Translate this page into:
Triple combination of fractional carbon dioxide laser, 308-nm excimer lamp, and platelet-rich plasma in refractory vitiligo: A randomized split-body comparative study
*Corresponding author: Mahin Aflatoonian, Clinical Research Development Unit, Afzalipour Hospital, Kerman University of Medical Sciences, Kerman, Iran. maaflatoonian@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khalili M, Solhjou S, Amiri R, Rukerd MRZ, Aflatoonian M. Triple combination of fractional carbon dioxide laser, 308-nm excimer lamp, and platelet-rich plasma in refractory vitiligo: A randomized split-body comparative study. J Cutan Aesthet Surg. 2025;18:34-41. doi: 10.25259/JCAS_16_2024
Abstract
Objectives:
Vitiligo significantly impacts patients’ quality of life. Current evidence indicates that combination therapy results in faster improvement, enhancing patient adherence to treatment and leading to higher satisfaction among patients. In this study, we compare the efficacy of combined fractional carbon dioxide (FCO2) laser and excimer lamp with platelet-rich plasma (PRP) or topical tacrolimus in patients with refractory vitiligo.
Material and Methods:
This is a prospective, single-blind, randomized split-body clinical trial involving 41 patients with resistant focal patches of vitiligo vulgaris. Each patient had two similar lesions randomly assigned to receive either a combination of FCO2 laser, excimer lamp, and intradermal PRP injections or a combination of FCO2 laser, excimer lamp, and topical 0.1% tacrolimus (applied twice daily for 12 weeks). The FCO2 laser and PRP treatments were administered in three monthly sessions, and the excimer lamp was used twice a week over 12 weeks. The efficacy of treatment was assessed based on the physician’s assessment and patient’s satisfaction
Results:
Despite significant improvement in both treatment groups during the course of treatment, the PRP group showed significantly superior efficacy (more than 50% improvement) compared to the tacrolimus group (56.1% and 26.8%, respectively). Furthermore, the PRP group exhibited greater improvement in resistant acral areas compared to the tacrolimus group (51.2% and 19.5%, respectively).
Conclusion:
The combination of FCO2, an excimer lamp, and PRP demonstrates superior efficacy, particularly in resistant acral areas. As a result, this combination can be recommended in difficult-to-treat areas in patients with vitiligo.
Keywords
Carbon dioxide laser
Excimer lamp
Platelet-rich plasma
Tacrolimus
Vitiligo
INTRODUCTION
Vitiligo, a commonly acquired pigmentary skin condition, is characterized by the autoimmune destruction of melanocytes. It manifests as depigmented skin lesions and significantly impacts patients’ quality of life.1-3 Current treatment modalities for vitiligo include topical therapies, phototherapy, laser and light devices, systemic therapies, and surgical therapies. The excimer laser/lamp and topical calcineurin inhibitors, such as tacrolimus, have been used to treat localized vitiligo. These treatments demonstrate anti-inflammatory effects by inducing T-cell apoptosis and reducing depigmented patches by stimulating melanocytes to proliferate, migrate, and produce more melanin pigment.4-6
In recent years, novel potential treatment modalities have emerged, including platelet-rich plasma (PRP) and the use of ablative laser treatment to enhance topical drug absorption.7-9 PRP contains growth factors such as platelet-derived growth factor, transforming growth factor-beta, basic fibroblast growth factor, vascular endothelial growth factor, and insulin-like growth factor, which stimulate melanocyte proliferation and melanin production. PRP also exhibits anti-inflammatory properties by inhibiting the production of inflammatory cytokines, such as tumor necrosis factor-alpha, interleukin-1, and interferon-gamma. In addition, PRP provides a supportive matrix composed of proteins such as fibrin, fibronectin, and vitronectin, which enhances the interaction of melanocytes with keratinocytes and fibroblasts.8-10 The fractional ablative laser stimulates melanocyte proliferation and migration from hair follicles and adjacent normal skin by up-regulating the levels of cytokines and growth factors, which activates matrix metalloproteinase (MMP)-2 and MMP-9. It also generates microthermal columns in the epidermis and dermis, which improves topical drug and ultraviolet-B (UVB) penetration. Furthermore, the denaturation of collagen bundles following the laser leads to tissue contraction and, as a result, a reduction in the size of the depigmented patch.10-14
According to current evidence, combination therapy results in faster repigmentation, increases patient adherence to treatment, and leads to higher patient satisfaction.10-12 Based on our knowledge, no clinical trial has evaluated the efficacy of a triple combination of fractional carbon dioxide (FCO2) laser, 308-nm excimer lamp, and PRP. Therefore, in this study, we compare the efficacy of a combined FCO2 laser and 308-nm excimer lamp with either PRP or topical tacrolimus in patients with resistant focal patches of vitiligo vulgaris.
MATERIAL AND METHODS
Study design
This is a prospective, single-blind, randomized, and split-body comparative clinical trial on eight-two vitiligo lesions. This study was approved by the ethical committee of Kerman Medical Sciences with the ethical code of IR.KMU. AH.REC.1399.165 and registered in the Iranian clinical trial registry system with registry code IRCT20210125050139N1. Based on the current evidence, no study has investigated the effectiveness of these two methods in vitiligo patients. Therefore, a preliminary pilot study involving 20 lesions (10 patients with symmetrical lesions) was conducted. The excellent effectiveness in PRP and tacrolimus groups at the end of the third session was 27.5% and 0.3%, respectively. A sample size of 41 lesions in each group was estimated using the sample size formula to compare two ratios (alpha = 0.0500 [two-sided], power = 0.8000, n2/n1 = 1.00). Thereby, 41 patients were randomly enrolled in the study.
The inclusion criteria were patients with focal patches of vitiligo vulgaris resistant to previous treatments (having shown no response to conventional treatment modalities for at least 6 months). Exclusion criteria include patients who received narrow-band UVB (NB-UVB), corticosteroids, or any immunosuppressive therapy within the past 6 months; those younger than 18 years old; patients in the unstable phase of vitiligo (development of new lesions or spreading of previous lesions within the past 6 months); those with segmental vitiligo; involvement of more than 20% of body surface area; history of keloids; positive Koebner phenomenon; pregnancy; lactation; anemia (hemoglobin <10 g/dL); thrombocytopenia (platelets <150,000/mm3); use of any anticoagulant or antiplatelet drugs; sensitivity to photosensitivity; and coagulative, neoplastic, infectious, or serious systemic diseases.
First, after explaining the treatment methods and possible side effects, informed consent was obtained from all participants. Vitiligo was diagnosed based on clinical features, and Wood’s lamp was used to confirm the diagnosis in suspicious cases. Following that, demographic information of the patients (age, gender, and skin type) and clinical characteristics (duration, location, and size of the lesions) were recorded. Next, two lesions in symmetrical sites of the body with nearly similar sizes were randomly chosen for treatment in each patient (using simple randomization by flipping a coin). The randomization and enrollment of participants into treatment groups were conducted by a dermatologist not involved in evaluating treatment responses. Both assessors and analysts were blinded to the type of treatment modalities.
Group 1: Combined FCO2 laser, excimer lamp, and PRP
The fractional laser (SmartXide2; DEKA Laser, Florence, Italy, 10600 nm) was administered in three monthly sessions. Initially, topical anesthetic cream (Xyla-P, Tehran Chemie Pharmaceutical Co.) was applied under occlusion for 45 min. Then, the skin was sterilized with 70% ethanol after washing with soap and water. After ethanol evaporation, laser treatment was applied to the depigmented patch and a 1 mm margin from surrounding normal skin. The laser settings were as follows: 6 watts, 550 µm spacing, 400 µs dwell time, and single stack. These settings (low power along with high density) are suitable to produce intra-epidermal microchannels to enhance penetration of the topical drug.9,11,12
The excimer laser (Medflash II, Italy, 308 nm) was used biweekly, starting 1 week after FCO2 laser treatment, and continued for 3 months. The initial dose was 0.5 j/cm2, with increments of 0.1 j/cm2 per session. If symptoms such as pain, blistering, or prolonged erythema (lasting more than 48 h) occurred at the treatment site, laser sessions were paused for 1–2 sessions until improvement, after which the previous dose was resumed. Protective glasses were worn during the laser procedure, and sunblock cream was applied to protect the surrounding skin.
To prepare PRP, 10 cc of venous blood was collected from each patient and placed in a sterile tube containing sodium citrate. The blood was then centrifuged (RooyaGen kit, Tehran, Iran) for 14 min at 1950 revolutions per minute (rpm). The upper layer containing plasma was separated from the bottom layer (red blood cells) into a separate tube and centrifuged at 1450 rpm for 9 min. Finally, the lower layer was transferred to an insulin syringe containing calcium chloride as an activator in a 9:1 ratio.11 The final volume of PRP product was 10% of the initial blood volume that, yielded platelet concentration of approximately more than 4 times of initial whole blood.8 Patients were given topical anesthetic cream for 45 min before injections. PRP was injected intradermally (0.1 cc/cm2, maximum 1cc/session) 1 week after the FCO2 laser session, conducted in three monthly sessions.
Group 2: Combined FCO2 laser, excimer lamp, and topical tacrolimus 0.1%
As previously mentioned, the depigmented patch was treated with an FCO2 laser. Following the laser treatment, patients were instructed to apply 0.1% tacrolimus ointment twice daily for 12 weeks. The excimer lamp was then performed 1 week after the FCO2 laser, as described previously.
Follow-up sessions
Patients in both treatment groups were instructed to continue applying topical tacrolimus twice daily and undergoing excimer treatments twice a week as maintenance therapy at the end of the treatment course. Participants were followed up for recurrence rates up to 6 months after the completion of treatment.
Evaluation of treatment efficacy and relapse rate
Photographs were taken of each lesion at monthly intervals using a digital camera (SX410IS, Canon, Tokyo, Japan). The response rate was assessed by two independent blinded dermatologists at the 4th, 8th, and 12th months of treatment. The physician response rate was classified as excellent (more than 75%), marked (50–75%), moderate (25–49%), and poor (<25%), based on the percentage of repigmentation. At the 6-month follow-up session, patients rated their satisfaction using a visual analog scale (VAS) ranging from 0 (unsatisfied) to 10 (completely satisfied). In addition, the type of repigmentation (follicular, peripheral, and diffuse) was noted during each treatment session. At the end of treatment, patients were queried about side effects such as pain, erythema, pruritus, and post-inflammatory hyperpigmentation.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences version 24 (IBM Corp., Armonk, NY, USA). Quantitative data were described using mean (± standard deviation), while qualitative data were summarized using frequencies. The Chi-square test and independent t-test were employed to assess relationships between treatment efficacy and qualitative and quantitative patient characteristics, respectively. The Cochran Q test was used to evaluate treatment outcomes over the treatment period. The analysis of variance was used to assess treatment outcomes based on the duration of lesions. The Chi-square test and independent t-test were also used to determine treatment efficacy based on physician’s evaluation and patient satisfaction.
RESULTS
At the beginning of the study, 41 patients were evaluated, and all of them completed the treatment course and follow-up sessions [Figure 1]. The mean age of the patients was 41.48 ± 9.46 years (range: 20–56 years). The majority of participants (65.9%) were female. The patients had skin type IV (53.7%) and type III (46.3%). The mean duration of the disease was 10.53 ± 6.77 months (range: 7–28 months). Lesions were located in acral areas (90.2%) and extremities (9.8%). In both treatment groups, the majority of lesions were <5 cm2 in size.
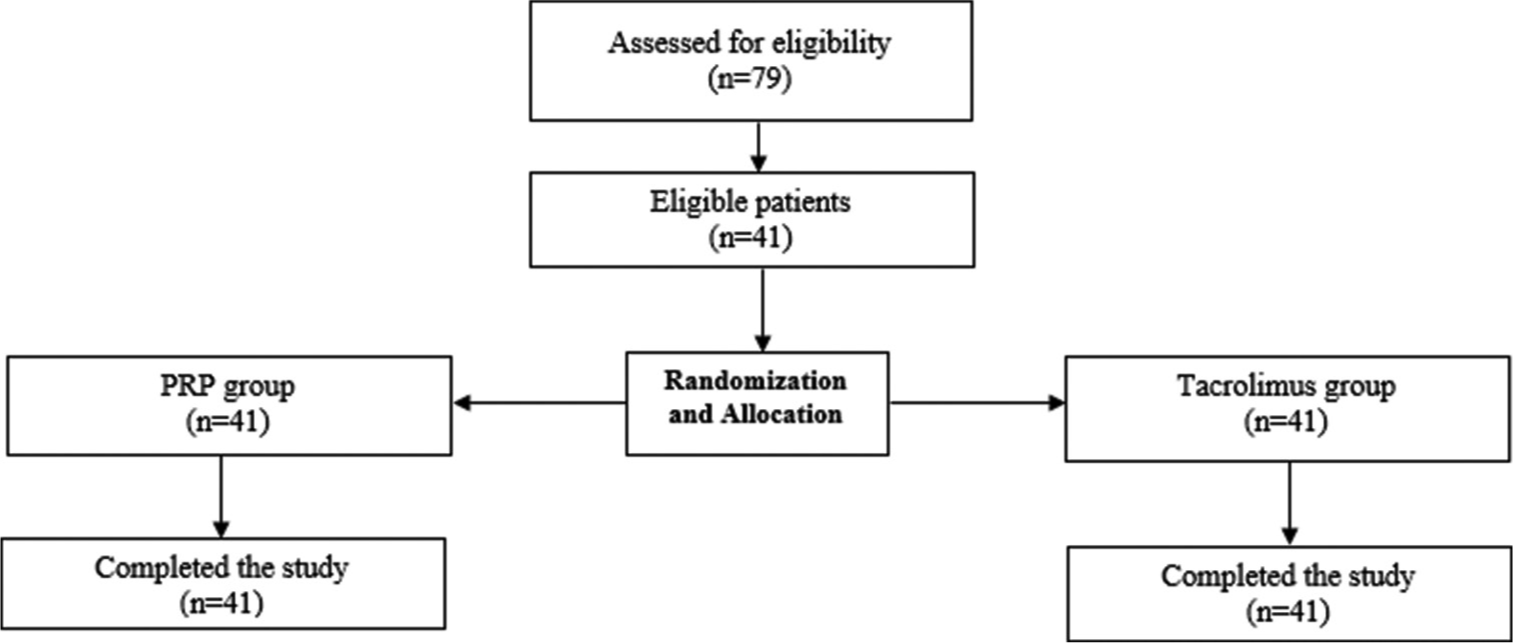
- Flow diagram of the case selection of the study. PRP: Platelet-rich plasma
Treatment response based on physician evaluation
The vitiligo lesions improved significantly in both treatment groups (P = 0.001). There was no statistically significant difference in the response rate between the two groups at the 4th and 8th weeks of treatment; however, the superior response was observed in the PRP group compared to the tacrolimus group at the 12th week of treatment (P = 0.002, [Table 1]). Furthermore, the PRP group demonstrated higher improvement in resistant acral areas compared to the tacrolimus group (51.2% and 19.5%, respectively). In both treatment groups, there was no significant difference in the percentage of improvement based on variables such as lesion size and duration, as well as patient gender [Tables 2 and 3]. In both groups, 19.5% of cases had perifollicular repigmentation. Only 1 case (2.4%) in the PRP group had both diffuse and peripheral repigmentation. Others had diffuse repigmentation (78% in the PRP group and 80.5% in the tacrolimus group). Among all 41 patients, [Figures 2 and 3], as examples, present a comparison between two groups based on treatment response as evaluated by physicians.
| Treatment sessions | Degree of improvement | Excimer laser+FCO2 laser+PRP (n=41) |
Excimer laser+FCO2 laser+tacrolimus (n=41) |
P-value |
|---|---|---|---|---|
| n(%) | n(%) | |||
| First session | Poor | 27 (65.9) | 32 (78) | 0.21 |
| Moderate | 14 (34.1) | 9 (22) | ||
| Marked | 0 (0) | 0 (0) | ||
| Excellent | 0 (0) | 0 (0) | ||
| Second session | Poor | 13 (31.7) | 22 (53.7) | 0.15 |
| Moderate | 17 (41.5) | 14 (34.1) | ||
| Marked | 10 (24.4) | 5 (12.2) | ||
| Excellent | 1 (2.4) | 0 (0) | ||
| Third session | Poor | 5 (12.2) | 13 (31.7) | 0.002 |
| Moderate | 13 (31.7) | 17 (41.5) | ||
| Marked | 12 (29.3) | 11 (26.8) | ||
| Excellent | 11 (26.8) | 0 (0) | ||
| P-value | 0.001 | 0.001 |
FCO2:Fractional carbon dioxide, PRP: Platelet-rich plasma
| Variables | Degree of improvement | ||||
|---|---|---|---|---|---|
| Poor | Moderate | Marked | Excellent | P-value | |
| Site of the lesions | |||||
| Extremities, n(%) | 0 (0) | 2 (50) | 0 (0) | 2 (50) | 0.48 |
| Acral, n(%) | 5 (13.5) | 11 (29.8) | 12 (32.4) | 9 (24.3) | |
| Size of the lesions | |||||
| <5 cm, n(%) | 4 (13.3) | 11 (36.7) | 8 (26.7) | 7 (23.3) | 0.62 |
| >5 cm, n(%) | 1 (9.1) | 2 (18.1) | 4 (36.4) | 4 (36.4) | |
| Sex | |||||
| Male, n(%) | 0 (0) | 6 (42.9) | 5 (35.7) | 3 (21.4) | 0.26 |
| Female, n(%) | 5 (18.5) | 7 (25.9) | 7 (25.9) | 8 (29.7) | |
| Mean duration, months | 11.8±4.49 | 9.46±6.35 | 8.41±3.23 | 13.54±9.90 | 0.28 |
PRP: Platelet-rich plasma
| Variables | Degree of improvement | ||||
|---|---|---|---|---|---|
| Poor | Moderate | Marked | Excellent | P-value | |
| Site of the lesions | |||||
| Extremities, n(%) | 0 (0) | 1 (25) | 3 (75) | 0 (0) | 0.03 |
| Acral, n(%) | 13 (35.1) | 16 (43.2) | 8 (21.7) | 0 (0) | |
| Size of the lesions | |||||
| <5 cm, n(%) | 12 (37.5) | 14 (43.8) | 6 (18.7) | 0 (0) | 0.07 |
| >5 cm, n(%) | 1 (11.1) | 3 (33.3) | 5 (55.6) | 0 (0) | |
| Sex | |||||
| Male, n(%) | 6 (42.9) | 5 (35.7) | 3 (21.4) | 0 (0) | 0.54 |
| Female, n(%) | 7 (25.9) | 12 (44.4) | 8 (29.7) | 0 (0) | |
| Mean duration, Months | 11.38±5.26 | 8.52±4.15 | 12.63±10.5 | 0 (0) | 0.25 |
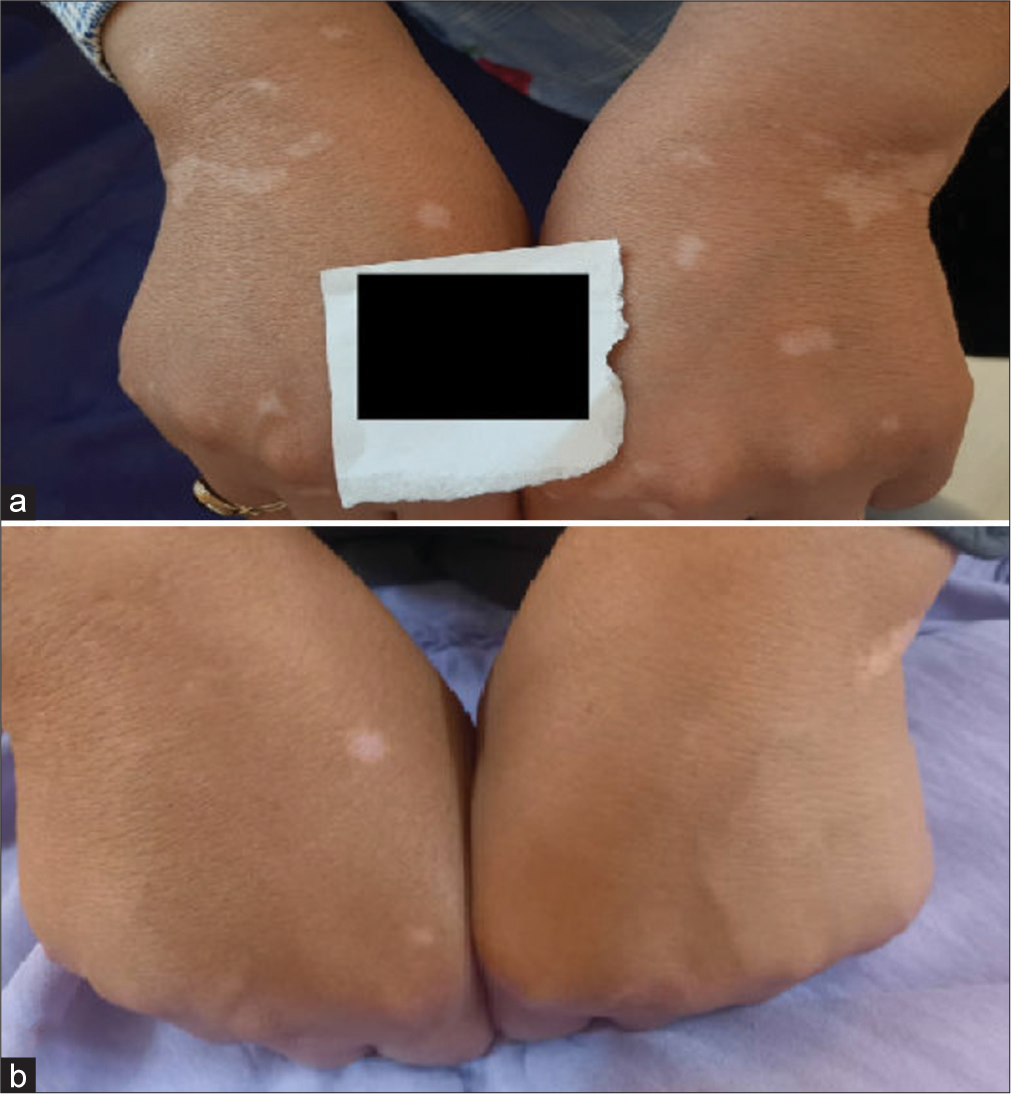
- (a) Clinical photographs of a 51-year-old female with refractory vitiligo lesions on both hands before treatment and (b) six months after the final treatment session. The patient’s right hand treated with a combination of fractional carbon dioxide (FCO2) laser, excimer lamp therapy, and platelet-rich plasma demonstrates >75% repigmentation. The patient’s left hand was treated with a combination of FCO2 laser, excimer lamp therapy, and topical tacrolimus 0.1% shows between 50% and 75% repigmentation.

- (a) Clinical photographs of a 56-year-old male with refractory vitiligo lesions on both hands before treatment and (b) six months after the final treatment session. The patient’s right hand treated with a combination of fractional carbon dioxide (FCO2) laser, excimer lamp therapy, and platelet-rich plasma demonstrates >75% repigmentation. The patient’s left hand was treated with a combination of FCO2 laser, excimer lamp therapy, and topical tacrolimus 0.1% shows between 50% and 75% repigmentation.
Treatment response based on patients’ satisfaction
Patients in the PRP group reported significantly higher satisfaction with the treatment results compared to those in the tacrolimus group (P = 0.001). The mean VAS scores for participants in the PRP and tacrolimus groups were 6.95 ± 1.82 (median 7, range 3–10) and 5.56 ± 1.46 (median 6, range 2–8), respectively.
Follow-up session
Patients were followed for 6 months after completing the treatment course, and no relapse or worsening of the lesions was reported in any of the treatment groups.
Side effects of treatment
No serious side effects were reported in any of the patients in both treatment groups. Burning sensation, erythema, and skin dryness were observed in both groups; however, the difference was not statistically significant (P = 0.51, [Table 4]).
| Side effects | Excimer laser+FCO2 laser+PRP (n=41) | Excimer laser+FCO2 laser+tacrolimus (n=41) | P-value |
|---|---|---|---|
| n(%) | n(%) | ||
| Pruritus | 3 (50) | 3 (50) | 0.51 |
| Erythema | 4 (57.1) | 3 (42.9) | |
| Peeling | 2 (25) | 6 (75) |
FCO2: Fractional carbon dioxide, PRP: Platelet-rich plasma
DISCUSSION
Vitiligo affecting acral areas and bony prominences is a refractory disease due to the sparse number of hair follicles and melanocytes reservoir in these regions. Hence, long-term treatment is usually required, which leads to low patient compliance and ultimately disappointing results. Adjuvant of two or more treatment modalities can have synergistic effects and result in superior outcomes over a shorter treatment course with fewer adverse effects.12-15 The previous clinical trials demonstrated that FCO2 laser combined with NBUVB, topical corticosteroid, and 5-fluorouracil were more effective than each of these treatments alone. In addition, evidence suggests that adding PRP to the excimer laser, NB-UVB, or FCO2 laser results in superior improvement and less recurrence rate without a significant increase in complications compared to the excimer laser alone.7-10,13,16-18
Recently, there have been a few studies evaluating the efficacy of triple therapy in refractory cases of vitiligo.15,19,20 Kanokrungsee et al. demonstrated a significantly higher response rate with triple therapy involving FCO2 laser, NBUVB, and topical 0.01% bimatoprost compared to double therapy with laser and NB-UVB in generalized vitiligo.19 Similarly, Li et al. demonstrated a significantly higher response rate (more than 50% repigmentation) with triple therapy of FCO2 laser (every 2 weeks), NB-UVB (twice/thrice a week), and topical betamethasone solution compared to double therapy of FCO2 laser and NB-UVB (44% vs. 8%, respectively) over a 6-month treatment course.20
In this study, we compared the efficacy of the triple combination of FCO2 laser, 308-nm excimer lamp, and PRP with FCO2 laser, 308-nm excimer lamp, and 0.1% tacrolimus ointment on resistant focal patches of vitiligo vulgaris. While both treatment groups showed significant improvement during the course of treatment, the PRP group demonstrated significantly superior outcomes compared to the tacrolimus group. An excellent response rate was observed exclusively in the PRP group.
Abdelghani et al. evaluated the effectiveness of monotherapy with PRP (four sessions every 3 weeks) or FCO2 laser (four sessions every 2 weeks) compared to combined FCO2 laser with either PRP or NB-UVB (twice a week, total number of eight sessions) in non-segmental localized type of vitiligo. They reported excellent-to-good improvement (more than 50% repigmentation) in 30% and 100% of patients in the combined laser and NB-UVB group and combined laser and PRP group, respectively, while only 20% and 10% of patients in the PRP group and laser monotherapy groups showed more than 50% improvement, respectively. Notably, only the combined laser and PRP group demonstrated some degree of repigmentation in acral areas.11 The present study found that the triple combination of FCO2 laser, excimer lamp, and either PRP or topical 0.1% tacrolimus ointment resulted in excellent-to-good results in 56.1% and 26.8% of cases, respectively. The present study enrolled patients with recalcitrant acral lesions, whereas the latter study included patients with vitiligo on all body sites, including the face, neck, and trunk, which typically responds better than acral lesions. Thereby, this can explain the lower response in the present study compared to the aforementioned study.11
In a similar clinical trial, Wen et al. compared the efficacy of the triple combination of FCO2 laser (3 monthly sessions), excimer lamp (twice weekly), and topical tacrolimus for 6 months with a double combination of excimer lamp and topical tacrolimus. Good-to-excellent improvement was observed in 28.5% and 23.8% of patients in triple therapy and double therapy groups, respectively, with no statistically significant difference between the two groups. They concluded that the high molecular weight of tacrolimus, along with the formation of crust and necrosis at the laser site, may all contribute to the low tacrolimus absorption. As a result, no significant increase in effectiveness was reported by adding FCO2 laser to the treatment.21 Similarly, the present study found comparable efficacy with a good-to-excellent response rate of 26.8% in the triple combination of FCO2 laser, excimer lamp, and topical tacrolimus.
To the best of our knowledge, this is the first study to evaluate the efficacy of the triple combination of FCO2 laser, excimer lamp, and PRP on recalcitrant vitiligo lesions in acral areas. This combination demonstrated superior efficacy due to a synergistic effect that stimulates melanocyte proliferation and migration from surrounding peripheral skin and follicular units through the release of growth factors and cytokines. Therefore, this combination is recommended for patients with difficult-to-treat lesions.7-10
The limitations of this clinical trial include short duration of study and follow-up period. In addition, future studies should preferably compare the therapeutic effects of monotherapy with FCO2 laser, PRP, or tacrolimus against combinations of these treatment modalities. Therefore, future research with larger sample sizes is recommended to compare the efficacy of monotherapy with each treatment modality to combination therapy groups over longer treatment courses and follow-up periods.
CONCLUSION
The combination of FCO2 laser, excimer lamp, and PRP demonstrated superior outcomes compared to combined FCO2 laser, excimer lamp, and topical tacrolimus. Furthermore, the PRP group shows superior improvement in resistant acral lesions compared to the tacrolimus group. Thus, for the treatment of recalcitrant vitiligo lesions, a triple combination of FCO2 laser, excimer lamp, and PRP can be recommended.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. Maryam Khalili, Dr. Saleh Solhjou, Dr. Rezvan Amiri, Dr. Mohammad Rezaei Zadeh Rukerd and Dr. Mahin Aflatoonian. The first draft of the manuscript was written by Dr. Mahin Aflatoonian and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical approval
The research/study approved by the Institutional ethical committee of Kerman Medical Sciences, IR.KMU. AH.REC.1399.165 and registered in the Iranian clinical trial registry system with registry code IRCT20210125050139N1 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Prevalence of metabolic syndrome in vitiligo patients in comparison with the control group. Hormozgan Med J. 2022;26:141-4.
- [CrossRef] [Google Scholar]
- Evaluation of quality of life in parents of the patients with vitiligo by Persian version of the family dermatology life quality index (FDLQI) in Kerman. J Pak Assoc Dermatol. 2019;29:196-202.
- [Google Scholar]
- Epidemiological aspects and disease association of childhood vitiligo. J Pak Assoc Dermatol. 2015;25:105-10.
- [Google Scholar]
- Efficacy and safety of traditional and surgical treatment modalities in segmental vitiligo: A review article. J Cosmet Dermatol. 2022;21:2360-73.
- [CrossRef] [Google Scholar]
- Treatment protocols and efficacy of combined laser with medical treatment modalities in vitiligo. J Cosmet Dermatol. 2022;21:3272-91.
- [CrossRef] [Google Scholar]
- Efficacy of combination therapy of pimecrolimus 1% cream and mometasone cream with either agent alone in the treatment of childhood vitiligo. J Pak Assoc Dermatol. 2018;28:507-13.
- [Google Scholar]
- Meta-analysis of the efficacy of adding platelet-rich plasma to 308-nm excimer laser for patients with vitiligo. J Int Med Res. 2022;50:3000605221119646.
- [CrossRef] [Google Scholar]
- The effect of platelet-rich plasma on the outcome of short-term narrowband-ultraviolet B phototherapy in the treatment of vitiligo: A pilot study. J Cosmet Dermatol. 2016;15:108-16.
- [CrossRef] [Google Scholar]
- Platelet-rich plasma versus combined fractional carbon dioxide laser with platelet-rich plasma in the treatment of vitiligo: A comparative study. Clin Cosmet Investig Dermatol. 2018;11:551-9.
- [CrossRef] [Google Scholar]
- Evaluation of combined excimer laser and platelet-rich plasma for the treatment of nonsegmental vitiligo: A prospective comparative study. J Cosmet Dermatol. 2020;19:869-77.
- [CrossRef] [Google Scholar]
- Combined treatment with fractional carbon dioxide laser, autologous platelet-rich plasma, and narrow band ultraviolet B for vitiligo in different body sites: A prospective, randomized comparative trial. J Cosmet Dermatol. 2018;17:365-72.
- [CrossRef] [Google Scholar]
- Efficacy of combination therapy with fractional carbon dioxide laser and ultraviolet B phototherapy for vitiligo: A systematic review and meta-analysis. Aesthet Surg J. 2020;40:NP46-50.
- [CrossRef] [Google Scholar]
- New approach in the treatment of refractory vitiligo: CO2 laser combined with betamethasone and salicylic acid solution. Dermatol Ther. 2017;30(1):e12410.
- [CrossRef] [Google Scholar]
- Fractional laser for vitiligo treated by 10,600 nm ablative fractional carbon dioxide laser followed by sun exposure. Lasers Surg Med. 2014;46:443-8.
- [CrossRef] [Google Scholar]
- Combination of carboxytherapy with narrowband-ultraviolet B in the treatment of recalcitrant areas of vitiligo: A randomized clinical trial. Dermatol Ther. 2022;35:e15229.
- [CrossRef] [Google Scholar]
- Carbon dioxide laser plus topical 5-fluorouracil: A new combination therapeutic modality for acral vitiligo. J Cosmet Laser Ther. 2015;17:216-23.
- [CrossRef] [Google Scholar]
- The efficacy of fractional carbon dioxide laser combined with narrow-band ultraviolet B phototherapy for non-segmental vitiligo: A systematic review and meta-analysis. Lasers Med Sci. 2021;36:165-73.
- [CrossRef] [Google Scholar]
- A comparative study to evaluate the efficacy of fractional CO2 laser+ PRP vs. fractional CO2 laser alone in patients with vitiligo. J Cutan Aesthet Surg. 2023;16:186-91.
- [CrossRef] [Google Scholar]
- Triple combination therapy of narrowband ultraviolet B, fractional carbon dioxide laser and topical bimatoprost 0.01% for non-segmental vitiligo on non-facial areas: A randomized half-body, double-blind, placebo-controlled, comparative study. Dermatol Ther. 2022;35:e15198.
- [CrossRef] [Google Scholar]
- Triple combination treatment with fractional CO2 laser plus topical betamethasone solution and narrowband ultraviolet B for refractory vitiligo: A prospective, randomized half-body, comparative study. Dermatol Ther. 2015;28:131-4.
- [CrossRef] [Google Scholar]
- A preliminary study of fractional CO2 laser added to topical tacrolimus combined with 308 nm excimer lamp for refractory vitiligo. Dermatol Ther. 2019;32:e12747.
- [CrossRef] [Google Scholar]






