Translate this page into:
Use of ionized plasma jet therapy in the treatment of xanthelasma palpebrarum
*Corresponding author: Ajay Dodeja, Department of Dermatology, Venereology and Leprosy, N.K.P. Salve Institute of Medical Sciences and Research Centre and Lata Mangeshkar Hospital, Nagpur, Maharashtra, India. ajaydodeja1995@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thobde M, Borkar M, Oke MA, Dodeja A. Use of ionized plasma jet therapy in the treatment of xanthelasma palpebrarum. J Cutan Aesthet Surg. doi: 10.25259/JCAS_32_2024
Abstract
Objectives:
To evaluate the safety and efficacy of ionized plasma therapy for the treatment of xanthelasma palpebrarum.
Material and Methods:
A total of 35 patients were enrolled for the study. Patients were screened as per the predefined inclusion and exclusion criteria. The patients were treated with ionized plasma jet therapy (IPJT) plasma machines. Pre- and post-sizes of the xanthelasma lesions were noted along with the side effects, and the patients were followed up for a period of 90 days.
Results:
The complete resolution of the xanthelasma lesion was observed in 28 out of 35 patients, with two patients requiring two sessions, five patients developing hypopigmentation, and 1 patient having hyperpigmentation as a side effect, which was resolved after 4 weeks.
Conclusions:
Based on the results, ionized plasma therapy for xanthelasma palpebrarum can be recommended as a safe and effective option.
Keywords
Xanthelasma palpebrarum
Ionized plasma therapy
Jet plasma therapy
Xanthomas
INTRODUCTION
Xanthelasma palpebrarum is a condition characterized by yellowish deposits of fat underneath the skin on or around the eyelids. These deposits are typically soft and appear as flat, slightly raised patches, majorly caused due to lipid accumulation.1 Xanthelasma is usually asymptomatic, and its characteristic features can be noted as soft plaques, macules, or papules of yellowish color. Most seen in middle-aged and older men and women with an incidence rate of 0.3% and 1.1%, respectively.2,3 Although xanthelasmas are asymptomatic, they are esthetically not pleasing. There are multiple treatments available, such as surgical excision, ablative and non-ablative lasers, trichloro-acetic acid peeling, and radiofrequency ablation, but these treatments have their own set of limitations. Ionized plasma therapy is a newer modality for the treatment of xanthelasmas. Plasma is the fourth state of matter. Plasma can be created by heating or subjecting gas to a strong magnetic field. A plasma generator produces a strong microplasma beam due to the ionization of gases present in the air. The energy thus produced is used to treat epidermal areas affected by esthetic blemishes.4
MATERIAL AND METHODS
This is an open-label experimental research study of the patients affected with xanthelasma palpebrarum, who visited the dermatology outpatient department in a tertiary care center. An institutional ethics committee approval was obtained before the initiation of the study.
The inclusion criteria of the patients were as follows:
All adults with no significant medical history
Patients having normal and abnormal lipid profile
Wash-off period of 3 months prior to surgical/non-surgical treatment.
The exclusion criteria for the patients were as follows:
Keloidal tendencies
Pregnant and lactating females
Active infections
Patients with bleeding tendencies or on blood thinners
Concomitant eye diseases
Patients having implants and pacemakers.
An informed written consent was obtained from all the patients to participate in the study. Topical anesthesia was applied to the region affected and left for 45 min. The procedure area was cleaned with betadine and normal saline. An assistant held down the eyelid. Xanthelasmas were superficially ablated using ionized plasma jet therapy (IPJT) device at the intensity of 4–6 in a paintbrush fashion, leaving no skip areas in between, until a layer of thin brown crusts, a superficial layer of the desiccated epidermis was seen [Figures 1 and 2]. The number of passes depended on the size of the lesion. The time taken for the entire procedure was 10–15 min.

- Ionized plasma jet therapy (IPJT) device.
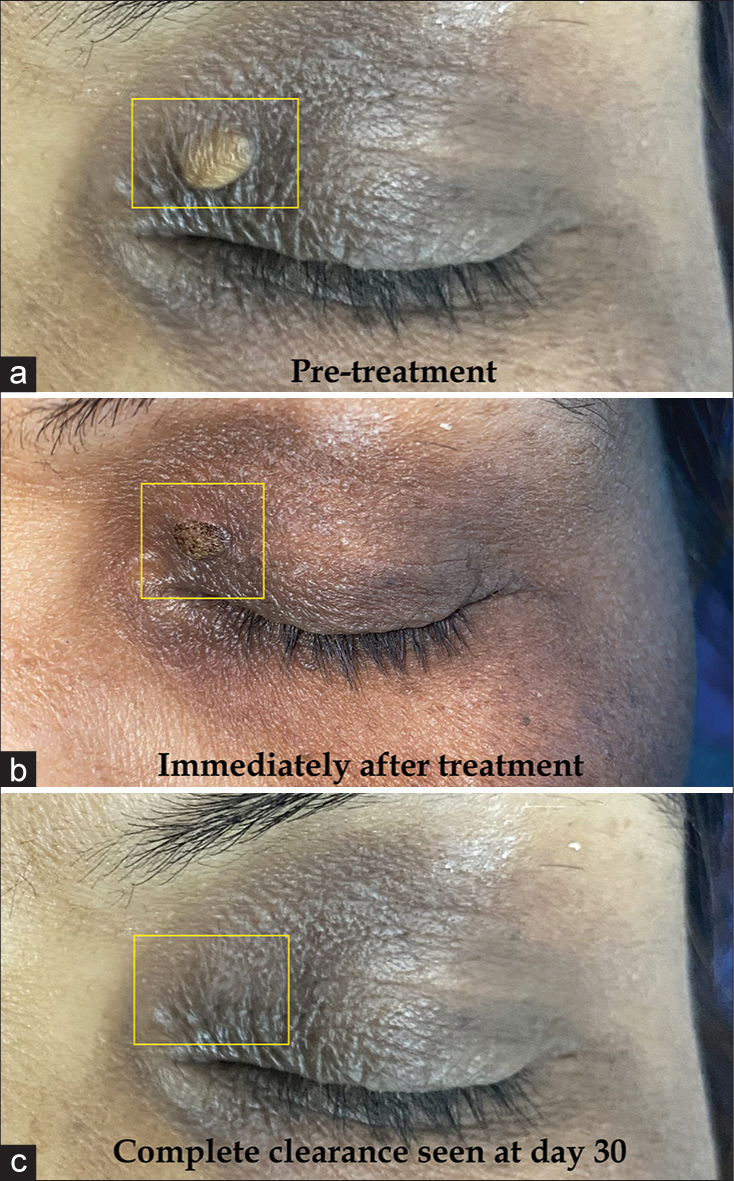
- Superficial ablation of xanthelasma palpebrarum (yellow rectangle) with ionized plasma jet therapy (IPJT) ((a) – Pre-treatment at day 0, (b) – Immediately post-treatment thin crusts seen, (c) – Complete clearance of xanthelasma in a single sitting at day 30).
The patients were evaluated on the following symptoms: Edema, pain, itching, and local hyperemia and the treated area presented hyperpigmentation or hypopigmentation on day 7. The pain was analyzed using a 100 mm Visual Analog Score. At the initial session, the size and number of the lesions were graded numerically. The clinical assessment was done by photographic assessment using a five-pointer scale as mentioned in Table 1.
| Pointer grades | Symptoms resolution |
|---|---|
| 0 | No improvement |
| 1 | Mild (0–25%) |
| 2 | Moderate (26–50%) |
| 3 | Good (51–75%) |
| 4 | Excellent (76–100%) |
Post-procedure topical antibiotic was given. The crust formation healed spontaneously on its own in a period of 7 days. Patients were followed up for a period of 7, 30, and 90 days. A second session was planned at 30 days from the first session if required.
RESULTS
A total of 35 patients with xanthelasma palpebrarum were included in this study, ranging between 40 years and 60 years of age, with no related medical history. None of the patients had any smoking/tobacco/alcohol habits and were vegetarian in dietary habits. All the patients reported to have no significant medical history. The patient profile is mentioned in detail in Table 2. Results were observed after the first session as only 2 patients (5.7%) required the second session, which was Grade 2 and Grade 4 [Figure 3]. Hypopigmentation and hyperpigmentation were reported in 14.3% and 5.7% of patients, respectively [Figure 4].
| Parameter | Mean±Standard Deviation/Number (Frequency %) |
|---|---|
| Age | 47±7.58 years |
| Male | 5 (15) |
| Females | 30 (85) |
| Fitzpatrick skin type 03 | 16 (45.71) |
| Fitzpatrick skin type 04 | 19 (54.27) |
| Improvement pointer grades (0) | 4 (11.43) |
| Improvement pointer grades (1) | 11 (31.43) |
| Improvement pointer grades (2) | 17 (48.57) |
| Improvement pointer grades (3) | 1 (2.86) |
| Improvement pointer grades (4) | 2 (5.71) |
| No follow up data | 4 (11.43) |
| Hyperpigmentation | 2 (5.71) |
| Hypopigmentation | 5 (14.3) |
| Second session required | 2 (5.71) |

- Patient presentation of bilateral xanthelasma palpebrarum lesions requiring two sessions ((a) – Pre-treatment, (b) – After the first session at day 30, c – After the second session at day 90).

- Patient presentation of bilateral xanthelasma palpebrarum lesions developed hypopigmentation ((a) – Pre-treatment, (b) – After 1 session at day 7, (c) – Post-treatment day 90).
An abnormal lipid profile was noted in 6 (17%) out of 35 patients. Out of all the patients who were treated with IPJT with the aforementioned frequencies, 54.3% of patients were extremely satisfied with the results and excellent results in terms of plaque resolution, and esthetic looks were noted in 40% of patients. A detailed table of patient satisfaction is mentioned in Table 3.
| Satisfaction achieved | n(%) |
|---|---|
| Patient satisfaction (0) | 3 (8.57) |
| Patient satisfaction (1) | 5 (14.29) |
| Patient satisfaction (2) | 9 (25.71) |
| Patient satisfaction (3) | 15 (42.86) |
| Patient satisfaction (4) | 3 (8.57) |
| Patient satisfaction (5) | 3 (8.57) |
Good results with no side effects such as edema, erythema, itching, scarring, recurrence, or hematoma were observed in most of the cases. All four grades of xanthelasma were treated effectively. In terms of the procedure being painful, results were noted in 2.8 according to the Visual Analog Scale score.
DISCUSSION
Xanthelasma palpebrarum is a common form of xanthelasma usually characterized by the yellowish deposits of the fat under the skin.5,6 It does not have any fatal health consequences attached, but it has been reported as a marker of different clinical conditions such as hyperlipidemia, atherosclerosis, and cardiovascular diseases.7 Based on research evidence, it might be suggested that similar underlying mechanisms might be involved in the formation of xanthomata and emerging atheromas based on the ground of commonalities observed in the ultrastructural composition of both these plaques.6,8 Although we have mixed evidence regarding xanthelasma and cholesterol levels. Research reports have found that individuals having xanthelasma did not compulsorily become hyperlipidemic.6,9,10 Some of the affected individuals were found to be normolipidemic, as in this case series. We included patients with both normal and abnormal lipid profiles in our study. There are many treatment approaches for xanthelasmas but still, there is disagreement over the best ones in terms of effectiveness and adverse effects.11,12
Plasma therapy, which is based on ionized gas, has been newly recommended and widely accepted for the treatment of xanthelasma palpebrarum. The device generates spark discharge and plasma using direct current high voltage (5 kV), with a maximal current of 1 mA. The energy is absorbed by the positive and negative electrons present in the free air. A 2 mm distance is maintained between the skin and the tip of the device for free air. The air is ionized, and it becomes plasma which initially causes cell dehydration followed by necrosis. This process transforms solid tissue into a gaseous state and creates mild coagulation, causing the contraction of local epidermal and dermal skin, which results in increased collagenosis, as histopathologically xanthelasmas affect only up to the superficial reticular dermis.10,13 A spark of 1 mm2 allows precise and controlled thermal damage, which in turn causes less injury to the surrounding skin. Results from some research studies using this therapy have been listed in Table 4.14-17
Apart from the use of jet plasma in the treatment of xanthelasma, it has been utilized for the treatment of benign vascular lesions such as angioma (hemangioma and nevus capillaries), telangiectasia, and cutaneous lesions, which include keratosis (verruca seborrheic and keratosis seborrheic), fibroma, and blepharoplasty.18
CONCLUSION
Plasma therapy is an effective and painless treatment option with fewer side effects, such as hypopigmentation, which can be resolved over follow-up visits. Based on the results of this study, controlled tissue destruction, immediate results with minimal downtime, and lower recurrence rates make it safe for use in sensitive areas around the eye. This noninvasive surgical device can be used for other dermatological conditions such as seborrheic keratosis, dermatosis papulosa nigra, fibroma, etc. More studies are needed on this, but the clinical experience to date is excellent.
Authors’ contributions
Mallika Thobde: Concepts, design, definition of intellectual content, literature research, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing, manuscript review, guarantor. Milind Borkar: Concepts, design, definition of intellectual content, manuscript preparation, manuscript review, guarantor. Manjiri Abhijit Oke: Literature research, clinical studies, experimental studies, data acquisition, data analysis, statistical analysis. Ajay Dodeja: Data analysis, statistical analysis, manuscript preparation, manuscript editing, manuscript review, guarantor.
Ethical approval
The research/study approved by the Institutional Review Board at N.K.P Salve Institute of Medical Sciences and Research Centre and Lata Mangeshkar Hospital, number 2/2023, dated February 23, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Xanthelasma: An update on treatment modalities. J Cutan Aesthet Surg. 2018;11:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Skin manifestations associated with systemic diseases-Part II. An Bras Dermatol. 2021;96:672-87.
- [CrossRef] [PubMed] [Google Scholar]
- Xanthelasma palpebrarum-a brief review. Clin Cosmet Investig Dermatol. 2017;11:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Xanthelasma palpebrarum and its relation to atherosclerotic risk factors and lipoprotein (a) Int J Dermatol. 2008;47:785-9.
- [CrossRef] [PubMed] [Google Scholar]
- The pathogenesis and clinical significance of xanthelasma palpebrarum. J Am Acad Dermatol. 1994;30:236-42.
- [CrossRef] [PubMed] [Google Scholar]
- Xanthelasma palpebrarum: More than meets the eye. Indian J Otolaryngol Head Neck Surg. 2019;71:439-46.
- [CrossRef] [PubMed] [Google Scholar]
- Risk of non-alcoholic fatty liver disease in xanthelasma palpebrarum. J Inflamm Res. 2021;14:1891-9.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of cholesterolester fatty acid patterns in the blood and in evolving xanthoma and atheroma during cholesterol-feeding of rabbits. J Invest Dermatol. 1966;47:253-9.
- [CrossRef] [PubMed] [Google Scholar]
- Normolipidemic xanthelasma palpebrarum: Lipid composition, cholesterol metabolism in monocyte-derived macrophages, and plasma lipid peroxidation. Acta Derm Venereol. 1996;76:107-10.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma sublimation for the treatment of xanthelasma palpebrarum. Acta Dermatovenerol Alp Pannonica Adriat. 2020;29:55-7.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of surgical management of xanthelasma palpebrarum. Arch Plast Surg. 2013;40:380-6.
- [CrossRef] [PubMed] [Google Scholar]
- Disappearance of eyelid xanthelasma following oral simvastatin (Zocor) Br J Ophthalmol. 2005;89:639-40.
- [CrossRef] [PubMed] [Google Scholar]
- Xanthelasma palpebrarum In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531501 [last accessed on 2024 May 28]
- [Google Scholar]
- Treatment of xanthelasma with fractional plasma. Esperienze Dermatol. 2021;23:1-6.
- [CrossRef] [Google Scholar]
- Long-wave plasma radiofrequency ablation for treatment of xanthelasma palpebrarum. J Cosmet Dermatol. 2019;18:121-3.
- [CrossRef] [PubMed] [Google Scholar]
- Successful cosmetic ablation of xanthelasma palpebrarum with low-voltage radiofrequency: Back to the basics! Dermatol Surg. 2014;40:1443-4.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of low-voltage radiofrequency in the treatment of xanthelasma palpebrarum: A pilot study of 15 cases. Dermatol Surg. 2010;36:1973-8.
- [CrossRef] [PubMed] [Google Scholar]
- Focus on plasma: The application of plasma devices in aesthetic medicine. PMFA J. 2017;4:24-6.
- [Google Scholar]







