Translate this page into:
Treatment of Localized Granuloma Annulare with the 595-nm Pulsed Dye Laser
Address for correspondence: Dr. Catarina Correia, Department of Dermatology, Centro Hospitalar Universitário Lisboa Norte, 1649-028 Lisboa, Portugal. E-mail: catarinacorreia03@gmail.com
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Dear Editor,
Granuloma annulare (GA) is a benign idiopathic inflammatory granulomatous skin disease that can affect individuals of all ages, with a predilection for women (3:1). It often presents on the dorsum of the hands and feet, with annular groups of skin-colored to red‒brown papules. GA encompasses five distinct clinical forms: localized, generalized, perforating, patchy, and subcutaneous. Despite the availability of numerous treatment methods, the search for a consistent and long-term solution remains challenging.[12]
In this article, we present a case of an annular granuloma located on the back that was resistant to topical and intralesional corticosteroids, topical calcineurin inhibitors, and phototherapy. Remarkably, complete resolution of the granuloma was achieved after two treatments with a 585 nm pulsed dye laser (PDL).
A healthy 60-year-old woman, Fitzpatrick phototype II, presented with a three-year history of three asymptomatic erythematous plaques on her back. Despite prior treatment attempts with topical and intralesional corticosteroids, topical calcineurin inhibitors, and phototherapy, there was no improvement. Physical examination revealed three erythematous-violaceous plaques arranged in an annular configuration [Figure 1A and B]. A skin biopsy confirmed the diagnosis of GA. The patient underwent two treatment sessions with a 595 nm PDL with a two-month interval between sessions. The laser settings used were as follows: 7 mm spot size, 0.5 ms pulse duration, and 8 J/cm2 fluence, with continuous forced-air cooling. Remarkably, complete resolution of the skin lesions was achieved [Figure 1D]. There were no complications. During the one-year follow-up period, there was no recurrence of the lesions.
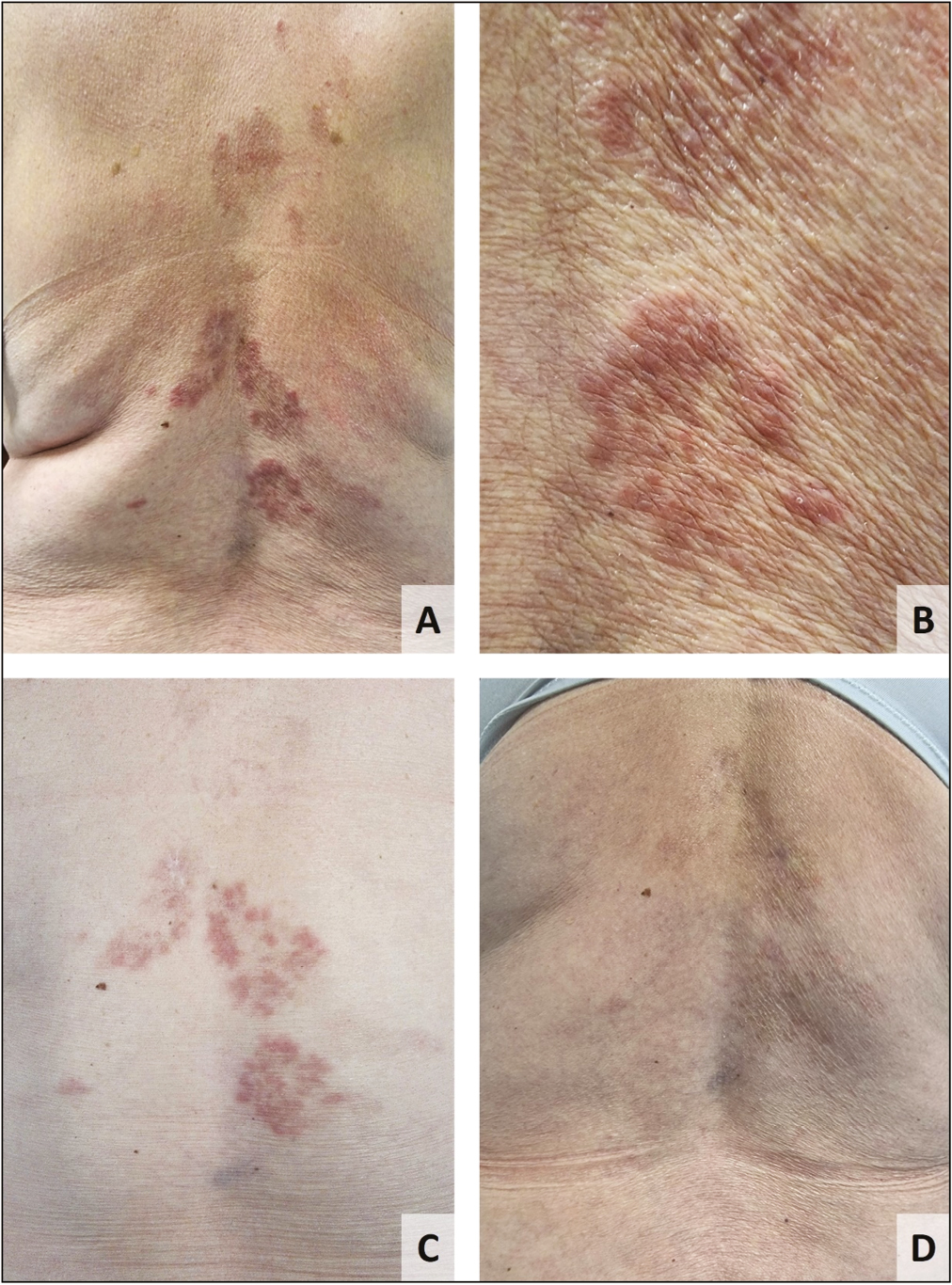
- Granuloma annulare, clinical images: (A) erythematous-violaceous plaques arranged in an annular configuration on the back; (B) clinical photography after the first PDL session; (C) complete resolution of granuloma annulare after 2 PDL sessions
Numerous therapies have been employed in treating GA, with varying degrees of efficacy reported. These treatments include topical, systemic, and intralesional corticosteroids, topical calcineurin inhibitors, phototherapy, antimicrobials, antimalarials, apremilast, methotrexate, pentoxifylline, biologic therapies, and tofacitinib, among others.[2] Additionally, the PDL, the CO2 laser, the Nd:YAG laser, and the excimer laser have each been used to treat GA, with varying success rates.[13]
The pulsed dye laser is considered the treatment of choice for various cutaneous vascular and nonvascular lesions. However, few case reports and only one retrospective study have documented the use of PDL treatment for GA.[34] In that retrospective study, 56.2% of localized GA lesions showed improvement after three sessions, with no recurrence after 6 months. Nevertheless, generalized GA has been reported to show a weak response to PDL treatment and high recurrence rates.[1]
Taking into account our case report and the existing literature, we propose that PDL therapy should be considered, like topical and intralesional corticosteroids, a first-line therapy for the treatment of localized GA, particularly in cases with significant erythema. This therapeutic modality has demonstrated substantial efficacy with minimal complications (transient hyperpigmentation, crusting, and hypopigmentation), thereby avoiding the cutaneous and systemic adverse effects associated with corticosteroids and other systemic therapies.[13] Our findings highlight the potential of PDL therapy as an effective and well-tolerated treatment option for localized GA, with low recurrence rates. Further studies are needed to explore the long-term outcomes of PDL treatment and compare its efficacy with alternative therapies. The development of comprehensive guidelines is warranted to establish standardized protocols for managing the various subtypes of granuloma annulare.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
None.
REFERENCES
- Treatment of granuloma annulare with the 595-nm pulsed dye laser, a multicentre retrospective study with long-term follow-up. J Eur Acad Dermatol Venereol. 2013;27:785-8.
- [Google Scholar]
- Granuloma annulare: An updated review of epidemiology, pathogenesis, and treatment options. Am J Clin Dermatol. 2022;23:37-50.
- [Google Scholar]
- Treatment of granuloma annulare with the 585 nm pulsed dye. Dermatolog Surg. 2005;31: 1370-3.
- [Google Scholar]





