 38 | Male | 16 years | 10 mm | LN2, topical retinoid, ILS | 3 | Pain swelling |
| 3 | 28 | Male | 9 years | 6 mm | ILS | 1 | – |
| 4 | 37 | Male | 11 years | Multiple coalescing to form 20 mm | ILS, isotretinoin | 4 | Pain itching |
| 5 | 35 | Male | 14 years | 9 mm | ILS, isotretinoin, LN2 | 3 | Pain |
| 6 | 28 | Male | 8 years | 8 mm | ILS, isotretinoin, LN2 | 2 | Headache |
| 7 | 32 | Male | 12 years | 10 mm | ILS, isotretinoin, LN2 | 3 | Pain |
ILS = intralesional steroid, LN2 = liquid nitrogen
Treatment protocol: [Video 1]
The area to be treated was trimmed for a clear surgical field.
After aseptic precautions local anesthetic agent; 2% lignocaine with adrenaline (1:10,000) was injected in all the lesions.
CO2 laser with focused continuous ablative mode with energy 130–150 J/cm2.
The direction of the CO2 laser beam in the direction of the hair follicle to reach fibrotic tissue of the deep dermis or subcutaneous tissue. The entire lesion was ablated in continuous repetitive circular motions.
Injection triamcinolone acetonide 40 mg/mL was injected at the base of each lesion. A maximum of 2 mL was used in each sitting.
Total three sessions of CO2 laser ablation and intralesional triamcinolone acetonide were done at intervals of 8 weeks. Out of the seven patients, only one patient who had coalescing large lesions required a fourth sitting.
Antibiotics, analgesics, and topical antibiotic cream were advised for 7 days, and follow-up analysis was done at 1, 3, and 8 weeks after the procedure.
Decision about repeat session was taken by evaluating the lesions at 8 weeks.
Evaluation
Each patient was evaluated clinically at the baseline and after every sitting to analyze the efficacy of the procedure.
Photographic documentation was done using a standardized high-resolution camera (iPhone 13S) before starting the treatment and before every sitting. Due consents were taken for the same.
The follow-photographs were taken after 6 months after the last sitting. The duration of the study was 2 years.
RESULTS
Six patients showed significant response with more than 90% resolution at the end of three sessions and one after the fourth session.
Treatment was well tolerated, and all patients completed both CO2 laser and intralesional steroid sessions.
Close follow-up up to 6 months was done after last triamcinolone injection and no patient reported any recurrence [Figures 1 and 2].
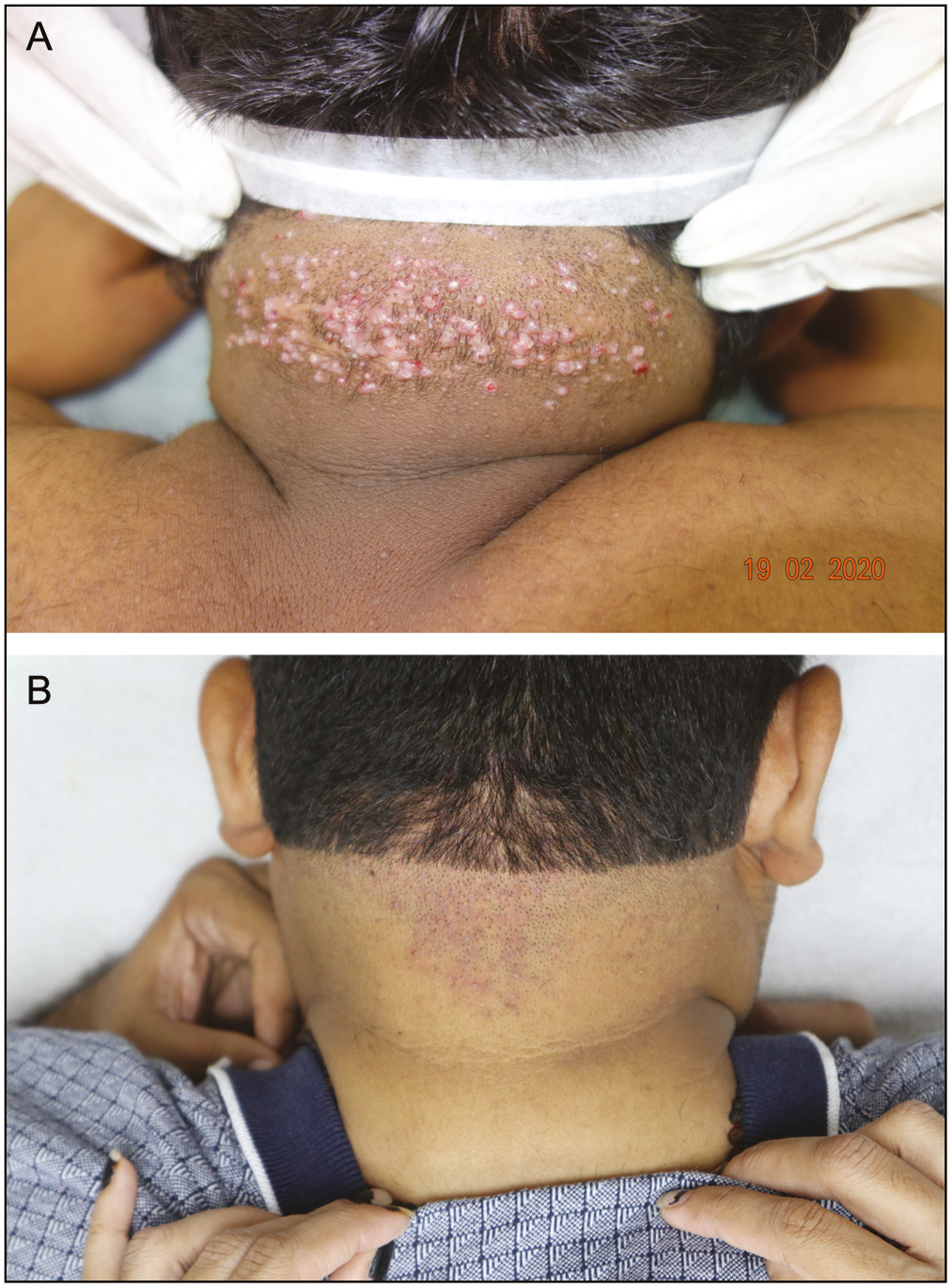
- (A) Multiple keloidal nodules over the nape of the neck. (B) Complete resolution of the lesions after 3 sessions and 6 months after end of all treatment sessions

- (A) Multiple keloidal nodules over the nape of the neck. (B) Complete resolution of the lesions 6 months after end of all treatment sessions
DISCUSSION
The term AKN is considered a misnomer as it refers to an entity that is not related to acne vulgaris and is not characterized by keloid lesions but rather hypertrophic lesions.[10]
AKN is a chronic condition leading to physical and cosmetic discomfort to the patients as it occurs around the nape of the neck and occiput. If not treated, it leads to the formation of large plaques, keloidal nodules, and even scarring alopecia. With conventional treatment options or even with laser therapy, there are chances of improper resolution and frequent relapses.[15,6] They are refractory to most treatment modalities. CO2 laser emits far infrared light of wavelength 10,600 nm. It uses water as a chromophore and vaporizes water in keloid tissue leading to the reduction or evaporation of lesions.[11]
Histopathology shows folliculitis with inflammatory granulomatous infiltrate rich in neutrophils and lymphocytes situated in the lower part of the isthmus suggesting an ongoing inflammatory process.[10] Sebaceous glands are destroyed in the early stages of this process. The damaged follicle finally releases its hair shaft to the surrounding dermis leading to an acute and chronic granulomatous reaction, responsible for the clinical manifestation of papules with a firm consistency. The damaged hair shafts cannot be eliminated because of the involvement of the upper part of the follicle, thereby increasing the inflammatory and granulomatous reaction, with a continuous reparative process triggering that finally leads to hypertrophic scarring. This implies that only CO2 laser ablation is not sufficient for halting the pathogenesis of scarring which may lead to relapse. In a case reported by Kraeva et al.,[12] they demonstrated treating keloid with fractional CO2 and laser-assisted drug delivery of triamcinolone acetonide ointment. There are no studies where ablative CO2 and intralesional steroid were combined simultaneously in the same sitting.
Other methods like electrosurgery and dermabrasion, have been documented to have relapses or formation of hypertrophic scars in follow-ups.[913] Surgical excision with primary closure or split-thickness skin grafts has shown good results but few incidences of relapse are documented and these procedures often involve downtime of around 2–3 weeks for patients with chances of secondary infection.[18,14] There are also studies where large AKN were excised and left to heal by secondary intention.[15] But both these methods require long downtime. Frequent dressing and high chances of secondary infection can further delay the healing process. Combining ablative CO2 with intralesional triamcinolone acetonide can overcome these events.
LIMITATION
It was a small case series that was carried out in a private setup. A large multicentric study would help us analyze a larger group with better insight into the outcomes.
No metric documentation was done. Mean papule, pustule count, or keloidal plaque size with standardization of procedure will help calculate the exact score and treatment outcome.
CONCLUSION
CO2 laser ablation combined with intralesional triamcinolone can be an effective treatment option in AKN comprising large plaques and keloidal nodules. Both these procedures are carried out by most dermatosurgeons individually but combining them in the same sitting is a novel approach that has helped us optimize the results. Resolution of plaques and nodules with good cosmetic appearance, no relapse, and almost no downtime was seen in our patients with this simple outpatient procedure.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
All videos available online www.jcasonline.com
REFERENCES
- Treatment of acne keloidalis nuchae: A systematic review of the literature. Dermatol Ther. 2016;6:363-78.
- [Google Scholar]
- Pseudofolliculitis barbae and acne keloidalis nuchae. Dermatol Clin. 2003;21:645-53.
- [Google Scholar]
- Acne Keloidalis Nuchae. 2023. StatPearls. Treasure Island (FL): StatPearls Publishing; Available from: https://www.ncbi.nlm.nih.gov/books/NBK459135/">https://www.ncbi.nlm.nih.gov/books/NBK459135/
- [Google Scholar]
- Acne keloidalis nuchae: Prevalence, impact, and management challenges. Clin Cosmet Investig Dermatol. 2016;9:483-9.
- [Google Scholar]
- Folliculitis keloidalis nuchae and pseudofolliculitis barbae: Are prevention and effective treatment within reach? Dermatol Clin. 2014;32:183-91.
- [Google Scholar]
- Keratosis follicularis spinulosa decalvans and acne keloidalis nuchae. Australas J Dermatol. 2005;46:257-60.
- [Google Scholar]
- Electrosurgical excision of acne keloidalis nuchae with secondary intention healing. J Clin Aesth Dermatol. 2011;4:36-9.
- [Google Scholar]
- Acne keloidalis nuchae: Treatment with excision and second-intention healing. J Am Acad Dermatol. 1995;33:243-6.
- [Google Scholar]
- Histologic features of alopecias: Part II: Scarring alopecias. Actas Dermosifiliogr. 2015;106:260-70.
- [Google Scholar]
- Successful treatment of keloid with fractionated carbon dioxide (CO2) laser and laser-assisted drug delivery of triamcinolone acetonide ointment in an African-American man. J Drugs Dermatol. 2017;16:925-7.
- [Google Scholar]
- Acne keloidalis is a form of primary scarring alopecia. Arch Dermatol. 2000;136:479-84.
- [Google Scholar]
- Surgical excision of acne keloidalis nuchae with secondary intention healing. Clin Exp Dermatol. 2008;33:53-5.
- [Google Scholar]






